The relationship between preoperative serum LP(a) and revascularization after PCI in patients with acute coronary syndrome and type 2 diabetes
-
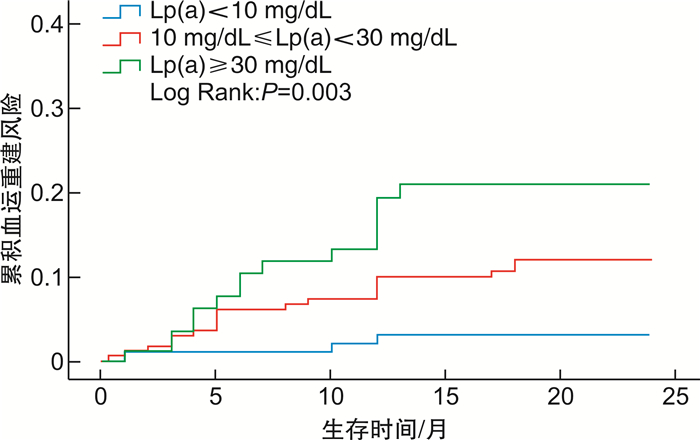
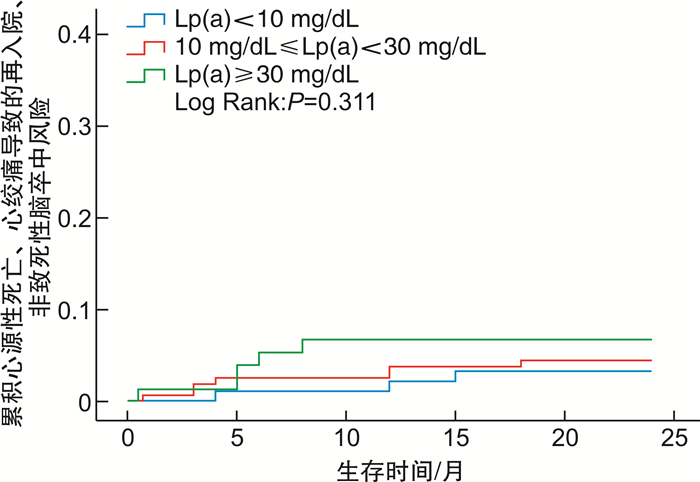
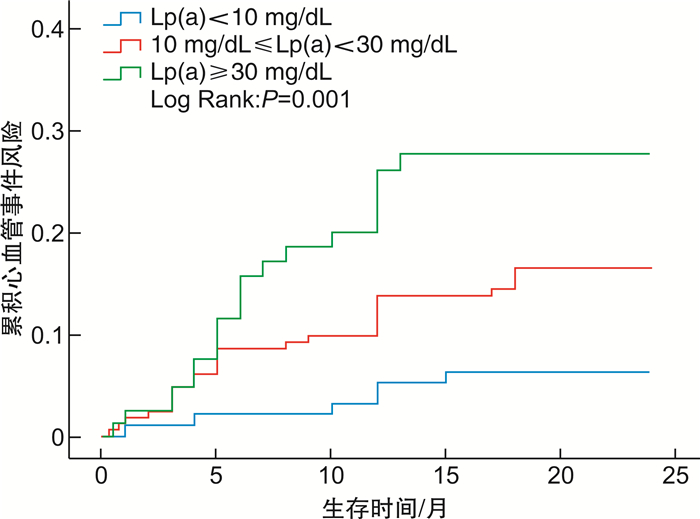
摘要: 目的 探讨术前血清脂蛋白a[LP(a)]与急性冠状动脉综合征(ACS)合并2型糖尿病患者经皮冠状动脉介入治疗(PCI)术后血运重建的关系。方法 连续纳入353例初次诊断ACS并接受PCI的2型糖尿病患者,根据术前LP(a)水平分为高水平(≥30 mg/dL)、中间水平(10~30 mg/dL)、低水平(< 10 mg/dL)3组,进行2年随访,终点事件定义为主要不良心血管事件(MACE)。MACE包括心源性死亡、心肌缺血导致的血运重建、不稳定型心绞痛导致的再入院及非致死性脑卒中。利用Kaplan-Meier、Cox回归分析探究LP(a)与ACS合并2型糖尿病患者PCI术后血运重建的关系。结果 在2年的随访中,共出现68例MACE,其中因心肌缺血导致的血运重建52例(76.47%);MACE组LP(a)水平较非MACE组显著升高(22.60 mg/dL vs 14.30 mg/dL,P< 0.01)。Kaplan-Meier分析显示,在2型糖尿病患者中,高水平LP(a)组患者发生MACE的风险较中、低水平组显著增加(Log Rank:P=0.001),且主要是增加血运重建的发生(Log Rank:P=0.003);Cox回归分析进一步证实LP(a)≥30 mg/dL是糖尿病患者PCI术后再次血运重建的独立危险因素(HR=3.154;95%CI:1.444~6.888;P< 0.01),即便是调整相关危险因素后仍与血运重建相关(HR=3.169;95%CI:1.270~7.907,P< 0.05)。结论 术前血清LP(a)水平升高与ACS合并2型糖尿病患者PCI术后血运重建相关。
-
关键词:
- 脂蛋白a /
- 急性冠状动脉综合征 /
- 2型糖尿病 /
- 经皮冠状动脉介入治疗 /
- 血运重建
Abstract: Objective To investigate the relationship between preoperative serum lipoprotein a([LP(a)]) and revascularization after percutaneous coronary intervention(PCI) in patients with acute coronary syndrome(ACS) complicated with type 2 diabetes mellitus.Methods 353 patients with type 2 diabetes who were diagnosed with ACS for the first time and received PCI were consecutively enrolled. According to the preoperative level of LP(a), they were divided into high level(≥30 mg/dL), intermediate level(10~30 mg/dL), and low level(< 10 mg/dL) groups and were followed up for 2 years. The endpoint event was defined as a major adverse cardiovascular event(MACE). MACE includes cardiogenic death, revascularization caused by myocardial ischemia, readmission caused by unstable angina, and non-fatal stroke. Kaplan-Meier and Cox regression analyses were used to explore the relationship between LP(a) and revascularization after PCI in patients with ACS and type 2 diabetes.Results During the 2-year follow-up, 68 cases of MACEs occurred, of which 52 cases(76.47%) occurred in revascularization caused by myocardial ischemia; the level of LP(a) in the MACE group was significantly higher than that in the non-MACE group(22.60 mg/dL vs. 14.30 mg/dL,P< 0.01). Kaplan-Meier analysis showed that in patients with type 2 diabetes, the risk of MACE in the high-level LP(a) group was significantly higher than that in the middle and low-level groups(Log Rank:P=0.001), and it mainly increased the occurrence of revascularization(Log Rank:P=0.003); Cox regression analysis further confirmed that LP(a) ≥30 mg/dL was an independent risk factor for revascularization in diabetic patients after PCI(HR=3.154; 95%CI: 1.444~6.888;P< 0.01), even after adjusting for related risk factors, it was still related to revascularization(HR=3.169; 95%CI: 1.270~7.907,P< 0.05).Conclusion Increased preoperative serum LP(a) level is associated with revascularization after PCI in ACS patients with type 2 diabetes. -

-
表 1 不同LP(a)水平患者的基线特征
Table 1. Baseline clinical characteristics of patients with different LP(a) levels
例(%), X±S, M(P25, P75) 项目 低水平LP(a)组
(98例)中间水平LP(a)组
(172例)高水平LP(a)组
(83例)P 一般特征 男性 55(56.12) 103(59.88) 45(54.22) 0.656 年龄/岁 65.01±10.35 65.85±8.98 65.95±10.00 0.745 BMI/(kg·m-2) 26.02±2.96 26.40±3.60 25.61±3.10 0.222 收缩压/mmHg 136.42±18.21 135.08±19.91 137.01±18.85 0.720 心率/ (次·min-1) 69.75±9.69 70.12±13.07 71.88±11.92 0.441 现吸烟史 32(32.65) 52(30.23) 28(33.73) 0.831 现饮酒史 26(26.53) 41(23.84) 24(28.92) 0.665 高血压 67(68.37) 122(70.93) 64(77.11) 0.330 实验室指标 LDL-C/(mmol·L-1) 2.32±0.67 2.53±0.89 2.65±0.99 < 0.05 TC/(mmol·L-1) 4.14±1.12 4.25±1.16 4.35±1.25 0.472 TG/(mmol·L-1) 1.83±1.07 1.79±1.01 1.45±0.63 < 0.05 HDL-C/(mmol·L-1) 1.14±0.34 1.17±0.27 1.19±0.22 0.436 Apo A1/(g·L-1) 1.28±0.26 1.29±0.25 1.25±0.25 0.608 Apo B/(g·L-1) 0.85±0.22 0.92±0.27 0.96±0.29 < 0.05 LP(a)/(mg·dL-1) 7.34(5.34,87.3) 16.4(12.5,20.9) 46.4(37.0,63.7) < 0.01 HbA1c/% 7.82±1.11 7.90±1.60 7.52±1.27 0.385 LVEF/% 59.43±6.31 56.77±8.69 56.84±9.10 < 0.01 术后用药 阿司匹林 98(100.00) 170(98.84) 82(98.80) 0.533 P2Y12抑制剂 97(98.98) 168(97.67) 82(98.80) 0.672 他汀药物 98(100.00) 170(98.84) 82(98.80) 0.559 β受体阻滞剂 63(64.29) 115(66.86) 61(73.49) 0.396 钙通道阻滞剂 36(36.73) 50(29.07) 23(27.71) 0.328 硝酸酯类 70(71.43) 121(70.35) 60(72.29) 0.947 ACEI/ARB 46(46.94) 75(43.60) 34(40.96) 0.717 糖尿病治疗 口服药物 61(62.24) 106(61.63) 49(59.04) 0.895 胰岛素 29(29.59) 47(27.33) 23(27.71) 0.921 注:HbA1c:糖化血红蛋白,ACEI/ARB:血管紧张素转化酶抑制剂/血管紧张素Ⅱ受体拮抗剂。 表 2 MACE组与非MACE组基线资料比较
Table 2. Comparison of baseline data between the MACE group and the non-MACE group
例(%), X±S, M(P25, P75) 项目 MACE组(68例) 非MACE组(285例) P 一般特征 男性 41(60.29) 162(56.84) 0.605 年龄/岁 67.69±9.55 65.15±9.56 0.050 BMI/(kg·m-2) 26.10±3.83 26.11±3.19 0.973 现吸烟史 23(33.82) 89(31.23) 0.679 现饮酒史 17(25.00) 74(25.96) 0.858 高血压 50(73.53) 203(71.23) 0.578 实验室指标 LDL-C/(mmol·L-1) 2.32±0.92 2.54±0.85 0.092 TC/(mmol·L-1) 3.93±1.11 4.32±1.18 0.635 TG/(mmol·L-1) 1.51±0.76 1.77±0.99 0.056 HDL-C/(mmol·L-1) 1.19±0.31 1.18±0.30 0.680 Apo A1/(g·L-1) 1.26±0.22 1.28±0.26 0.665 Apo B/(g·L-1) 0.86±0.27 0.92±0.26 0.065 LP(a)/(mg·dL-1) 22.60(12.83,43.32) 14.30(8.90,24.13) < 0.01 HbA1c/% 8.05±1.40 7.72±1.38 0.229 LVEF/% 56.13±9.38 57.84±7.96 0.130 术后用药 阿司匹林 66(97.06) 284(99.65) 1.000 P2Y12抑制剂 65(95.59) 282(98.95) 0.160 他汀药物 67(98.53) 283(99.30) 1.000 β受体阻滞剂 47(69.12) 192(67.37) 0.782 钙离子通道阻滞剂 19(27.94) 90(31.58) 0.560 硝酸酯类 48(70.59) 203(71.23) 0.917 ACEI/ARB 29(42.65) 126(44.21) 0.815 糖尿病治疗 口服药物 40(58.82) 176(61.75) 0.656 胰岛素 19(27.94) 80(28.07) 0.983 术后3个月实验室指标 LDL-C/(mmol·L-1) 1.66±0.50 1.65±0.46 0.838 TC/(mmol·L-1) 2.65±0.71 2.81±0.76 0.128 Apo B/(g·L-1) 0.54±0.17 0.58±0.17 0.069 LP(a)/(mg·dL-1) 23.85(11.15,48.78) 15.72(7.50,29.73) < 0.01 HbA1c/% 6.91±0.96 6.76±0.95 0.417 表 3 LP(a)水平与ACS合并糖尿病患者PCI术后MACE的关系
Table 3. Relation of LP(a)levels with MACE in diabetic patients with ACS after PCI
例(%) 项目 事件 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P MACEs LP(a) < 10 mg/dL 12(12.24) 参照 参照 10 mg/dL≤LP(a)<30 mg/dL 29(16.86) 1.464(0.747~2.869) 0.267 1.728(0.804~3.715) 0.161 LP(a)≥30 mg/dL 27(32.53) 3.017(1.528~5.958) < 0.01 2.722(1.200~6.173) < 0.05 心肌缺血导致的血运重建 LP(a) < 10 mg/dL 9(9.18) 参照 参照 10 mg/dL≤LP(a)<30 mg/dL 22(12.79) 1.486(0.684~3.227) 0.317 1.712(0.716~4.093) 0.227 LP(a)≥30 mg/dL 21(25.30) 3.154(1.444~6.888) < 0.01 3.169(1.270~7.907) < 0.05 心源性死亡、心绞痛导致的再入院、非致死性脑卒中 LP(a) < 10 mg/dL 3(3.06) 参照 参照 10 mg/dL≤LP(a)<30 mg/dL 7(4.07) 1.397(0.361~5.404) 0.628 1.686(0.337~8.434) 0.525 LP(a)≥30 mg/dL 6(7.23) 2.614(0.653~10.458) 0.174 1.425(0.216~9.383) 0.713 -
[1] Pandey A, McGuire DK, de Lemos JA, et al. Revascularization Trends in Patients With Diabetes Mellitus and Multivessel Coronary Artery Disease Presenting With Non-ST Elevation Myocardial Infarction: Insights From the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network Registry-Get with the Guidelines(NCDR ACTION Registry-GWTG)[J]. Circ Cardiovasc Qual Outcomes, 2016, 9(3): 197-205. doi: 10.1161/CIRCOUTCOMES.115.002084
[2] Serban MC, Colantonio LD, Manthripragada AD, et al. Statin Intolerance and Risk of Coronary Heart Events and All-Cause Mortality Following Myocardial Infarction[J]. J Am Coll Cardiol, 2017, 69(11): 1386-1395.
[3] Xu N, Tang XF, Yao Y, et al. Lipoprotein(a)levels are associated with coronary severity but not with outcomes in Chinese patients underwent percutaneous coronary intervention[J]. Nutr Metab Cardiovasc Dis, 2020, 30(2): 265-273. doi: 10.1016/j.numecd.2019.09.020
[4] Sumarjaya I, Nadha I, Lestari A. High Lipoprotein(a) Levels as a Predictor of Major Adverse Cardiovascular Events in Hospitalized-Acute Myocardial Infarction Patients[J]. Vasc Health Risk Manag, 2020, 16: 125-132. doi: 10.2147/VHRM.S233503
[5] Takahashi N, Dohi T, Funamizu T, et al. Prognostic impact of lipoprotein(a)on long-term clinical outcomes in diabetic patients on statin treatment after percutaneous coronary intervention[J]. J Cardiol, 2020, 76(1): 25-29. doi: 10.1016/j.jjcc.2020.01.013
[6] Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association[J]. Circulation, 2019, 139(10): e56-e528.
[7] 吴硕, 赵志豪, 史宛鑫, 等. 脂蛋白a在心血管疾病中的研究进展[J]. 临床心血管病杂志, 2021, 37(12): 1151-1156. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202112017.htm
[8] Shah NP, Pajidipati NJ, McGarrah RW, et al. Lipoprotein(a): An Update on a Marker of Residual Risk and Associated Clinical Manifestations[J]. Am J Cardiol, 2020, 126: 94-102. doi: 10.1016/j.amjcard.2020.03.043
[9] Moldogazieva NT, Mokhosoev IM, Mel'nikova TI, et al. Oxidative Stress and Advanced Lipoxidation and Glycation End Products(ALEs and AGEs)in Aging and Age-Related Diseases[J]. Oxid Med Cell Longev, 2019, 2019: 3085756.
[10] Picard F, Adjedj J, Varenne O. [Diabetes Mellitus, a prothrombotic disease][J]. Ann Cardiol Angeiol(Paris), 2017, 66(6): 385-392. doi: 10.1016/j.ancard.2017.10.011
[11] Tsimikas S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies[J]. J Am Coll Cardiol, 2017, 69(6): 692-711. doi: 10.1016/j.jacc.2016.11.042
[12] 薛强, 曹雯丽, 饶莉, 等. 血管内超声评价他汀类药物治疗不稳定型心绞痛前后冠状动脉斑块稳定性的观察[J]. 临床心血管病杂志, 2020, 36(5): 438-444. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202005010.htm
[13] Rehberger Likozar A, Zavrtanik M, Šebeštjen M. Lipoprotein(a) in atherosclerosis: from pathophysiology to clinical relevance and treatment options[J]. Ann Med, 2020, 52(5): 162-177. doi: 10.1080/07853890.2020.1775287
[14] Saeed A, Sun W, Agarwala A, et al. Lipoprotein(a)levels and risk of cardiovascular disease events in individuals with diabetes mellitus or prediabetes: The Atherosclerosis Risk in Communities study[J]. Atherosclerosis, 2019, 282: 52-56. doi: 10.1016/j.atherosclerosis.2018.12.022
[15] Zhang Y, Jin JL, Cao YX, et al. Lipoprotein(a) predicts recurrent worse outcomes in type 2 diabetes mellitus patients with prior cardiovascular events: a prospective, observational cohort study[J]. Cardiovasc Diabetol, 2020, 19(1): 111. doi: 10.1186/s12933-020-01083-8
[16] Bigazzi F, Minichilli F, Sbrana F, et al. Gender difference in lipoprotein(a)concentration as a predictor of coronary revascularization in patients with known coronary artery disease[J]. Biochim Biophys Acta Mol Cell Biol Lipids, 2021, 1866(3): 158869.
[17] Tam DY, Dharma C, Rocha RV, et al. Revascularization Strategies for the Treatment of Multivessel Coronary Artery Disease in Patients With Diabetes Mellitus[J]. Circ Cardiovasc Interv, 2020, 13(9): e009082. doi: 10.1161/CIRCINTERVENTIONS.120.009082
[18] O'Donoghue ML, Fazio S, Giugliano RP, et al. Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk[J]. Circulation, 2019, 139(12): 1483-1492. doi: 10.1161/CIRCULATIONAHA.118.037184
[19] Bittner VA, Szarek M, Aylward PE, et al. Effect of Alirocumab on Lipoprotein(a)and Cardiovascular Risk After Acute Coronary Syndrome[J]. J Am Coll Cardiol, 2020, 75(2): 133-144. doi: 10.1016/j.jacc.2019.10.057
[20] Tsimikas S, Karwatowska-Prokopczuk E, Xia S. Lipoprotein(a)Reduction in Persons with Cardiovascular Disease. Reply[J]. N Engl J Med, 2020, 382(21): e65. doi: 10.1056/NEJMc2004861
-




 下载:
下载: