Clinical efficiency of left bundle branch pacing in patients with heart failure and atrioventricular block
-
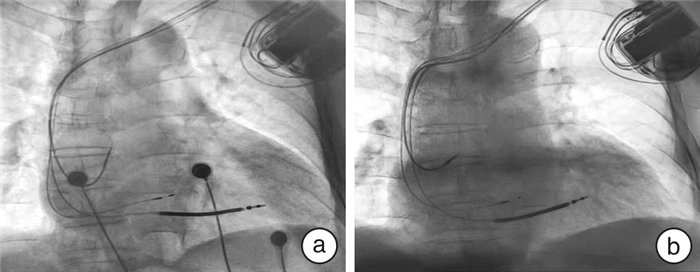
摘要: 目的 观察左束支起搏(LBBP)对慢性心力衰竭(心衰)合并持续性高度房室传导阻滞或三度房室传导阻滞患者的近中期临床疗效。方法 入选慢性射血分数降低的心衰合并持续性高度房室传导阻滞或三度房室传导阻滞需行起搏治疗的患者,分为LBBP组及常规双心室心脏同步化治疗(CRT)组。比较LBBP组起搏植入术中及随访6个月、12个月时各项起搏参数的变化。比较两组患者起搏治疗前后心电图QRS波时限,纽约心功能分级(NYHA)、左室舒张末期内径(LVEDD)、左室收缩末期内径(LVESD)、左室短轴缩短率(FS)、左室射血分数(LVEF)、血清B型脑钠肽(BNP)水平。结果 共有21例患者入组,术前两组患者年龄、性别、合并疾病、服用药物情况、QRS波时限、NYHA心功能分级、LVEDD、LVESD、FS、LVEF、BNP水平无显著差异(P>0.05)。LBBP组术中QRS波时限与术前比较明显缩窄(P<0.05);随访6、12个月发现,LBBP组QRS波时限、LBBP单极夺获左束支阈值、心室电极头端单极感知均稳定,电极头端阻抗与术中比较无显著变化(P>0.05);两组患者术后随访6、12个月,其NYHA心功能分级、LVEDD、LVESD、FS、LVEF、BNP水平均较术前有显著改善(P<0.05)。术中及术后随访6、12个月,LBBP组QRS时限较CRT组稍缩短(P<0.05);随访6个月时,LBBP组患者NYHA分级情况较CRT组改善(P<0.05),BNP水平降低(P<0.05),两组患者LVEDD、LVESD、LVEF无显著差异(P>0.05)。随访12个月,两组患者NYHA心功能分级、LVEDD、LVESD、FS、LVEF、BNP水平无显著差异(P>0.05)。结论 LBBP对于慢性射血分数降低的心衰合并持续性高度房室传导阻滞或三度房室传导阻滞患者治疗效果与传统CRT相似。Abstract: Objective This study was aimed to explore the efficiency of left bundle branch pacing(LBBP) in patients with heart failure and persistent high-grade or third-degree atrioventricular block.Methods Patients with chronic heart failure and high-grade atrioventricular block requiring pacemaker treatment were enrolled in the study from March 2018 to December 2020, and were randomly divided into LBBP group and cardiac synchronization therapy(CRT) group. QRS wave duration, left ventricular end-diastolic diameter(LVEDD), left ventricular ejection fraction(LVEF), cardiac function classification, pacemaker parameters, and serum brain natriuretic peptide(BNP) level were compared between the two groups during follow-up.Results A total of 21 patients were enrolled. There were no significant differences in age, gender, co-morbidity, drug use, QRS duration, NYHA cardiac function grade, LVEDD, LVESD, FS, LVEF and BNP levels between the two groups(P > 0.05) before surgery. QRS duration in LBBP group was significantly narrower compared with that before surgery(P < 0.05). During the follow-up of 6 months and 12 months, it was found that QRS duration, the threshold of LBBP unipolar capture of left bundle branch and the unipolar perception of ventricular electrode tip in LBBP group were stable, and the impedance of electrode tip had no significant change compared with that during surgery(P > 0.05). The NYHA cardiac function grading, LVEDD, LVESD, FS, LVEF and BNP levels in two groups were significantly improved after 6 and 12 months of postoperative follow-up compared with those before surgery(P < 0.05 or P < 0.01). The duration of QRS in LBBP group was slightly shorter than that in CRT group(P < 0.05). During 6-month follow-up, the NYHA grading in LBBP group was improved compared with that in CRT group(P < 0.05), while the BNP level was decreased(P < 0.05). There were no significant differences in LVEDD, LVESD and LVEF between the two groups(P > 0.05). After 12 months of follow-up, there were no significant differences in NYHA cardiac function grading, LVEDD, LVESD, FS, LVEF and BNP levels between the two groups(P > 0.05).Conclusion The clinical efficiency of LBBP in patients with chronic heart failure and persistent high-grade atrioventricular block or third-degree atrioventricular block is similar to that of conventional CRT.
-

-
表 1 两组患者术前一般临床资料
Table 1. General data
例(%), X±S 项目 LBBP组(8例) CRT组(13例) P值 年龄/岁 70.0±15.6 66.2±12.1 0.533 男性 5(62.5) 8(61.5) 0.965 LVEDD/mm 64.9±6.9 61.5±8.5 0.361 LVESD/mm 56.4±6.3 54.0±8.3 0.496 LVEF/% 27.9±7.2 26.6±6.3 0.677 FS/% 13.6±3.7 13.1±3.6 0.741 BNP/(pg·mL-1) 1253.1±832.9 1318.9±913.9 0.870 NYHA分级 0.925 Ⅲ 6(75.0) 10(76.9) Ⅳ 2(25.0) 3(23.1) QRS波时限/ms 128.4±16.5 124.6±19.7 0.835 缺血性心肌病 1(12.5) 2(15.4) 0.853 高血压 2(25.0) 4(30.7) 0.775 糖尿病 2(25.0) 3(23.1) 0.920 房颤 1(12.5) 2(15.4) 0.853 药物治疗 ARNI 8(100.0) 13(100.0) 利尿剂 8(100.0) 13(100.0) 降糖药 2(25.0) 3(23.1) 0.920 抗血小板药物 2(25.0) 4(30.7) 0.775 口服抗凝药 1(12.5) 2(15.4) 0.853 表 2 LBBP组患者起搏参数随访情况
Table 2. Follow-up of pacing parameters in patients in LBBP group
X±S 项目 术中 术后6个月 P值 术后12个月 P值 QRS波时限/ms 114.6±5.2 114.8±3.4 0.955 114.5±6.8 0.968 LBBP单极夺获左束支阈值/[(V·(0.42 ms)-1] 0.8±0.2 0.7±0.3 0.371 0.7±0.2 0.294 单极电极头端阻抗/Ω 631.3±133.6 597.5±108.9 0.588 601.3±98.2 0.617 电极头端单极感知/mV 9.1±3.4 9.8±3.5 0.721 8.8±2.8 0.814 表 3 两组术中和术后临床情况
Table 3. Clinical conditions of the two groups before and after operation
例(%), X±S 项目 LBBP组(8例) CRT组(13例) 术中 术后6个月 术后12个月 术中 术后6个月 术后12个月 QRS波时限/ms 114.6±5.21) 114.8±3.41) 114.5±6.81) 125.3±9.4 126.7±5.7 126.8±6.0 NYHA分级 Ⅰ 0(0) 2(25.0) 2(25.0) 0(0) 1(7.7) 2(15.4) Ⅱ 0(0) 5(62.5) 6(75.0) 0(0) 4(30.8) 9(69.2) Ⅲ 6(75.0) 1(12.5) 0(0) 10(76.9) 7(53.8) 2(15.4) Ⅳ 2(25.0) 0(0) 0(0) 3(23.1) 1(7.7) 0(0) LVEDD/mm 64.9±6.9 50.5±4.1 47.8±7.3 61.5±8.5 53.9±8.2 50.4±7.1 LVESD/mm 56.4±6.3 38.1±4.9 32.5±5.9 54.0±8.3 42.0±8.7 37.7±6.5 FS/% 13.6±3.7 24.6±5.7 28.0±3.5 26.6±6.3 21.5±3.7 24.7±4.6 LVEF/% 27.9±7.2 48.4±9.2 54.8±5.5 13.1±3.6 43.2±6.6 49.0±7.5 BNP/(pg·mL-1) 1253.1±832.92) 311.9±254.12) 181.1±67.72) 1318.9±913.9 571.2±199.2 219.6±124.4 与CRT组同时间段比较,1)P<0.01,2)P<0.05。 -
[1] Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology(ESC). Developed in collaboration with the European Heart Rhythm Association(EHRA)[J]. Eur Heart J, 2013, 34(29): 2281-2329. doi: 10.1093/eurheartj/eht150
[2] Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society[J]. J Am Coll Cardiol, 2018, 74(7): 932-987.
[3] Sweeney MO, Hellkamp AS, Ellenbogen KA, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction[J]. Circulation, 2003, 107(23): 2932-2937. doi: 10.1161/01.CIR.0000072769.17295.B1
[4] Tops LF, Schalij MJ, Bax JJ. The effects of right ventricular apical pacing on ventricular function and dyssynchrony implications for therapy[J]. J Am Coll Cardiol, 2009, 54(9): 764-776. doi: 10.1016/j.jacc.2009.06.006
[5] Huang WJ, Su L, Wu S, et al. A novel pacing strategy with low and stable output: pacing the left bundle branch immediately beyond the conduction block[J]. Can J Cardiol, 2017, 33(12): e1731-1736.
[6] Chen X, Jin Q, Bai J, et al. The feasibility and safety of left bundle branch pacing vs. right ventricular pacing after mid-long-term follow-up: a single-centre experience[J]. Europace, 2020, 22(Suppl-2): ii36-ii44.
[7] Zhang W, Huang J, Qi Y, et al. Cardiac resynchronization therapy by left bundle branch area pacing in patients with heart failure and left bundle branch block[J]. Heart Rhythm, 2019, 16(12): 1783-1790. doi: 10.1016/j.hrthm.2019.09.006
[8] Guo J, Li L, Xiao G, et al. Remarkable response to cardiac resynchronization therapy via left bundle branch pacing in patients with true left bundle branch block[J]. Clin Cardiol, 2020, 43(12): 1460-1468. doi: 10.1002/clc.23462
[9] Huang W, Wu S, Vijayaraman P, et al. Cardiac resynchronization therapy in patients with nonischemic cardiomyopathy using left bundle branch pacing[J]. JACC Clin Electrophysiol, 2020, 6(7): 849-858. doi: 10.1016/j.jacep.2020.04.011
[10] Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology(ESC)Developed with the special contribution of the Heart Failure Association(HFA)of the ESC[J]. Eur Heart J, 2016, 37(27): 2129-2200. doi: 10.1093/eurheartj/ehw128
[11] 王国营, 郑玥, 刘维康, 等. 2021欧洲心脏病学会急性心力衰竭指南解读[J]. 临床急诊杂志, 2022, 23(3): 177-182. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202203003.htm
[12] 张艳利, 于海侠, 郭金朋, 等. 新活素对心肺复苏后心力衰竭患者心功能及血清IL-6影响的研究[J]. 临床急诊杂志, 2020, 21(3): 209-211. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202003008.htm
[13] 叶嘉炜, 费爱华. CRRT联合药物治疗对急性失代偿性心力衰竭预后的影响[J]. 临床急诊杂志, 2019, 20(12): 913-918. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201912001.htm
[14] Curtis AB, Worley SJ, Adamson PB, et al. Biventricular pacing for atrioventricular block and systolic dysfunction[J]. N Engl J Med, 2013, 368(17): 1585-1593. doi: 10.1056/NEJMoa1210356
[15] Curtis AB, Worley SJ, Chung ES, et al. Improvement in clinical outcomes with biventricular versus right ventricular pacing: The BLOCK HF Study[J]. J Am Coll Cardiol, 2016, 67(18): 2148-2157. doi: 10.1016/j.jacc.2016.02.051
[16] 杨杰孚, 张健, 韩雅玲. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004
[17] Li Y, Chen K, Dai Y, et al. Recovery of complete left bundle branch block following heart failure improvement by left bundle branch pacing in a patient[J]. J Cardiovasc Electrophysiol, 2019, 30(9): 1714-1717. doi: 10.1111/jce.14034
[18] Wang Y, Gu K, Qian Z, et al. The efficacy of left bundle branch area pacing compared with biventricular pacing in patients with heart failure: A matched case-control study[J]. J Cardiovasc Electrophysiol, 2020, 31(8): 2068-2077. doi: 10.1111/jce.14628
[19] Chen X, Ye Y, Wang Z, et al. Cardiac resynchronization therapy via left bundle branch pacing vs. optimized biventricular pacing with adaptive algorithm in heart failure with left bundle branch block: a prospective, multi-centre, observational study[J]. Europace, 2022, 24(5): 807-816. doi: 10.1093/europace/euab249
[20] 蔡彬妮, 李琳琳, 黄心怡, 等. 左束支起搏的心脏电学和机械同步性及中远期导线稳定性研究[J]. 中国循环杂志, 2020, 35(1): 55-61. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202001011.htm
[21] Hua W, Fan X, Li X, et al. Comparison of left bundle branch and his bundle pacing in bradycardia patients[J]. JACC Clin Electrophysiol, 2020, 6(10): 1291-1299. doi: 10.1016/j.jacep.2020.05.008
[22] 吴梅琼, 林亚洲, 陈林, 等. 左束支起搏在心脏再同步治疗的初步应用经验[J]. 临床心血管病杂志, 2020, 36(4): 367-370. https://lcxb.chinajournal.net.cn/WKC/WebPublication/paperDigest.aspx?paperID=6e311608-a0ab-441b-8b68-e5f15ad6bd53
[23] 黄伟剑, 黄德嘉, 张澍. 希氏-浦肯野系统起搏中国专家共识[J]. 中华心律失常学杂志, 2021, 25(1): 10-36.
-




 下载:
下载: