The prognostic value of left atrial strain assessed by cardiac MR feature tracking to major adverse cardiovascular events in myocardial infarction patients
-
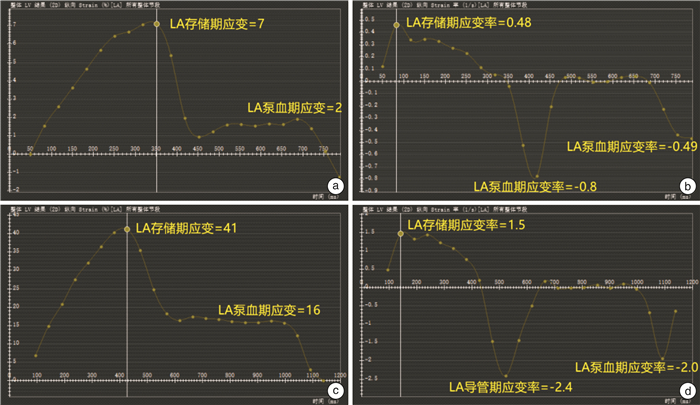
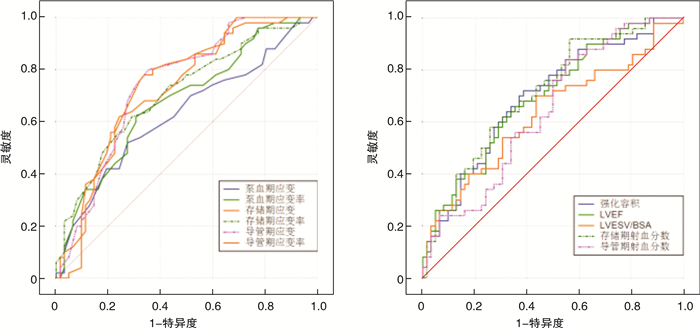
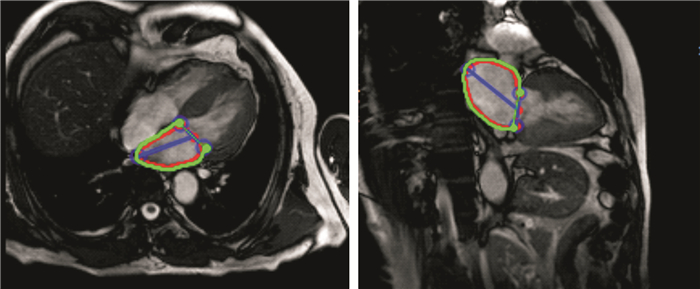
摘要: 目的利用心脏磁共振特征跟踪(CMR-FT)技术测定包括左心房(LA)应变在内的LA功能参数,初步探讨LA功能对心肌梗死(MI)患者发生主要心血管不良事件(MACE)的预测价值。方法收集2015年7月—2021年11月在昆明医科大学第二附属医院经临床及CMR确诊的MI患者112例,根据随访结果分为无MACE组和MACE组。所有患者均行CMR检查发现有明确心肌梗死灶,利用CMR-FT技术获得包括LA应变在内的LA功能参数。比较两组患者的临床基线资料及CMR参数,分析各参数对MI患者出现MACE的预测价值。结果共纳入MI患者112例,其中MACE组50例,无MACE组62例。两组患者LA 3期应变及应变率、LA存储期及导管期射血分数、左心室射血分数(LVEF)、左心室收缩末期容积标化值、梗死容积、年龄有显著统计学差异(P < 0.05)。LA存储期射血分数、LA存储期应变及应变率、LA导管期应变、LVEF与MI患者发生MACE呈负相关(rs < -0.3,P < 0.05)。LA导管期及泵血期应变率、梗死容积、左心室收缩末容积标化值及年龄与MI患者发生MACE呈正相关(rs>0.3,P < 0.05)。ROC分析提示导管期应变及应变率、存储期应变及应变率、存储期射血分数、梗死容积、LVEF及年龄对预测MI患者预后均有一定价值(AUC>0.7,P < 0.05),其中导管期应变及应变率的预测效能最大(AUC=0.74,P < 0.001)。结论CMR-FT技术可以量化LA应变参数并全面评估LA功能,对MI患者MACE的发生具有预测价值。LA应变参数预测效能总体优于LA容积参数及左心室功能参数,其中导管期应变及应变率对MI患者发生MACE预测效能最大。
-
关键词:
- 心肌梗死 /
- 左心房应变 /
- 主要心血管不良事件 /
- 心脏磁共振特征跟踪技术
Abstract: ObjectiveThe aims of this study were to evaluate The Prognostic Value of left atrial(LA) strain assessed with Cardiac MR feature tracking(CMR-FT) to major adverse cardiovascular events(MACE) in Myocardial Infarction(MI) Patients.MethodsBetween July 2015 and November 2021, 112 MI patients at admission were included in this study. According to the follow-up results, the study populationts were divided into MACE group and non-MACE group. All study participants underwent CMR and LA strain parameters were quantifified by CMR-FT. Various clinical and CMR parameters including LA strain were assessed for association with MACE in MI patients.ResultsA total of 112 participants were included. During follow-up, 50 patients reached the composite endpoint. There were significant differences between the LA strain, LA strain rate, LA reservoir ejection fraction, LA conduit ejection fraction, left ventricular ejection fraction(LVEF), left ventricular end-systolic volume index, percentage of infarct volume and age(P < 0.05). Spearman correlation analysis showed that LA reservoir ejection fraction, LA reservoir strain and strain rate, LA conduit strain and LVEF were slightly negatively correlated with MACE in MI paitents(rs < -0.3, P < 0.05). LA conduit strain rate, LA contraction rate, percentage of infarct volume, left ventricular end-systolic volume index and age were slightly positivly correlated with MACE in MI paitents(rs < -0.3, P < 0.05). ROC analysis revealed that LA reservoir strain and strain rate, LA conduit strain and strain rate, LA reservoir ejection fraction, LVEF and percentage of infarct volume had certain value for prognosis(AUC>0.7, P < 0.05). LA conduit strain and strain rate were the best predictors of MACE among these parameters.ConclusionCMR-FT can quantify the LA strain and comprehensively evaluate the LA function, which has predictive value for MACE in MI patients. The results showed that the predictive efficacy of LA strain parameters was superior to LA volume parameters and left ventricular function parameters in general, and the strain rate at catheter stage had the greatest predictive efficacy for MACE in MI patients. LA strain demonstrated better predictive power than LA volume index and left ventricular function parameters. LA conduit strain and strain rate were the best predictors of MACE. -

-
表 1 两组患者临床基线资料比较
Table 1. General data
X±S, M(P25, P75) 参数 总体(112例) 无MACE组(62例) MACE组(50例) χ2/t/ Z值 P值 男性/例(%) 91(81.2) 50(80.6) 41(82.0) -0.182 0.856 年龄/岁 55.21±13.98 50.79±14.08 60.68±11.88 -3.958 < 0.001 BMI/(kg·m-2) 23.78±3.11 23.97±3.17 23.54±3.06 0.719 0.474 吸烟/例(%) 66(58.9) 33(53.2) 33(66) -1.360 0.174 高血压/例(%) 52(46.4) 31(50.0) 21(42.0) -0.661 0.508 糖尿病/例(%) 19(17.0) 7(11.3) 12(24.0) -1.774 0.076 LDL/(mmol·L-1) 2.45±0.80 2.68±0.85 2.49±0.82 1.839 0.069 HDL/(mmol·L-1) 1.10±0.30 1.12±0.29 1.08±0.32 0.725 0.470 TC/(mmol·L-1) 4.22±1.12 4.36±1.13 4.04±1.10 1.495 0.138 TG/(mmol·L-1) 1.38(1.03,1.86) 1.54(1.17,1.88) 1.27(0.89,1.68) -1.926 0.054 MI与CMR间隔时间/d 19.00(15.00,36.00) 19.00(16.00,60.00) 18.00(15.00,34.00) -1.022 0.307 HDL:高密度脂蛋白;LDL:低密度脂蛋白;TC:总胆固醇;TG:甘油三酯。 表 2 两组患者左心室功能参数比较
Table 2. Left ventricular function parameters
X±S, M(P25, P75) 参数 总体(102例) 无MACE组(56例) MACE组(46例) χ2/t/ Z值 P值 LVEF/% 41.95±13.91 46.23±13.14 36.64±13.10 3.849 < 0.001 LVEDV/BSA/(mL·m-2) 78.21(63.56,106.18) 77.62(64.08,91.83) 82.09(60.24,121.68) -0.995 0.320 LVESV/BSA/(mL·m-2) 44.66(32.31,69.01) 36.57(31.14,59.67) 55.14(33.59,96.37) -2.370 0.018 梗死容积/% 22.48±11.42 18.95±10.02 26.86±11.64 -3.862 < 0.001 表 3 两组患者LA功能参数比较
Table 3. LA function parameters
X±S, M(P25, P75) 参数 总体(102例) 无MACE组(56例) MACE组(46例) χ2/t/Z值 P值 存储期射血分数/% 41.78±13.68 46.16±13.07 36.36±12.53 4.017 < 0.001 导管期射血分数/% 28.02(16.33,40.12) 33.08(17.00,46.76) 24.00(14.32,34.80) -2.599 0.009 泵血期射血分数/% 15.71(8.80,25.10) 17.81(10.70,26.82) 12.21(7.52,22.15) -1.809 0.059 存储期应变/% 26.58±12.77 30.96±13.12 21.15±10.04 4.482 < 0.001 导管期应变/% 15.33±8.80 18.66±9.53 11.20±5.56 5.169 < 0.001 泵血期应变/% 10.00(6.00,15.75) 11.00(7.75,16.00) 8.00(5.00,14.25) -2.302 0.021 存储期应变率/s 1.50(0.86,2.00) 1.73(1.24,2.20) 1.10(0.69,1.63) -3.803 < 0.001 导管期应变率/s -1.30(-2.00,-0.83) -1.75(-2.70,-1.20) -1.00(-1.32,-0.69) -4.432 < 0.001 泵血期应变率/s -1.30(-1.90,-0.80) -1.50(-2.23,-1.00) -1.10(-1.70,-0.60) -3.212 0.001 LAVmax/BSA/(mL·m-2) 37.11(29.47,47.08) 36.26(29.81,44.62) 37.40(28.48,53.18) -0.307 0.759 LAVmin/BSA/(mL·m-2) 18.85(14.63,29.71) 17.78(14.60,27.82) 22.26(15.43,34.46) -1.603 0.103 LAVpre/BSA/(mL·m-2) 25.96(18.32,36.03) 24.46(17.37,33.27) 27.14(19.57,37.20) -1.253 0.210 LAVmax/BSA:LA最大容积标化值;LAVmin/BSA:LA最小容积标化值;LAVpre/BSA:LA收缩前容积标化值。 表 4 MI患者左心功能与发生MACE的相关性分析
Table 4. The correlation between the CMR parameters and MACE
指标 相关系数rs P值 存储期射血分数 -0.362 < 0.001 导管期射血分数 -0.247 0.009 存储期应变 -0.384 < 0.001 导管期应变 -0.423 < 0.001 泵血期应变 -0.218 0.210 存储期应变率 -0.361 < 0.001 导管期应变率 0.421 < 0.001 泵血期应变率 0.305 0.001 LVEF -0.345 < 0.001 梗死容积 0.346 < 0.001 LVESV/BSA 0.225 0.017 年龄 0.353 < 0.001 表 5 左心参数对MI患者发生MACE预测价值
Table 5. ROC curve analysis
参数 截断值 灵敏度 特异度 AUC 95%CI P值 存储期射血分数 50.81% 0.92 0.44 0.71 0.617~0.792 < 0.001 导管期射血分数 36.37% 0.84 0.45 0.64 0.547~0.731 0.006 存储期应变 22.00% 0.62 0.76 0.72 0.625~0.799 < 0.001 导管期应变 15.00% 0.80 0.65 0.74 0.651~0.820 < 0.001 泵血期应变 8.00% 0.52 0.73 0.63 0.530~0.716 0.019 存储期应变率 1.30 s 0.62 0.71 0.71 0.616~0.791 < 0.001 导管期应变率 -1.50 s 0.78 0.66 0.74 0.653~0.822 < 0.001 泵血期应变率 -1.30 s 0.62 0.70 0.68 0.582~0.762 < 0.001 LVEF 43.20% 0.66 0.65 0.70 0.603~0.780 < 0.001 梗死容积 23.37% 0.66 0.68 0.70 0.606~0.783 < 0.001 LVESV/BSA 39.05 mL/m2 0.70 0.57 0.63 0.534~0.720 0.016 年龄 57岁 0.64 0.75 0.70 0.606~0.783 < 0.001 -
[1] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2020概要[J]. 中国循环杂志, 2021, 36(6): 521-545. doi: 10.3969/j.issn.1000-3614.2021.06.001
[2] Li J, Dharmarajan K, Bai X, et al. Thirty-day hospital readmission after acute myocardial infarction in China[J]. Circ Cardiovasc Qual Outcomes, 2019, 12(5): e005628. doi: 10.1161/CIRCOUTCOMES.119.005628
[3] Cau R, Bassareo P, Suri JS, et al. The emerging role of atrial strain assessed by cardiac MRI in different cardiovascular settings: an up-to-date review[J]. Eur Radiol, 2022, 32(7): 4384-4394. doi: 10.1007/s00330-022-08598-6
[4] 崔越, 曹玉坤, 刘佳, 等. 心脏磁共振T1 mapping和特征追踪技术定量评价肥厚型心肌病患者心肌纤维化和形变[J]. 临床心血管病杂志, 2020, 36(9): 856-862. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202009017.htm
[5] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. J Am Coll Cardiol, 2018, 72(18): 2231-2264. doi: 10.1016/j.jacc.2018.08.1038
[6] Kawel-Boehm N, Bremerich J. The importance of left atrial function after myocardial infarction[J]. Radiology, 2020, 296(2): 310-311. doi: 10.1148/radiol.2020202132
[7] 屈文涛, 康亚宁, 许磊, 等. 高血压并发阵发性心房颤动患者的左房形变功能与血清NT-proBNP的相关性[J]. 临床心血管病杂志, 2021, 37(2): 156-160. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202102014.htm
[8] Park IH, Cho HK, Oh JH, et al. Old age and myocardial injury in ST-segment elevation myocardial infarction[J]. Am J Med Sci, 2021, 362(6): 592-600. doi: 10.1016/j.amjms.2021.06.023
[9] Leng S, Ge H, He J, et al. Long-term prognostic value of cardiac MRI left atrial strain in ST-segment elevation myocardial infarction[J]. Radiology, 2020, 296(2): 299-309. doi: 10.1148/radiol.2020200176
[10] Thadani SR, Shaw RE, Fang Q, et al. Left atrial end-diastolic volume index as a predictor of cardiovascular outcomes: the heart and soul study[J]. Circ Cardiovasc Imaging, 2020, 13(4): e009746. doi: 10.1161/CIRCIMAGING.119.009746
[11] Yilmaz AS, Kahraman F, Ergül E, et al. Left atrial volume index to left ventricular ejection fraction ratio predicted major adverse cardiovascular event in ST-elevated myocardial infarction patients during 8 years of follow-up[J]. J Cardiovasc Echogr, 2021, 31(4): 227-233. doi: 10.4103/jcecho.jcecho_38_21
[12] Kim J, Yum B, Palumbo MC, et al. Left atrial strain impairment precedes geometric remodeling as a marker of post-myocardial infarction diastolic dysfunction[J]. JACC Cardiovasc Imaging, 2020, 13(10): 2099-2113. doi: 10.1016/j.jcmg.2020.05.041
[13] Modin D, Pedersen S, Fritz-Hansen T, et al. Left atrial function determined by echocardiography predicts incident heart failure in patients with STEMI treated by primary percutaneous coronary intervention[J]. J Card Fail, 2020, 26(1): 35-42. doi: 10.1016/j.cardfail.2019.08.014
[14] Hoit BD. Left atrial reservoir strain: its time has come[J]. JACC Cardiovasc Imaging, 2022, 15(3): 392-394. doi: 10.1016/j.jcmg.2021.10.003
[15] Truong VT, Palmer C, Wolking S, et al. Normal left atrial strain and strain rate using cardiac magnetic resonance feature tracking in healthy volunteers[J]. Eur Heart J Cardiovasc Imaging, 2020, 21(4): 446-453.
[16] Pathan F, Zainal Abidin HA, Vo QH, et al. Left atrial strain: a multi-modality, multi-vendor comparison study[J]. Eur Heart J Cardiovasc Imaging, 2021, 22(1): 102-110. doi: 10.1093/ehjci/jez303
[17] Feistritzer HJ, Nanos M, Eitel I, et al. Determinants and prognostic value of cardiac magnetic resonance imaging-derived infarct characteristics in non-ST-elevation myocardial infarction[J]. Eur Heart J Cardiovasc Imaging, 2020, 21(1): 67-76. doi: 10.1093/ehjci/jez165
-




 下载:
下载: