Evaluation of right ventricular dyssynchrony by two-dimensional speckle tracking echocardiography in patients of connective tissue disease-associated pulmonary arterial hypertension
-
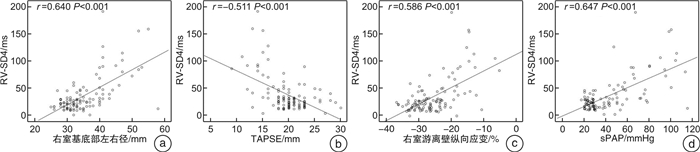
摘要: 目的 探讨二维斑点追踪超声心动图评估结缔组织病(CTD)患者右室同步性的变化及其诊断肺动脉高压(PAH)的价值。方法 前瞻性纳入2018年5月—2019年12月在风湿免疫科确诊的CTD患者111例,同期选取32例健康体检者作为正常对照。据超声估测肺动脉收缩压(sPAP)将111例CTD患者分为两组:肺动脉压力正常组(sPAP≤36 mmHg,1mmHg=0.133 kPa)60例,PAH组(sPAP>36 mmHg)51例。常规超声心动图获取左房前后径、左室前后径及左室射血分数;右房左右径、右室左右径及三尖瓣环收缩期位移(TAPSE)、右室面积变化率(FAC)及三尖瓣环收缩期峰值流速。二维斑点追踪超声心动图测量右室游离壁基底段与中间段纵向应变值、室间隔基底段与中间段纵向应变值,并计算上述4个右室壁应变达峰时间标准差(RV-SD4)。结果 与正常对照组相比,CTD患者右室游离壁纵向应变值显著减低(P<0.05),但右室RV-SD4明显增加(P<0.05);与CTD肺动脉压力正常组比较,PAH组右室游离壁纵向应变值明显减低(P<0.05),但右室RV-SD4亦明显增加(P<0.05)。Pearson相关性分析显示,RV-SD4与右室游离壁纵向应变(r=0.586,P<0.001)及sPAP(r=0.647,P<0.001)呈正相关;同时RV-SD4与TAPSE(r=-0.511,P<0.001)及FAC(r=-0.601,P<0.001)呈负相关。RV-SD4诊断PAH的ROC曲线下面积约0.777,灵敏度和特异度分别为67%和83%。结论 二维斑点追踪超声心动图中RV-SD4指标可有效反映CTD合并PAH患者右室壁收缩不同步,并随着sPAP升高,右室壁收缩不同步更显著。Abstract: Objective This study sought to investigate the clinical value of two-dimensional speckle tracking echocardiography for evaluating right ventricular dyssynchrony in patients of connective tissue disease-associated pulmonary arterial hypertension.Methods A total of 111 patients with connective tissue disease(CTD) and 32 healthy controls were prospectively recruited. According to systolic pulmonary artery pressure(sPAP), the CTD patients were divided into 2 subgroups: CTD without pulmonary arterial hypertension(PAH) group(sPAP ≤ 36 mmHg,n=60) and CTD-PAH group(sPAP>36 mmHg,n=51). The left atrium, left ventricle, left ventricular ejection fraction, right atrium, right ventricle, tricuspid annular plane systolic excursion(TAPSE), fractional area change(FAC) and the tricuspid annular plane systolic velocity(S') were measured by conventional echocardiography. Global right ventricular longitudinal deformation parameters were recorded by two-dimensional strain echocardiography from apical 4-chamber views using a four mid-basal RV segments model. The standard deviation of the heart rate-corrected intervals from QRS onset to peak strain for the 4 segments(RV-SD4) was used to quantify right intraventricular dyssynchrony.Results Compared with control group, the CTD group exhibited significantly lower longitudinal peak systolic strain of mid-basal RV segments(P< 0.05), while RV-SD4 was significant longer(P< 0.05). Compared with CTD without PAH group, the CTD-PAH group displayed lower longitudinal peak systolic strain of mid-basal RV segments(P< 0.05), while RV-SD4 was significant longer(P< 0.05). In CTD patients, RV-SD4 were moderately positive correlated with right ventricular longitudinal strain(r=0.586,P< 0.001), sPAP(r=0.647,P< 0.001), and were moderately negative correlated with TAPSE(r=-0.511,P< 0.001), and FAC(r=-0.601,P< 0.001). According to the receiver operating characteristic curve analysis, the areas under the curve of RV-SD4 for CTD-PAH patients was 0.777(P< 0.001), and the sensitivity and specificity were 67% and 83%, respectively.Conclusion In CTD-PAH patients, RV dyssynchrony could be significantly evaluated by RV-SD4 of two-dimensional speckle tracking echocardiography, and the RV dyssynchrony was moderately associated with systolic pulmonary artery pressure.
-

-
表 1 各组基线资料分析
Table 1. General data
X±S 参数 正常对照组(32例) CTD组(111例) CTD组 P值(正常对照vs CTD) P值(肺动脉压力正常组vs PAH组) 肺动脉压力正常组(60例) PAH组(51例) 年龄/岁 43±12 41±15 41±15 41±14 0.520 0.970 女性/例(%) 28(87.5) 99(89.2) 50(83.3) 49(96.1) 0.760 0.030 体表面积/m2 1.63±0.15 1.60±0.16 1.63±0.18 1.56±0.13 0.330 0.030 心率/(次·min-1) 69±9 78±13 76±12 79±14 0.001 0.190 QRS/ms 93±7 94±7 93±7 96±8.0 0.630 0.047 CTD分类/例(%) 系统性红斑狼疮 — 45(40.5) 19(31.7) 26(51.0) — 0.040 皮肌炎/多肌炎 — 31(27.9) 28(46.7) 3(5.9) — <0.001 系统性硬皮病 — 14(12.6) 5(8.3) 9(17.6) — 0.140 混合结缔组织病 — 8(7.2) 4(6.7) 4(7.8) — 1.000 干燥综合征 — 7(6.3) 3(5.0) 4(7.8) — 0.700 大动脉炎 — 4(3.6) 1(1.7) 3(5.9) — 0.330 类风湿关节炎 — 2(1.8) 0(0) 2(3.9) — 0.210 心功能分级/例(%) Ⅲ/Ⅳ — 41(36.9) 6(10.0) 35(68.6) — <0.001 表 2 各组超声指标分析
Table 2. Analysis of ultrasound indexes in each group
X±S 参数 正常对照组(32例) CTD组(111例) CTD组 P值(正常对照vs CTD) P值(肺动脉压力正常组vs PAH组) 肺动脉压力正常组(60例) PAH组(51例) 左房/mm 31.7±2.7 33.0±4.3 33.9±4.4 32.0±4.0 0.040 0.020 左室/mm 45.8±3.0 44.6±4.4 46.2±3.1 42.8±5.1 0.080 <0.001 LVEF/% 65.6±1.5 65.3±2.4 64.9±1.8 65.8±2.9 0.510 0.056 右房/mm 31.2±2.6 33.8±6.6 30.5±3.1 37.6±7.4 0.001 <0.001 右室/mm 31.6±2.6 35.2±6.7 31.2±3.0 39.9±6.8 <0.001 <0.001 心包积液/例(%) 0(0) 24(21.6) 5(8.3) 19(37.3) — <0.001 TAPSE/mm 22.2±1.8 19.7±3.8 21.2±2.8 17.8±4.0 <0.001 <0.001 FAC/% 47.1±4.0 40.2±8.2 44.2±4.8 35.5±8.9 <0.001 <0.001 S′/(cm·s-1) 12.1±1.5 11.7±2.4 12.6±2.2 10.6±2.1 0.240 <0.001 右室游离壁应变/% -30.3±4.2 -25.7±6.5 -28.6±4.1 -22.4±7.2 <0.001 <0.001 RV-SD4/ms 13.3±6.8 35.6±33.8 20.8±9.9 52.9±42.7 <0.001 <0.001 -
[1] 卢一品, 刘宏生. 肺动脉高压发病机制和药物治疗进展[J]. 临床心血管病杂志, 2019, 35(2): 109-112. https://lcxb.chinajournal.net.cn/WKC/WebPublication/paperDigest.aspx?paperID=6373d58a-b9e2-423e-93fd-93becd2885ca
[2] Yamagata Y, Ikeda S, Kojima S, et al. Right ventricular dyssynchrony in patients with chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension[J]. Circ J, 2022, 86(6): 936-944. doi: 10.1253/circj.CJ-21-0849
[3] Badagliacca R, Papa S, Valli G, et al. Right ventricular dyssynchrony and exercise capacity in idiopathic pulmonary arterial hypertension[J]. Eur Respir J, 2017, 49(6): 1601419. doi: 10.1183/13993003.01419-2016
[4] Badagliacca R, Reali M, Poscia R, et al. Right intraventricular dyssynchrony in idiopathic, heritable, and anorexigen-induced pulmonary arterial hypertension: clinical impact and reversibility[J]. JACC Cardiovasc Imaging, 2015, 8(6): 642-652. doi: 10.1016/j.jcmg.2015.02.009
[5] Demirci M, Ozben B, Sunbul M, et al. The evaluation of right ventricle dyssynchrony by speckle tracking echocardiography in systemic sclerosis patients[J]. J Clin Ultrasound, 2021, 49(9): 895-902. doi: 10.1002/jcu.23041
[6] 屈文涛, 许磊, 康亚宁, 等. 二维斑点追踪技术评价2型糖尿病患者右室心肌功能与心外膜脂肪厚度的相关性研究[J]. 临床心血管病杂志, 2020, 36(3): 275-279. https://lcxb.chinajournal.net.cn/WKC/WebPublication/paperDigest.aspx?paperID=b3f10e11-7bac-4625-92d4-5d155d91574a
[7] Lamia B, Muir JF, Molano LC, et al. Altered synchrony of right ventricular contraction in borderline pulmonary hypertension[J]. Int J Cardiovasc Imaging, 2017, 33(9): 1331-1339. doi: 10.1007/s10554-017-1110-6
[8] Li X, Zhang C, Sun X, et al. Prognostic factors of pulmonary hypertension associated with connective tissue disease: pulmonary artery size measured by chest CT[J]. Rheumatology(Oxford), 2020, 59(11): 3221-3228. doi: 10.1093/rheumatology/keaa100
[9] Vonk Noordegraaf A, Chin KM, Haddad F, et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update[J]. Eur Respir J, 2019, 53(1): 1801900. doi: 10.1183/13993003.01900-2018
[10] Liu BY, Wu WC, Zeng QX, et al. Two-dimensional speckle tracking echocardiography detected interventricular dyssynchrony predicts exercise capacity and disease severity in pre-capillary pulmonary hypertension[J]. Ann Transl Med, 2020, 8(7): 456. doi: 10.21037/atm.2020.03.146
[11] Badagliacca R, Poscia R, Pezzuto B, et al. Right ventricular dyssynchrony in idiopathic pulmonary arterial hypertension: determinants and impact on pump function[J]. J Heart Lung Transplant, 2015, 34(3): 381-389. doi: 10.1016/j.healun.2014.06.010
[12] Murata M, Tsugu T, Kawakami T, et al. Right ventricular dyssynchrony predicts clinical outcomes in patients with pulmonary hypertension[J]. Int J Cardiol, 2017, 228: 912-918. doi: 10.1016/j.ijcard.2016.11.244
[13] Haeck ML, Höke U, Marsan NA, et al. Impact of right ventricular dyssynchrony on left ventricular performance in patients with pulmonary hypertension[J]. Int J Cardiovasc Imaging, 2014, 30(4): 713-720. doi: 10.1007/s10554-014-0384-1
[14] Pezzuto B, Forton K, Badagliacca R, et al. Right ventricular dyssynchrony during hypoxic breathing but not during exercise in healthy subjects: a speckle tracking echocardiography study[J]. Exp Physiol, 2018, 103(10): 1338-1346. doi: 10.1113/EP087027
[15] Marcus JT, Gan CT, Zwanenburg JJ, et al. Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling[J]. JAmColl Cardiol, 2008, 51(7): 750-757.
[16] Sharifi Kia D, Kim K, Simon MA. Current Understanding of the Right Ventricle Structure and Function in Pulmonary Arterial Hypertension[J]. Front Physiol, 2021, 12: 641310. doi: 10.3389/fphys.2021.641310
-





 下载:
下载: