Predictive value of left ventricular global myocardial work on MACE occurrence after emergency PCI in patients with acute myocardial infarction
-
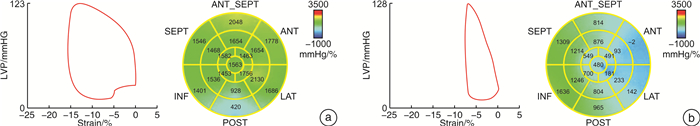
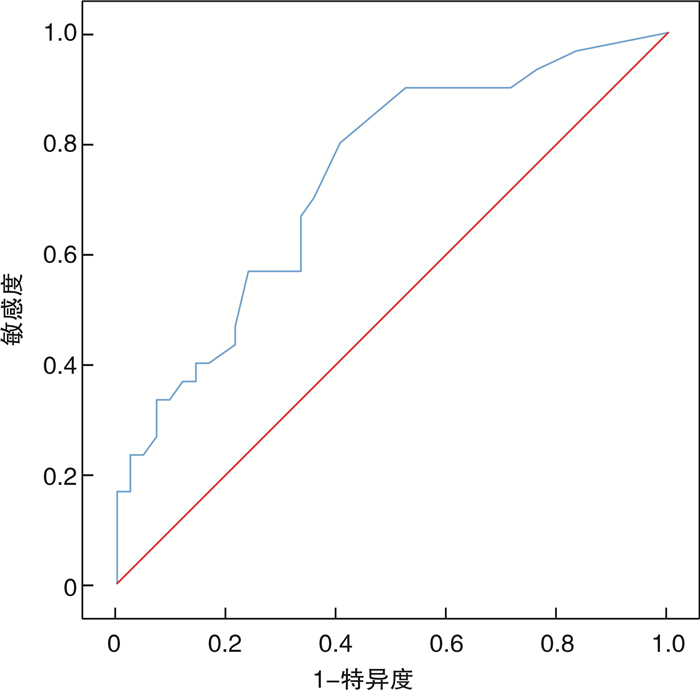
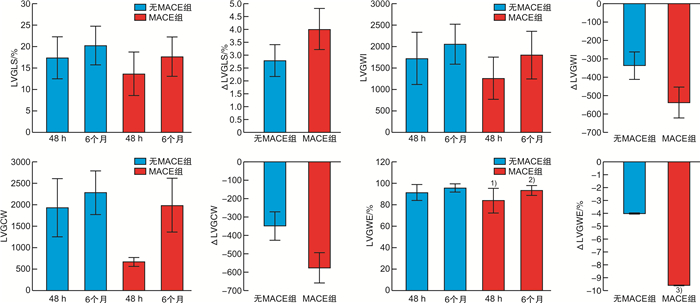
摘要: 目的 应用左室心肌做功(LVGMW)预测急诊经皮冠状动脉介入术(PCI)后的急性心肌梗死(AMI)患者主要不良心脏事件(MACE)的价值。方法 连续选取2019年1月—2020年12月因AMI行急诊PCI的患者73例,男62例,女11例,平均年龄(59.8±11.8)岁,分别在术后48 h内及术后6个月行常规心脏超声、斑点追踪超声(STE)以及LVGMW检查,检测左室射血分数(LVEF)、左室纵向应变(LVGLS)和LVGMW等;平均随访时间9个月,随访期间观察患者是否发生心力衰竭、恶性心律失常、心绞痛、心肌梗死、死亡等MACE,分析LVGMW对MACE的预测价值。结果 随访期间30例患者发生MACE,其中心力衰竭18例、心绞痛12例。MACE组48 h内的左室整体做功效率(LVGWE)明显低于无MACE组[(83.8±11.4)% vs.(91.4±7.3)%,P=0.002];多因素logistic回归分析结果显示,48 h内LVGWE预测AMI患者急诊PCI术后发生MACE的ROC曲线下面积为0.736(95%CI:0.620~0.852,截点为93.5%,敏感度为80.0%,特异度为59.5%,P=0.001)。结论 48 h内的LVGWE是AMI患者急诊PCI术MACE发生的独立预测因子。
-
关键词:
- 左室心肌做功 /
- 左室整体做功效率 /
- 急性心肌梗死 /
- 急诊经皮冠状动脉介入术 /
- 主要不良心脏事件
Abstract: Objective To explore the predictive value of left ventricular global myocardial work (LVGMW) on major adverse cardiac events (MACE) after emergency percutaneous coronary intervention (PCI) in patients with acute myocardial infarction (AMI).Methods From January 2019 to December 2020, 73 consecutive patients (62 males) who underwent emergency PCI for AMI were included with an average age of (59.8±11.8) years old. Conventional cardiac ultrasound and speck tracing ultrasound (STE) were performed within 48 hours and 6 months after PCI, respectively, to detect left ventricular ejection fraction (LVEF), left ventricular end-diastolic volume (LVEDV), longitudinal strain (GLS), and LVGMW. The mean follow-up time was 9 months. During the follow-up period, MACE such as heart failure, malignant arrhythmia, angina pectoris, myocardial infarction, and death were observed. The predictive value of LVGMW on MACE was analyzed.Results During the follow-up period, MACE occurred in 30 patients, heart failure in 18 patients and angina pectoris in 12 patients. LVGWE within 48 hours in the MACE group was significantly lower than that in non-MACE group[(83.8±11.4) % vs. (91.4±7.3) %, P=0.002]. Multivariate logistic regression analysis showed that LVGWE within 48 hours predicted the area under ROC curve of MACE after emergency PCI in AMI patients were 0.736(95%CI: 0.620—0.852, cut-off point 93.5%, sensitivity 80.0%, specificity 59.5%, P=0.001).Conclusion Lower LVGWE within 48 hours was an independent predictor of MACE in AMI patients undergoing emergency PCI. -

-
表 1 两组患者基础资料及治疗情况
Table 1. Comparison of clinical and interventional treatment datas X±S, M(P25, P75)
指标 无MACE组(43例) MACE组(30例) t/χ2/U P值 年龄/岁 57.7±11.4 62.9±11.9 -1.897 0.062 男性/例(%) 36(83.7) 26(86.7) 0.000 0.989 高血压/例(%) 19(44.2) 16(53.3) 1.007 0.218 糖尿病/例(%) 9(20.9) 5(16.7) 0.207 0.654 吸烟/例(%) 27(62.8) 17(56.7) 0.277 0.544 GRACE评分 134.5±25.7 139.9±30.6 -0.806 0.423 心率/(次·min-1) 69.2±14.1 68.5±10.2 -0.843 0.402 甘油三酯/(mmol·L-1) 2.1±1.5 1.6±1.0 1.839 0.070 胆固醇/(mmol·L-1) 5.3±5.7 4.6±1.3 -0.744 0.545 LDL/(mmol·L-1) 2.7±1.0 3.0±1.2 -1.246 0.217 LP-a/(g·L-1) 1.0±0.2 1.0±0.2 -0.026 0.980 GLU/(mmol·L-1) 6.6±2.8 6.7±2.5 -0.126 0.900 肌酐/(μmol·L-1) 73.0±11.6 79.1±22.5 -1.360 0.182 HbA1c/% 7.4±4.6 6.4±1.5 1.044 0.301 肌钙蛋白T/(pg·mL-1) 2124.5(590.6,6045.0) 4175.5(1175.0,9620.5) -1.712 0.087 CKMB/(U·L-1) 100.6±89.4 165.0±194.4 -1.685 0.100 NT-proBNP/(pg·mL-1) 378.3(148.7,812.0) 623.2(208.13,2753.5) -1.547 0.122 犯罪血管LAD/例(%) 20(46.5) 19(63.3) 1.288 0.256 犯罪血管LCX/例(%) 10(23.3) 3(10.0) 2.121 0.145 犯罪血管RCA/例(%) 13(30.2) 8(26.7) 0.110 0.741 BMI/(kg·m-2) 25.0±3.0 26.0±9.6 1.955 0.055 阿司匹林/例(%) 43(100.0) 30(100.0) P2Y12拮抗剂/例(%) 43(100.0) 30(100.0) 他汀/例(%) 43(100.0) 30(100.0) 美托洛尔/例(%) 35(81.4) 24(80.0) 0.022 0.882 ACEI/ARB/例(%) 32(74.4) 19(63.3) 0.628 0.428 注:LDL:低密度脂蛋白;LP-a:脱脂转化酶a;GLU:葡萄糖;HbA1c:糖化血红蛋白;CKMB:肌酸激酶同工酶;NT-proBNP:N末端脑利钠肽前体。 表 2 两组患者术后48 h及6个月的基础心脏超声比较
Table 2. Comparison of conventional echocardiographic parameters in 48 hours and 6 months after PCI
X±S 项目 无MACE组(43例) MACE组(30例) t值 P值 48 h 6个月 48 h 6个月 48 h 6个月 48 h 6个月 左房内径/mm 35.9±6.9 36.4±3.7 37.4±3.4 37.1±3.7 -1.157 -0.826 0.251 0.412 室间隔厚度/mm 10.0±1.3 9.6±1.0 10.1±1.8 9.8±1.4 -0.403 -0.539 0.688 0.591 LVEDD/mm 49.8±4.3 49.6±4.3 51.0±5.9 49.6±5.5 -0.986 -0.051 0.327 0.960 左室后壁厚度/mm 9.7±1.0 9.5±0.7 9.6±1.2 9.6±1.0 0.130 -0.436 0.897 0.664 LVESD/mm 34.9±5.2 33.3±4.4 38.2±6.4 34.0±5.8 -2.340 -0.488 0.022 0.628 LVEF/% 54.6±7.9 61.1±6.1 50.4±8.2 59.3±7.6 2.121 1.053 0.038 0.296 肺动脉压/mmHg 25.3±5.1 24.5±4.1 29.0±6.2 25.9±6.6 -2.691 -1.095 0.009 0.277 E/A 1.1±0.4 1.0±0.2 1.0±0.7 0.9±0.5 0.812 0.188 0.420 0.852 下腔/mm 14.3±4.0 10.3±3.7 15.5±4.8 11.6±4.1 -1.117 -1.285 0.268 0.203 表 3 两组患者术后48 h、6个月的GLS及做功的比较
Table 3. Comparison of LVGLS and LVGMW in 48 hours and 6 months after PCI
X±S 项目 无MACE组(43例) MACE组(30例) t值 P值 48 h 6个月 48 h 6个月 48 h 6个月 48 h 6个月 LVGLS/% 17.4±4.9 20.3±4.5 13.7±5.1 17.7±4.6 -3.106 -2.351 0.003 0.021 LVGWI/mmHg% 1716.5±606.1 2049.8±460.2 1258.5±491.1 1797.6±556.4 3.426 2.113 0.001 0.038 LVGCW/mmHg% 1931.9±675.6 2279.2±508.7 675.6±103.0 1981.2±619.5 3.550 2.250 0.001 0.028 LVGWW/mmHg% 126.5±163.5 69.02±53.8 163.5±24.9 90.8±63.3 -0.805 -1.582 0.424 0.118 LVGWE/% 91.4±7.3 95.6±3.6 83.8±11.4 93.0±4.6 3.218 2.269 0.002 0.026 表 4 两组患者48 h内的LVGW、GLS与随访6个月的LVGW、GLS差值比较
Table 4. Comparison of ΔLVGLS and ΔLVGMW in 48 hours and 6 months after PCI
X±S 项目 无MACE组(43例) MACE组(30例) t值 P值 ΔLVGLS/% 2.86±0.64 4.00±0.79 -1.120 0.267 ΔLVGWI/mmHg% -333.33±71.31 -539.07±80.91 1.889 0.063 ΔLVGCW/mmHg% -347.21±77.97 -575.57±92.96 1.881 0.064 ΔLVGWW/mmHg% 57.44±25.39 63.17±18.58 -0.168 0.867 ΔLVGWE/% -4.05±0.90 -9.60±1.97 2.560 0.014 注:ΔLVGLS:48 h内与6个月LVGLS的差值;ΔLVGWI:48 h内与6个月LVGWI的差值;ΔLVGCW:48 h内与6个月LVGCW的差值;ΔLVGWW:48 h内与6个月LVGWW的差值;ΔLVGWE:48 h内与6个月LVGWE的差值。 表 5 影响急诊PCI术后AMI患者MACE发生单因素和多因素logistic回归分析
Table 5. Univariate and multivariate logistic regression analyses of MACE
变量 单因素回归分析 多因素回归分析 B值 OR值 95%CI P值 B值 OR值 95%CI P值 48 h LVGLS 0.148 1.159 1.046~1.285 0.005 - - - - 48 h LVGWI -0.002 0.998 0.997~0.999 0.003 - - - - 48 h LVGCW -0.001 0.999 0.998~0.999 0.002 - - - - 48 h LVGWE -0.087 0.917 0.865~0.971 0.003 -0.08 0.923 0.872~0.978 0.006 6个月LVGLS 0.126 1.134 1.015~1.267 0.027 - - - - 6个月LVGWI -0.001 0.999 0.998~1.000 0.043 - - - - 6个月LVGCW -0.001 0.999 0.998~1.000 0.032 - - - - 6个月LVGWE -0.132 0.876 0.774~0.991 0.035 - - - - ΔLVGWE -8.198 2.75×10-4 4.44×10-7~0.170 0.012 - - - - LVESD 0.112 1.119 1.008~1.242 0.035 - - - - LVEF -0.065 0.937 0.879~0.998 0.044 - - - - 肺动脉压 0.12 1.127 1.024~1.241 0.014 - - - - -
[1] Roth GA, Johnson C, Abajobir A, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015[J]. J Am Coll Cardiol, 2017, 70(1): 1-25. doi: 10.1016/j.jacc.2017.04.052
[2] Chew DS, Heikki H, Schmidt G, et al. Change in Left Ventricular Ejection Fraction Following First Myocardial Infarction and Outcome[J]. JACC Clin Electrophysiol, 2018, 4(5): 672-682. doi: 10.1016/j.jacep.2017.12.015
[3] Pedersen F, Butrymovich V, Kelbæk H, et al. Short-and long-term cause of death in patients treated with primary PCI for STEMI[J]. J Am Coll Cardiol, 2014, 64(20): 2101-2108. doi: 10.1016/j.jacc.2014.08.037
[4] 张梦玮, 王宇, 段洋, 等. TyG指数及TyG指数联合Grace评分对急性心肌梗死患者预后的预测价值[J]. 临床心血管病杂志, 2021, 37(2): 113-117. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202102005.htm
[5] 赵跃华, 王占启, 庞艳彬, 等. 入院时血小板计数与淋巴细胞比值与AMI患者住院期间主要不良心血管事件的相关性[J]. 临床心血管病杂志, 2020, 36(1): 44-50. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202001010.htm
[6] Dokainish H, Rajaram M, Prabhakaran D, et al. Incremental value of left ventricular systolic and diastolic function to determine outcome in patients with acute ST-segment elevation myocardial infarction: the echocardiographic substudy of the OASIS-6 trial[J]. Echocardiography, 2014, 31(5): 569-578. doi: 10.1111/echo.12452
[7] Exner DV, Kavanagh KM, Slawnych MP, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study[J]. J Am Coll Cardiol, 2007, 50(24): 2275-2284. doi: 10.1016/j.jacc.2007.08.042
[8] Parodi G, Memisha G, Carrabba N, et al. Prevalence, predictors, time course, and long-term clinical implications of left ventricular functional recovery after mechanical reperfusion for acute myocardial infarction[J]. Am J Cardiol, 2007, 100(12): 1718-1722. doi: 10.1016/j.amjcard.2007.07.022
[9] Oh PC, Choi IS, Ahn T, et al. Predictors of recovery of left ventricular systolic dysfunction after acute myocardial infarction: from the korean acute myocardial infarction registry and korean myocardial infarction registry[J]. Korean Circ J, 2013, 43(8): 527-533. doi: 10.4070/kcj.2013.43.8.527
[10] Hall TS, Hallén J, Krucoff MW, et al. Cardiac troponin I for prediction of clinical outcomes and cardiac function through 3-month follow-up after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction[J]. Am Heart J, 2015, 169(2): 257-265. e1. doi: 10.1016/j.ahj.2014.10.015
[11] Dagres N, Hindricks G. Risk stratification after myocardial infarction: is left ventricular ejection fraction enough to prevent sudden cardiac death?[J]. Eur Heart J, 2013, 34(26): 1964-1971. doi: 10.1093/eurheartj/eht109
[12] Park JJ, Park JB, Park JH, et al. Global Longitudinal Strain to Predict Mortality in Patients With Acute Heart Failure[J]. J Am Coll Cardiol, 2018, 71(18): 1947-1957. doi: 10.1016/j.jacc.2018.02.064
[13] Cha MJ, Kim HS, Kim SH, et al. Prognostic power of global 2D strain according to left ventricular ejection fraction in patients with ST elevation myocardial infarction[J]. PLoS One, 2017, 12(3): e0174160. doi: 10.1371/journal.pone.0174160
[14] Karlsen S, Dahlslett T, Grenne B, et al. Global longitudinal strain is a more reproducible measure of left ventricular function than ejection fraction regardless of echocardiographic training[J]. Cardiovasc Ultrasound, 2019, 17(1): 18. doi: 10.1186/s12947-019-0168-9
[15] Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging[J]. Eur Heart J Cardiovasc Imaging, 2015, 16(3): 233-270. doi: 10.1093/ehjci/jev014
[16] Boe E, Skulstad H, Smiseth OA. Myocardial work by echocardiography: a novel method ready for clinical testing[J]. Eur Heart J Cardiovasc Imaging, 2019, 20(1): 18-20. doi: 10.1093/ehjci/jey156
[17] Russell K, Eriksen M, Aaberge L, et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work[J]. Eur Heart J, 2012, 33(6): 724-733. doi: 10.1093/eurheartj/ehs016
[18] Manganaro R, Marchetta S, Dulgheru R, et al. Echocardiographic reference ranges for normal non-invasive myocardial work indices: results from the EACVI NORRE study[J]. Eur Heart J Cardiovasc Imaging, 2019, 20(5): 582-590. doi: 10.1093/ehjci/jey188
[19] Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2018, 39(2): 119-177. doi: 10.1093/eurheartj/ehx393
[20] Abou R, Leung M, Goedemans L, et al. Effect of Guideline-Based Therapy on Left Ventricular Systolic Function Recovery After ST-Segment Elevation Myocardial Infarction[J]. Am J Cardiol, 2018, 122(10): 1591-1597. doi: 10.1016/j.amjcard.2018.07.035
[21] Przewlocka-Kosmala M, Marwick TH, Mysiak A, et al. Usefulness of myocardial work measurement in the assessment of left ventricular systolic reserve response to spironolactone in heart failure with preserved ejection fraction[J]. Eur Heart J Cardiovasc Imaging, 2019, 20(10): 1138-1146. doi: 10.1093/ehjci/jez027
[22] Edwards N, Scalia GM, Shiino K, et al. Global Myocardial Work Is Superior to Global Longitudinal Strain to Predict Significant Coronary Artery Disease in Patients With Normal Left Ventricular Function and Wall Motion[J]. J Am Soc Echocardiogr, 2019, 32(8): 947-957. doi: 10.1016/j.echo.2019.02.014
[23] Wang CL, Chan YH, Wu VC, et al. Incremental prognostic value of global myocardial work over ejection fraction and global longitudinal strain in patients with heart failure and reduced ejection fraction[J]. Eur Heart J Cardiovasc Imaging, 2021, 22(3): 348-356. doi: 10.1093/ehjci/jeaa162
[24] Butcher SC, Lustosa RP, Abou R, et al. Prognostic implications of left ventricular myocardial work index in patients with ST-segment elevation myocardial infarction and reduced left ventricular ejection fraction[J]. Eur Heart J Cardiovasc Imaging, 2022, 23(5): 699-707. doi: 10.1093/ehjci/jeab096
[25] Lustosa RP, Butcher SC, van der Bijl P, et al. Global Left Ventricular Myocardial Work Efficiency and Long-Term Prognosis in Patients After ST-Segment-Elevation Myocardial Infarction[J]. Circ Cardiovasc Imaging, 2021, 14(3): e012072. doi: 10.1161/CIRCIMAGING.120.012072
-




 下载:
下载: