Correlation between epicardial fat thickness and heart failure with preserved ejection fraction
-
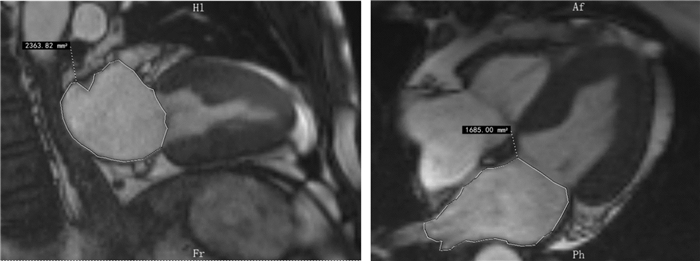
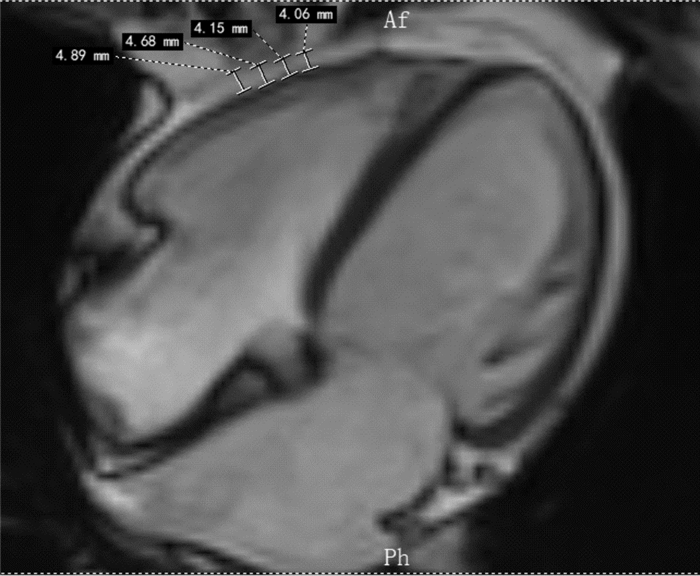
摘要: 目的 探讨心外膜脂肪组织(EAT)厚度与射血分数保留性心力衰竭(HFpEF)发生风险的相关性。方法 选取2019年8月—2020年8月于郑州大学第一附属医院住院治疗,且接受常规心脏磁共振检查的HFpEF患者147例,其中男66例,女81例作为HFpEF组,另选取33例患者作为正常对照组。于心脏磁共振长轴四腔心平面测量右室游离璧及左、右房室沟心外膜脂肪厚度(EFT),同时收集其余相关指标及一般基线资料。结果 HFpEF组较对照组心房颤动、高血压、高脂血症、冠心病、肥厚型心肌病患病率及NT-proBNP、肌钙蛋白Ⅰ、糖化血红蛋白明显升高,差异有统计学意义(P<0.05)。HFpEF患者右室游离璧及左、右房室沟EFT、左心房容积指数、三尖瓣反流速度均高于对照组,差异有统计学意义(P<0.05)。多因素logistic回归分析结果显示,NT-proBNP(β=0.092,OR=1.097,95%CI:1.036~1.161,P=0.002)、左室后壁厚度(β=2.177,OR=8.309,95%CI:1.669~41.376,P=0.010)、右室游离璧EFT(β=1.900,OR=6.683,95%CI:1.034~43.199,P=0.046)是HFpEF患者的独立危险因素(P<0.05)。结论 HFpEF的患者EFT较对照组明显增厚,右室游离璧EFT是HFpEF的发生的独立危险因素。Abstract: Objective To research the correlation between the thickness of epicardial adipose tissue(EAT) and the risk of heart failure with preserved ejection fraction(HFpEF, LVEF ≥ 50%).Methods The 147 patients with HFpEF who were hospitalized and underwent routine cardiac magnetic resonance examinations were selected in the First Affiliated Hospital of Zhengzhou University from August 2019 to August 2020. Of which 66 were males and 81 were females as HFpEF group, another 33 patients were selected as the normal control group. The right ventricular free wall EAT and left and right atrioventricular groove EAT were measured on the long-axis four-chamber heart plane of cardiac magnetic resonance. At the same time, other related indexes and general baseline data were collected.Results Compared with the control group, the prevalence of atrial fibrillation, hypertension, hyperlipidemia, coronary heart disease, hypertrophic cardiomyopathy, NT-proBNP, troponin I, and glycosylated hemoglobin were significantly higher in the HFpEF group. The difference was statistically significant(P< 0.05). The right ventricular free wall EFT, left and right atrioventricular groove EFT, left atrial volume index, and tricuspid regurgitation velocity of HFpEF patients were higher than those of the control group, and the difference was statistically significant(P< 0.05). Multivariate logistic regression analysis showed that NT-proBNP(β=0.092,OR=1.097, 95%CI: 1.036-1.161,P=0.002), left ventricular posterior wall thickness(β=2.177,OR=8.309, 95%CI: 1.669-41.376,P=0.010) and right ventricular free wall EFT(β=1.900,OR=6.683, 95%CI: 1.034-43.199,P=0.046) were independent risk factors in patients with HFpEF(P< 0.05).Conclusion The EFT of patients with HFpEF is significantly thicker than that of the control group, and the EFT of right ventricular free wall is an independent risk factor for the occurrence of HFpEF.
-

-
表 1 HFpEF组和对照组临床资料比较
Table 1. General data
X±S, M(P25, P75) 项目 HFpEF组(147例) 对照组(33例) P 年龄/岁 53.2±14.1 50.5±14.1 0.323 男/例(%) 66(36.3) 17(51.5) 0.491 体表面积/m2 1.80±0.19 1.83±0.19 0.380 BMI/(kg·m-2) 25.1±3.7 25.2±3.7 0.882 体重/kg 71±13 73±13 0.490 心率/(次·min-1) 77±13 80±11 0.218 收缩压/mmHg 129(118,141) 123(114,133) 0.118 舒张压/mmHg 78(69,85) 77(71,88) 0.839 合并症 肥厚型心肌病/例(%) 30(20.4) 0(0) 0.002 室性心律失常/例(%) 29(19.7) 2(6.1) 0.074 室上性心动过速/例(%) 12(9.8) 0(0) 0.127 房室传导阻滞/例(%) 11(7.5) 0(0) 0.220 房颤/例(%) 22(15.0) 0(0) 0.016 高血压/例(%) 64(43.5) 6(12.0) 0.007 高脂血症/例(%) 47(32.0) 1(3.0) 0.001 冠心病/例(%) 60(40.8) 7(21.2) 0.035 糖尿病/例(%) 21(14.3) 1(3.0) 0.084 脑梗死/例(%) 11(7.5) 2(6.1) 1.0 睡眠呼吸暂停综合征/例(%) 4(2.7) 0(0) 1.0 抑郁状态/例(%) 12(8.2) 1(3.0) 0.468 NYHA分级 心功能Ⅱ级/例(%) 123(83.7) 0(0) 心功能Ⅲ级/例(%) 20(13.6) 0(0) 心功能Ⅳ级/例(%) 4(2.7) 0(0) NT-proBNP/(ng·L-1) 316(170,766) 36(19,60) <0.001 肌钙蛋白Ⅰ/(μg·L-1) 0.012(0.010,0.019) 0.010(0.004,0.012) <0.001 糖化血红蛋白/% 5.9(5.6,6.3) 5.6(5.5,6.0) 0.004 C-反应蛋白/(mg·L-1) 1.9(0.81,3.70) 1.70(0.47,2.50) 0.042 肌酸激酶同工酶/(U·L-1) 13(9,18) 13(10,23) 0.366 肾小球滤过率/[mL·min-1·(1.73 m2)-1] 99(87,107) 104(97,117) 0.028 白细胞/(×109·L-1) 6.0(5.1,7.6) 6.5(5.5,8.1) 0.399 血红蛋白/(g·L-1) 134(118,147) 137(131,152) 0.030 尿酸/(μmol·L-1) 298(245,380) 299(263,369) 0.972 总胆固醇/(mmol·L-1) 3.71(3.16,4.55) 4.03(3.26,4.89) 0.213 甘油三酯/(mmol·L-1) 1.16(0.82,1.65) 1.29(0.83,1.94) 0.405 高密度脂蛋白/(mmol·L-1) 1.12(0.89,1.37) 1.17(1.00,1.42) 0.237 低密度脂蛋白/(mmol·L-1) 2.06(1.72,2.73) 2.29(1.83,3.16) 0.180 表 2 心脏超声及心脏磁共振成像特点
Table 2. Cardiac ultrasound and cardiac magnetic resonance imaging features
X±S, M(P25, P75) 项目 HFpEF组(147例) 对照组(33例) P 心脏超声 E/A 0.8(0.7,1.3) 1.1(0.8,1.4) 0.017 LAD/mm 35(32,39) 30(29,34) <0.001 LVD/mm 45(42,47) 45(41,46) 0.222 左室后壁厚度/mm 10(9,11) 9(9,9) <0.001 肺动脉压/mmHg 25(21,33) 23(21,27) 0.052 相对室璧厚度 0.43(0.39,0.48) 0.40(0.38,0.42) 0.021 三尖瓣反流速度/(m·s-1) 2.20±0.44 2.02±0.21 0.021 心脏磁共振 右室游离璧EAT厚度/mm 5.1(4.4,6.1) 4.2(3.9,4.6) <0.001 右侧房室沟EAT厚度/mm 16.1±3.5 14.2±4.5 0.006 左侧房室沟EAT厚度/mm 14.3(12.6,16.8) 11.8(9.9,14.2) <0.001 LVEF/% 65.6±7.8 65.2±6.2 0.798 LVMI/(g·m-2) 54.7(41.7,70.8) 49.8(43.9,57.9) 0.207 LVEDVI/(mL·m-2) 56.7±15.5 56.9±13.1 0.960 LVESVI/(mL·m-2) 19.1(13.9,24.3) 21.3(15.0,25.1) 0.541 SVI/(mL·m-2) 37.0±9.8 37.2±7.6 0.900 CI/(mL·m-2) 2.6±0.7 2.8±0.8 0.181 LAVI/(mL·m-2) 44.1(34.8,51.9) 31.2(28.1,37.9) <0.001 LVEDVI:左室舒张末期容积指数;LVESVI:左室收缩末期容积指数;LAVI:左心房容积指数。 表 3 单因素logistic回归分析
Table 3. 单因素logistic回归分析
变量 β Wald χ2 P OR 95%CI 肥厚型心肌病 -19.937 7338.195 0.998 0 0 房颤 -19.871 8569.168 0.998 0 0 高血压 1.244 6.690 0.010 0.288 0.112~0.740 高脂血症 2.711 6.916 0.009 0.066 0.009~0.501 冠心病 -7.40 2.830 0.093 0.477 0.202~1.130 NT-proBNP 0.033 20.584 <0.001 1.034 1.019~1.049 肌钙蛋白I 2.899 0.785 0.376 18.164 0.030~11071.885 糖化血红蛋白 0.767 5.472 0.019 2.152 1.132~4.092 C-反应蛋白 0.229 3.277 0.070 1.257 0.981~1.611 肾小球滤过率 0 0.013 0.910 1 0.995~1.005 血红蛋白 -0.025 4.601 0.032 0.976 0.954~0.998 E/A -0.622 2.120 0.145 0.537 0.232~1.240 LAD 0.187 16.461 <0.001 1.206 1.102~1.320 左室后壁厚度 0.676 10.974 0.01 1.965 1.318~2.931 相对室璧厚度 8.480 5.976 0.015 4816.827 5.370~4320301.001 三尖瓣反流速度 1.235 5.226 0.022 3.439 1.193~9.918 右室游离璧EAT 1.151 16.073 <0.001 3.163 1.801~5.554 右侧房室沟EAT 0.161 7.245 0.007 1.175 1.045~1.321 左侧房室沟EAT 0.284 14.268 <0.001 1.328 1.146~1.539 LAVI 0.097 18.486 <0.001 1.102 1.054~1.151 表 4 多因素logistic回归分析
Table 4. 多因素logistic回归分析
变量 β Waldχ2 P OR 95%CI 高脂血症 4.430 2.917 0.088 83.957 0.520~13547.884 NT-proBNP 0.092 10.063 0.002 1.097 1.036~1.161 左室后壁厚度 2.117 6.683 0.010 8.309 1.669~41.376 右室游离璧EAT 1.900 3.980 0.046 6.683 1.034~43.199 左侧房室沟EAT 0.408 3.683 0.055 1.503 0.991~2.279 -
[1] Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015[J]. European Journal of Heart Failure, 2019, 21(11): 1329-1337. doi: 10.1002/ejhf.1629
[2] 国家心血管病医疗质量控制中心专家委员会心力衰竭专家工作组. 2020中国心力衰竭医疗质量控制报告[J]. 中华心力衰竭和心肌病杂志, 2020, 4(4): 237-249. doi: 10.3760/cma.j.cn101460-20201217-00123
[3] 周浩斌, 色珍, 白煜佳, 等. 射血分数减低和非射血分数减低心力衰竭患者的临床特征和预后[J]. 中华心力衰竭和心肌病杂志(中英文), 2018, 2(2): 65-70. https://cdmd.cnki.com.cn/Article/CDMD-10422-1019078289.htm
[4] Galllina BA, Daniela B, Bartholow DB, et al. Epicardial fat: definition, measurements and systematic review of main outcomes. [J]. Arquivos Brasileiros De Cardiologia, 2013, 101: E18-E28.
[5] Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart[J]. Nature Clinical Practice Cardiovascular Medicine, 2005, 2(10): 536-543. doi: 10.1038/ncpcardio0319
[6] Iacobellis G, Bianco A C. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. [J]. Trends Endocrinol Metab, 2011, 22(11): 450-457. doi: 10.1016/j.tem.2011.07.003
[7] Machann J, Thamer C, Schnoedt B, et al. Standardized assessment of whole body adipose tissue topography by MRI[J]. Journal of Magnetic Resonance Imaging, 2005, 21(4): 455-462. doi: 10.1002/jmri.20292
[8] S Flüchter, Haghi D, Dinter D, et al. Volumetric assessment of epicardial adipose tissue with cardiovascular magnetic resonance imaging[J]. Obesity, 2007, 15(4): 870-878. doi: 10.1038/oby.2007.591
[9] Burkert P, Carsten T, De B, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association(HFA)of the European Society of Cardiology(ESC)[J]. European Heart Journal, 2019, 40(40): 3297-3317. doi: 10.1093/eurheartj/ehz641
[10] Shahar E. Trends in prevalence and outcome of heart failure with preserved ejection fraction[J]. N Engl J Med, 2006, 355(3): 251-259. doi: 10.1056/NEJMoa052256
[11] Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study[J]. New England Journal of Medicine, 2006, 355(3): 260. doi: 10.1056/NEJMoa051530
[12] Jaarsma T. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction[J]. Journal of the American College of Cardiology, 2013, 61(14): 1498-1506. doi: 10.1016/j.jacc.2012.12.044
[13] Kuno T, Ueyama H, Fujisaki T, et al. Meta-analysis evaluating the effects of renin-angiotensin-aldosterone system blockade on outcomes of heart failure with preserved ejection fraction[J]. The American Journal of Cardiology, 2020, 125(8): 1187-1193. doi: 10.1016/j.amjcard.2020.01.009
[14] Nielsen EE, Feinberg JB, Bu Fl, et al. Beneficial and harmful effects of sacubitril/valsartan in patients with heart failure: a systematic review of randomised clinical trials with meta-analysis and trial sequential analysis[J]. Open Heart, 2020, 7(2): e001294. doi: 10.1136/openhrt-2020-001294
[15] 杨帅, 杨萍萍, 吴清华. ARNI在常见心血管及相关疾病中应用的研究进展[J]. 临床心血管病杂志, 2021, 37(3): 279-283. http://lcxb.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=9c3c3779-6265-43e3-8e17-4fbd26667dbe
[16] Hypertonic Saline in Conjunction with High-Dose Furosemide Improves Dose-Response Curves in Worsening Refractory Congestive Heart Failure[J]. Advances in Therapy, 2015, 32(10): 971-982.
[17] Li S, Zhang X, Dong M, et al. Effects of spironolactone in heart failure with preserved ejection fraction: A meta-analysis of randomized controlled trials[J]. Medicine, 2018, 97(35): 111.
[18] Martin N, Manoharan K, Davies C, et al. Beta-blockers and inhibitors of the renin-angiotensin aldosterone system for chronic heart failure with preserved ejection fraction[J]. Cochrane Database of Systematic Reviews(Online), 2021, 5(5): 111.
[19] Shamloo A S, Schoene K, Stauber A, et al. Epicardial adipose tissue thickness as an independent predictor of ventricular tachycardia recurrence following ablation[J]. Heart Rhythm, 2019, 16(10): 1492-1498. doi: 10.1016/j.hrthm.2019.06.009
[20] Christopher X, Wong X. Epicardial fat and atrial fibrillation: current evidence, potential mechanisms, clinical implications, and future directions[J]. European Heart Journal, 2017, 38(17): 1294-1302.
[21] Mirolo A, Viart G, A Savouré, et al. Epicardial fat thickness predicts atrial fibrillation recurrence after a first pulmonary vein isolation procedure using a second-generation cryoballoon[J]. Archives of Cardiovascular Diseases, 2019, 112(5): 314-322. doi: 10.1016/j.acvd.2018.11.011
[22] Milton P. The epicardial adipose inflammatory triad: coronary atherosclerosis, atrial fibrillation, and heart failure with a preserved ejection fraction[J]. European Journal of Heart Failure, 2018, 20(11): 1567-1569. doi: 10.1002/ejhf.1294
[23] Mrad G, Ancel E. Exenatide decreases liver fat content and epicardial adipose tissue in patients with obesity and type 2 diabetes: a prospective randomized clinical trial using magnetic resonance imaging and spectroscopy[J]. Diabetes, Obesity & Metabolism, 2016, 18(9): 882-891.
[24] Bouchi R, Terashima M, Sasahara Y, et al. Luseogliflozin reduces epicardial fat accumulation in patients with type 2 diabetes: A pilot study[J]. Cardiovascular Diabetology, 2017, 16(1): 32. doi: 10.1186/s12933-017-0516-8
[25] Packer M. Do Drugs that ameliorate epicardial adipose tissue inflammation have concordant benefits on atrial fibrillation and on heart failure with a preserved ejection fraction?[J]. Journal of Cardiac Failure, 2019, 25(12): 986-1003. doi: 10.1016/j.cardfail.2019.09.002
[26] Dozio E, Ruscica M, Vianello E, et al. PCSK9 expression in epicardial adipose tissue: molecular association with local tissue inflammation[J]. Mediators of Inflammation, 2020, 2020(3): 1-8.
[27] 陈洋, 郭方君, 阮月华, 等. PCSK9抑制剂不良反应的研究进展[J]. 临床心血管病杂志, 2021, 37(8): 775-779. http://lcxb.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=bc79c100-da7a-4116-a33c-9288bd20917f
-




 下载:
下载: