Effects of different admission modes on reperfusion time and risk factors of in-hospital death in patients with acute ST-segment elevation myocardial infarction
-
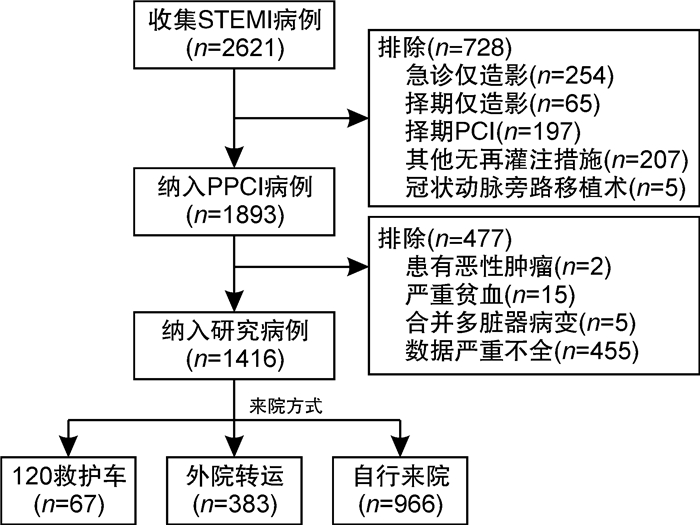
摘要: 目的 探讨胸痛中心(CPC)模式下不同来院方式对急性ST段抬高型心肌梗死(STEMI)患者再灌注时间及院内不良事件发生的影响。方法 根据来院方式不同将1416例接受直接经皮冠状动脉介入治疗(PPCI)的STEMI患者分为120现场接送组(67例)、外院转运组(383例)和自行来院组(966例)。比较各组患者的临床特征及再灌注时间,并对不同来院方式患者的院内不良事件(急性左心衰、院内死亡)发生情况进行回归分析。结果 所有患者平均年龄为(61.57±11.08)岁,发病-首次医疗接触(S2FMC)中位时间为160.0(79.8,338.5) min、发病-球囊开通(S2B)中位时间为258.0(168.0,457.0) min,3组比较,通过120救护车来院患者的上述过程时间较外院转运和自行来院组短(均P < 0.01)。所有患者肌钙蛋白抽血-出结果中位时间为17.0(15.0,19.0) min、知情同意开始-签署完成中位时间为4.0(2.0,6.0) min,3组比较,自行来院组患者的上述过程用时均较外院转运组长(均P < 0.01)。所有患者的大门-球囊开通(D2B)中位时间为52.0(44.0,63.0) min,不同来院方式的患者D2B时间基本相同(P=0.493),D2B时间>90 min的比例在各组间无显著统计学差异(P=0.631)。多因素logistic回归分析显示,调整性别、年龄、糖尿病史、高血压史、Killip分级、入院时收缩压后,外院转运(OR:3.50,95%CI:1.95~6.31,P < 0.001)和自行来院(OR:11.62,95%CI:6.53~20.68,P < 0.001)的患者较120救护车现场接送的患者更易出现S2FMC时间≥90 min。120救护车现场接送组、外院转运组和自行来院组患者院内死亡发生率分别为4.5%、1.3%、0.9%(P=0.035),急性左心衰发生率分别为3.0%、5.7%、4.7%(P=0.538)。调整性别、年龄、Killip分级、入院时收缩压、吸烟史、病变血管数后,不同来院方式的STEMI患者院内死亡发生率差异无统计学意义(P>0.05)。结论 不同来院方式STEMI患者院内死亡发生率无显著差异,但通过120救护车现场接送入院的STEMI患者的总缺血时间最短。为改善和提高我国急性胸痛患者的预后,仍需不断优化和改进STEMI救治流程,进一步缩短患者从症状发生到再灌注治疗的时间。Abstract: Objective To assess the effect of different admission modes on reperfusion time and the related risk factors of nosocomial adverse events of patients with acute ST-elevation myocardial infarction(STEMI) under the chest pain center(CPC) model.Methods 1416 cases STEMI patients receiving PPCI were divided into 120 on-site transfer group(67 cases), transfer group(383 cases), and self-admission group(966 cases) according to different admission modes to the hospital. The clinical characteristics and reperfusion time of patients in each group were compared, and the incidence of nosocomial adverse events(acute left heart failure, nosocomial death) in patients with different admission modes were analyzed by regression.Results The mean age of all patients was(61.57±11.08) years, the median time of S2FMC was 160.0(79.8, 338.5) min, the median time of S2B was 258.0(168.0, 457.0) min. Compared with the three groups, the above process time of patients who came to the hospital by 120 ambulance was shorter than that of patients who came to the hospital by themselves(P < 0.01). The time from blood drawing to the result of troponin was 17.0(15.0, 19.0) min, and the time from the beginning of informed consent to the completion of informed consent was 4.0(2.0, 6.0) min. Compared with the three groups, the patients in the self-admission group had the longest time in the above process(all P < 0.01). The D2B time of all patients was 52.0(44.0, 63.0) min, and the D2B time of patients with different transfer pathways was the same(P=0.493). The ratio of D2B>90 min was the same among all groups(P=0.631). After adjusting for sex, age, diabetes, hypertension, Killip grade, systolic blood pressure, referral to the hospital(OR: 3.50, 95%CI: 1.95-6.31, P < 0.001) and self-admission(OR: 11.62, 95%CI: 6.53-20.68, P < 0.001) patients were more likely to develop S2FMC time ≥90 min than patients admitted by 120 ambulances. The incidence of acute left heart failure was 3.0% in the 120 ambulance group, 5.7% in the transfer group, and 4.7% in the self-admission group(P=0.538), and the incidence of in-hospital death was 4.5%, 1.3%, and 0.9%(P=0.035), respectively. After adjusting gender, age, Killip grade, systolic blood pressure, smoking, and number of pathological vessels, there was no significant difference in the incidence of in-hospital death among STEMI patients with different admission methods(all P>0.05).Conclusion There was no significant difference in the incidence of in-hospital death among STEMI patients with different admission modes, and the total ischemic time of STEMI patients admitted by 120 ambulance was the shortest. To improve the prognosis of patients with acute chest pain in China, it is necessary to continuously optimize the STEMI treatment process and further shorten the time from symptom occurrence to reperfusion therapy.
-
Key words:
- myocardial infarction /
- admission modes /
- reperfusion time /
- in-hospital death
-

-
表 1 STEMI患者基本特征
Table 1. Baseline characteristics of participants with STEMI
例(%), X±S 变量 总体(1416例) 120救护车(67例) 外院转运(383例) 自行来院(966例) 统计量 P值 年龄/岁 61.57±11.08 60.63±11.20 61.63±12.05 61.61±10.67 0.253 0.776 男性 1071(75.6) 50(74.6) 287(74.9) 734(76.6) 0.203 0.904 吸烟 829(58.5) 35(52.2) 228(59.5) 566(58.6) 1.252 0.535 饮酒 370(26.1) 17(25.4) 99(25.8) 254(26.3) 0.049 0.976 既往史 高血压 806(56.9) 42(62.7) 199(52.0) 565(58.5) 5.723 0.057 糖尿病 307(21.7) 16(23.9) 75(19.6) 216(22.4) 1.447 0.485 血脂异常 49(3.4) 1(1.5) 11(2.9) 37(3.8) 1.785 0.410 卒中/短暂性脑缺血发作 80(5.6) 5(7.5) 19(5.0) 56(5.8) 0.771 0.680 冠心病 23(1.6) 1(1.5) 6(1.6) 16(1.7) 0.022 0.998 Killip分级* 1.698 0.428 Ⅰ级 1331(94.0) 59(88.1) 352(91.9) 920(95.2) Ⅱ级 74(5.2) 5(7.5) 28(7.3) 41(4.2) Ⅲ级 7(0.5) 1(1.5) 3(0.8) 3(0.3) Ⅳ级 4(0.3) 2(3.0) 0(0) 2(0.2) 收缩压/mmHg 136.55±25.46 128.27±23.32 133.94±24.47 138.16±25.821)2) 7.570 0.001 舒张压/mmHg 82.76±15.62 81.57±14.79 82.33±16.02 83.02±15.52 0.474 0.623 心率/(次·min-1) 74.36±17.04 72.24±20.19 75.78±17.90 73.95±16.43 2.123 0.120 实验室指标 血肌酐/(μmol·L-1) 75.00±38.93 69.13±17.34 73.69±28.90 75.93±43.21 1.252 0.286 谷丙转氨酶/(U·L-1) 47.67±79.41 39.50±23.57 44.61±31.76 49.46±93.86 0.877 0.416 谷草转氨酶/(U·L-1) 162.47±170.60 137.45±122.88 161.75±146.08 164.50±182.26 0.780 0.459 总胆固醇/(mmol·L-1) 4.46±1.00 4.44±1.01 4.39±1.07 4.49±0.97 1.294 0.274 甘油三酯/(mmol·L-1) 1.54±1.17 1.47±0.80 1.52±1.04 1.55±1.24 0.157 0.855 高密度脂蛋白胆固醇/(mmol·L-1) 1.02±0.24 1.03±0.23 1.01±0.25 1.03±0.24 0.365 0.694 低密度脂蛋白胆固醇/(mmol·L-1) 2.88±0.87 2.87±0.86 2.83±0.94 2.91±0.84 1.199 0.302 病变血管数 5.474 0.485 单支 402(28.4) 21(31.3) 120(31.3) 261(27.0) 双支 442(31.2) 17(25.4) 114(29.8) 311(32.2) 3支 517(36.5) 24(35.8) 136(35.5) 357(37.0) 4支 55(3.9) 5(7.5) 13(3.4) 37(3.8) 罪犯病变血管 2.672 0.849 前降支 632(44.6) 31(46.3) 171(44.6) 430(44.5) 回旋支 150(10.6) 5(7.5) 38(9.9) 107(11.1) 左主干 14(1.0) 1(1.5) 2(0.5) 11(1.1) 右冠脉 620(43.8) 30(44.8) 172(44.9) 418(43.3) 意识 6.323 0.176 清醒 1409(99.5) 67(100.0) 378(98.7) 964(99.8) 模糊/呼之有反应 3(0.2) 0(0) 2(0.5) 1(0.1) 昏迷/丧失 4(0.3) 0(0) 3(0.8) 1(0.1) 住院天数/d 8.85±3.80 9.09±6.17 8.58±2.81 8.93±3.93 1.303 0.272 总费用/万元 4.65±2.69 6.37±8.59 4.66±1.571) 4.53±2.091) 14.945 0.001 注:*采用Ridit分析方法。与120救护车组比较,1)P < 0.05;与外院转运组比较,2)P < 0.05。 表 2 不同来院方式患者再灌注时间比较
Table 2. Comparison of reperfusion time in STEMI patients with different admission modes
M(P25, P75), 例(%) 再灌注相关时间 总体(1416例) 120救护车(67例) 外院转运(383例) 自行来院(966例) 统计量 P值 S2FMC/min 160.0(79.8,338.5) 50.0(30.0,110.0) 102.0(54.5,208.0)1) 200.0(112.0,426.0)1) 9.620 < 0.001 肌钙蛋白抽血-出结果/min 17.0(15.0,19.0) 16.0(14.0,18.0) 16.0(14.0,18.0) 17.0(15.0,19.0)2) 20.545 0.001 大门-导管室激活时间/min 24.0(18.0,33.0) 24.0(18.0,32.3) 21.0(16.0,29.0) 25.0(19.7,34.0) 0.088 0.916 知情同意开始-签署完成/min 4.0(2.0,6.0) 4.0(2.0,5.0) 3.0(1.0,5.0)1) 4.0(2.0,6.0)2) 25.982 0.001 开始穿刺-手术结束时间/min 29.0(22.0,37.0) 30.0(22.0,45.0) 28.0(21.0,36.0) 29.0(22.0,37.0) 5.037 0.081 D2B/min 52.0(44.0,63.0) 47.5(42.0,60.0) 47.5(42.0,60.0) 47.5(42.0,60.0) 0.707 0.493 S2B/min 258.0(168.0,457.0) 128.0(110.0,180.0) 268.0(187.0,420.5)1) 262.0(170.0,493.0)1) 24.045 0.001 D2B>90 min 60(4.2) 3(4.5) 13(3.4) 44(4.6) 0.920 0.631 注:与120救护车组比较,1)P < 0.05;与外院转运组比较,2)P < 0.05 表 3 S2FMC时间≥90 min的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of S2FMC time≥90 min
项目 OR 95%CI P 性别 1.37 1.00~1.89 0.053 年龄 1.02 1.01~1.03 0.002 糖尿病史 1.08 0.79~1.47 0.649 高血压史 0.98 0.76~1.27 0.896 Killip分级 1.17 0.77~1.76 0.463 入院收缩压 1.01 1.00~1.01 0.007 来院方式 120救护车 Ref. — — 外院转运 3.50 1.95~6.31 < 0.001 自行来院 11.62 6.53~20.68 < 0.001 表 4 不同来院方式STEMI患者不良事件发生情况分析
Table 4. Analysis of adverse events in STEMI patients with different admission modes
例(%) 不良事件 总体(1416例) 120救护车(67例) 外院转运(383例) 自行来院(966例) 统计量 P值 院内死亡 17(1.2) 3(4.5) 5(1.3) 9(0.9) 6.690 0.035 急性左心衰 69(4.9) 2(3.0) 22(5.7) 45(4.7) 1.238 0.538 表 5 STEMI患者院内死亡发生危险因素的多因素logistic回归分析
Table 5. Multivariate logistic regression analysis of risk factors for in-hospital death in STEMI patients
因素 OR 95%CI P 性别 1.57 0.46~5.38 0.477 年龄 1.06 1.00~1.13 0.041 Killip分级 7.97 3.89~16.34 0.001 收缩压 0.98 0.96~1.00 0.061 吸烟 2.40 0.70~8.26 0.167 病变血管数 0.77 0.741~1.46 0.426 来院方式 120救护车 Ref. — — 外院转运 1.47 0.20~10.89 0.709 自行来院 1.19 0.34~3.95 0.777 -
[1] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2020概要[J]. 中国循环杂志, 2021, 36(6): 521-545. doi: 10.3969/j.issn.1000-3614.2021.06.001
[2] Lambert L, Brown K, Segal E, et al. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction[J]. JAMA, 2010, 303(21): 2148-2155. doi: 10.1001/jama.2010.712
[3] 中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 等. ST段抬高型心肌梗死基层诊疗指南(实践版·2019)[J]. 中华全科医师杂志, 2020, 19(12): 1092-1099. doi: 10.3760/cma.j.cn114798-20200904-00962
[4] 林捷, 颜彦, 施鸿毓. 胸痛中心建设对急性心梗救治效率及预后影响的研究[J]. 临床急诊杂志, 2019, 20(10): 767-770. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201910005.htm
[5] 麦合甫热提·乌甫尔, 袁玉娟, 冯彦玲, 等. 急性心肌梗死冠脉血内皮细胞微粒研究[J]. 临床急诊杂志, 2021, 22(6): 421-425. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202106013.htm
[6] 尼菲拉·甫拉提, 菲尔凯提·玉山江, 袁玉娟, 等. 急性冠状动脉综合征患者外周血内皮细胞及红细胞微粒水平分析[J]. 临床心血管病杂志, 2020, 36(5): 459-463. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202005013.htm
[7] 陈国钦, 张稳柱, 李健豪, 等. 胸痛中心模式下不同到院方式对急性ST段抬高型心肌梗死患者再灌注时间的影响[J]. 中国循环杂志, 2017, 32(9): 859-863. doi: 10.3969/j.issn.1000-3614.2017.09.007
[8] Yudi MB, Ramchand J, Farouque O, et al. Impact of door-to-balloon time on long-term mortality in high-and low-risk patients with ST-elevation myocardial infarction[J]. Int J Cardiol, 2016, 224: 72-78. doi: 10.1016/j.ijcard.2016.09.003
[9] 易绍东, 向定成, 段天兵, 等. 建立胸痛中心对不同来院方式ST段抬高急性心肌梗死患者进门-球囊时间的影响[J]. 中国介入心脏病学杂志, 2014, 22(9): 549-552. doi: 10.3969/j.issn.1004-8812.2014.09.002
[10] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南[J]. 中华心血管病杂志, 2015, 43(5): 380-393. doi: 10.3760/cma.j.issn.0253-3758.2015.05.003
[11] 刘璇, 李树仁, 杨国慧. 胸痛中心模式下急性ST段抬高型心肌梗死救治现状研究[J]. 临床心血管病杂志, 2019, 35(05): 420-424. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201905008.htm
[12] 陈盼盼, 董淑娟, 李静超, 等. "门-字"时间延误程度及其影响因素分析[J]. 中华急诊医学杂志, 2019, 28(5): 596-603. doi: 10.3760/cma.j.issn.1671-0282.2019.05.013
[13] Barbagelata A, Perna ER, Clemmensen P, et al. Time to reperfusion in acute myocardial infarction. It is time to reduce it![J]. J Electrocardiol. 2007 Jul; 40(3): 257-264.
[14] 胡大一, 丁荣晶. "胸痛中心"建设中国专家共识[J]. 中华危重症医学杂志(电子版), 2011, 4(6): 381-393. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWZD201106009.htm
[15] 林全洪, 许向东, 张云柯, 王飞, 顾建华, 徐耀伟, 朱仰阁, 李君. 不同来院方式急性ST段抬高心肌梗死患者再灌注时间与结果影响因素分析[J]. 中华急诊医学杂志, 2020, 29(7): 921-928. doi: 10.3760/cma.j.issn.1671-0282.2020.07.006
[16] Zhang Q, Zhang RY, Qiu JP, et al. Prospective multicenter randomized trial comparing physician versus patient transfer for primary percutaneous coronary intervention in acute ST-segment elevation myocardial infarction[J]. Chin Med J(Engl), 2008, 121(6): 485-491.
[17] Zhang Q, Zhang RY, Qiu JP, et al. Impact of different clinical pathways on outcomes of patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: the RAPID-AMI study[J]. Chin Med J(Engl), 2009, 122(6): 636-642.
-




 下载:
下载: