Effect of anemia on the prognosis within 3 years in patients undergoing percutaneous coronary intervention
-
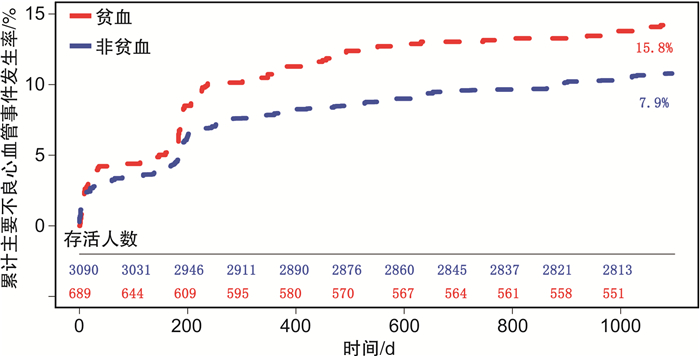
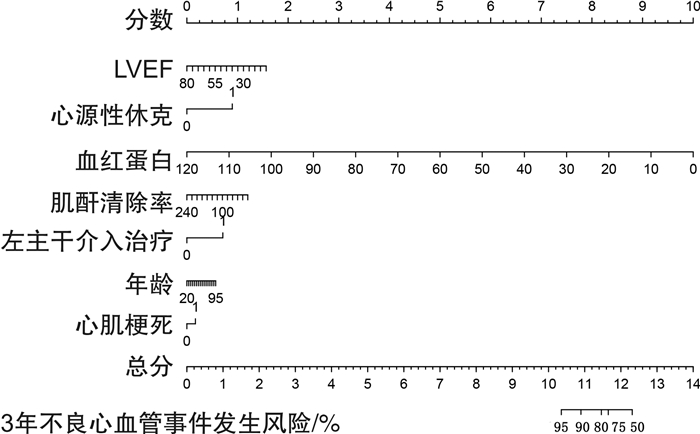
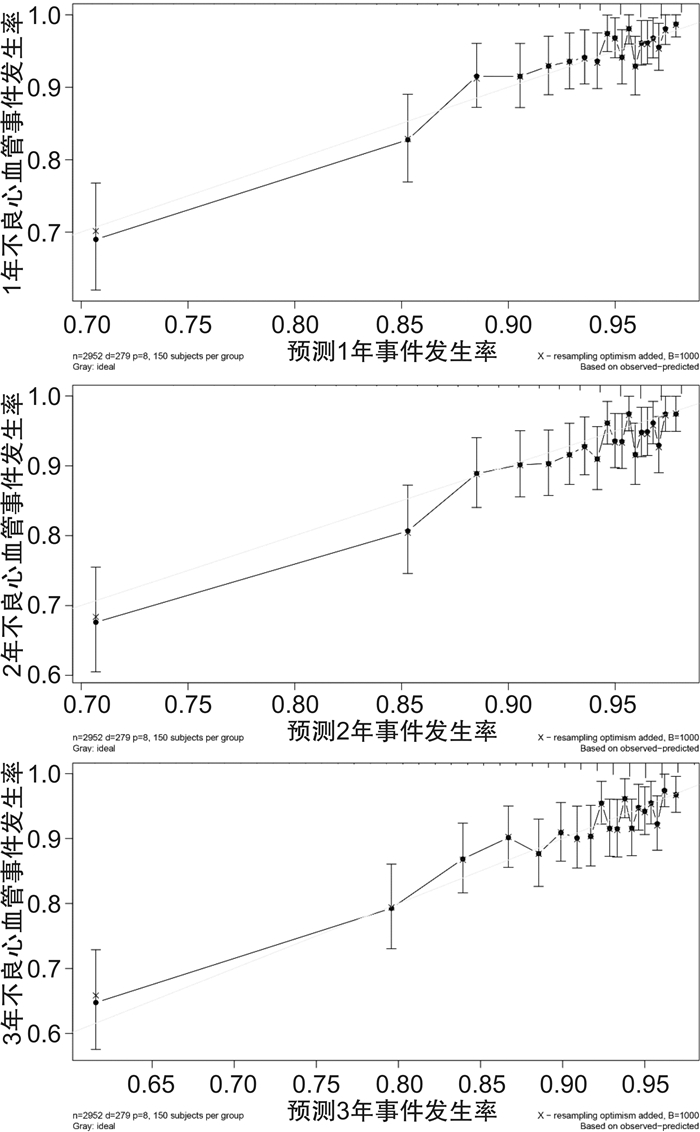
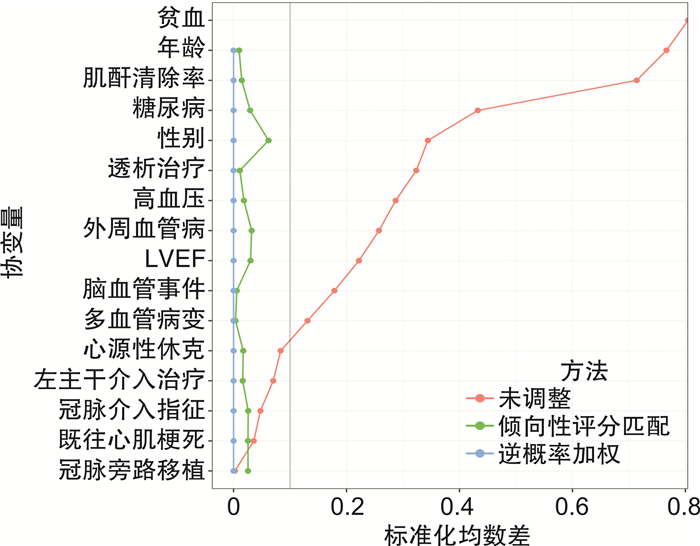
摘要: 目的 探索亚洲人群中贫血对于PCI预后的影响。方法 本研究为前瞻性队列研究,选择2004年1月—2017年12月在韩国高丽大学九老医院行经皮冠状动脉介入治疗(PCI)的患者共4855例。比较贫血组与非贫血组患者PCI治疗后3年预后的差异。研究的主要终点为主要不良心血管事件,包括心血管死亡、靶病变血运重建和心肌梗死的复合终点。结果 排除628例无血红蛋白数值的研究对象后,共入选4227例患者,其中贫血组764例,非贫血组3463例。贫血组合并高血压、脑血管病史等疾病的患者比例较高。随访3年,贫血组发生主要不良心血管事件的风险显著高于非贫血组(HR=2.15,95%CI:1.74~2.67,P < 0.001),并有较高的全因死亡(HR=3.53,95%CI:2.71~4.60,P < 0.001)和靶病变血运重建(HR=1.69,95%CI:1.28~2.45,P < 0.001)风险。倾向性评分匹配、逆概率加权以及多因素Cox回归进一步验证了以上结果。结论 贫血明显增加了PCI术后3年不良心血管事件的发生风险。Abstract: Objective To explore the effect of anemia on the prognosis in patients with percutaneous coronary intervention(PCI) in Asia.Methods The present study was a prospective cohort study involving 4855 patients who underwent PCI at Korea University Guro Hospital from January 2004 to December 2017. Patients were divided into the anemia group and the non-anemia group. The difference of prognosis within 3 years after PCI between the anemia group and the non-anemia group was compared. The primary endpoints were major adverse cardiovascular events(MACE), defined as a composite of cardiac death, target lesion revascularization(TLR), and myocardial infarction(MI).Results A total of 4227 subjects were enrolled after 628 patients without hemoglobin values were excluded, 764 anemia patients were divided into the anemia group and 3463 patients were divided into the non-anemia. The proportion of patients with hypertension and cerebrovascular history in the anemia group was higher than that in the non-anemia group. Following up for 3 years, the risk of MACE was significantly higher in the anemia group than that in the non-anemia group(HR=2.15, 95%CI: 1.74-2.67, P < 0.001), and the anemia group had a higher risk of all-cause death(HR=3.53, 95%CI: 2.71-4.60, P < 0.001) and target lesion revascularization(HR=1.69, 95%CI: 1.28-2.45, P < 0.001). The results were further verified by propensity score matching, inverse probability weighting, and multivariable Cox regression.Conclusion Anemia increases the risk of adverse cardiovascular events in 3 years after PCI.
-

-
表 1 贫血组与非贫血组基线数据资料
Table 1. Baseline characteristics of the anemia group and the non-anemia group
例(%), M(P25, P75) 项目 贫血组(764例) 非贫血组(3463例) P 年龄/岁 71.0(63.3,76.5) 61.9(54.2,70.2) < 0.001 男性 255(55.6) 585(71.2) < 0.001 吸烟 180(23.6) 1198(34.6) < 0.001 PCI指征 < 0.001 急性STEMI 135(17.7) 653(18.9) 急性NSTEMI 159(20.8) 533(15.4) UA 208(27.2) 1184(34.2) SA 193(25.3) 907(26.2) 其他 69(9.0) 186(5.4) 病史 心肌梗死 7(0.9) 45(1.3) 0.790 冠脉旁路移植 4(0.5) 17(0.5) 0.783 高血压 567(74.2) 2129(61.9) < 0.001 糖尿病 383(50.1) 1038(30.3) 0.610 高脂血症 133(17.4) 756(21.8) 0.007 脑血管事件 79(10.3) 182(5.3) < 0.001 周围血管病 64(8.3) 93(2.7) < 0.001 慢性肾脏病 132(17.3) 64(1.8) < 0.001 实验室检查 LVEF/% 56(45,60) 60(51,60) < 0.001 血红蛋白/(g·L-1) 105.0(97.0,112.0) 136.0(127.0,146.0) < 0.001 cTnT/(ng·mL-1) 0.02(0.01,0.30) 0.01(0.01,0.11) < 0.001 LDL-C/(mg·mL-1) 93.0(69.0,120.0) 110.0(85.0,136.0) < 0.001 肌酐/(mg·mL-1) 0.9(0.7,1.4) 0.8(0.7,1.0) < 0.001 介入治疗血管 0.007 左主干 37(4.9) 118(3.4) 右冠脉 182(23.9) 669(19.4) 左前降支 421(55.2) 2023(58.5) 左回旋支 118(15.5) 635(18.4) 中间支 4(0.5) 11(0.3) 多支血管病变 248(32.5) 932(26.9) 0.002 左主干病变 61(8.0) 214(6.2) 0.067 靶病变慢性完全闭塞 54(7.1) 272(7.9) 0.461 钙化病变 54(15.2) 77(9.1) 0.002 应用血管内超声 19(2.5) 46(1.3) 0.018 支架类型a) 0.951 金属裸支架 14(1.8) 54(1.6) 药物洗脱支架 747(98.2) 3389(98.4) 支架长度/mm 33.0(22.0,56.0) 30.0(18.0,48.0) < 0.001 支架内径/mm 3.0(2.7,3.5) 3.0(2.8,3.5) < 0.001 注:a)贫血组另有3例患者植入生物可降解支架。 表 2 贫血组与非贫血组3年临床预后的差异
Table 2. Comparison of clinical outcomes between the anemia group and the non-anemia group
项目 贫血组
(764例)非贫血组
(3463例)未调整 倾向性评分匹配调整 逆概率加权调整 Cox多变量调整 HR(95%CI) P HR(95%CI) P HR(95%CI) P HR(95%CI) P 全因死亡 95
(12.4%)128
(3.7%)3.53
(2.71~4.60)< 0.001 1.35
(0.93~1.95)0.118 3.42
(2.59~4.53)< 0.001 1.44
(1.05~1.98)0.024 心源性死亡 54
(7.1%)72
(2.1%)3.53
(2.48~5.02)< 0.001 1.25
(0.77~2.04)0.365 1.39
(0.92~2.08)0.110 1.22
(0.79~1.89)0.366 心肌梗死 28
(3.7%)73
(2.1%)1.85
(1.20~2.87)0.005 1.32
(0.70~2.49)0.389 1.92
(1.23~3.01)0.004 1.44
(0.86~2.40)0.161 靶病变血运重建 65
(8.5%)187
(5.4%)1.69
(1.28~2.45)< 0.001 1.72
(1.11~2.67)0.015 1.77
(1.32~2.38)< 0.001 1.51
(1.08~2.10)0.015 靶血管血运重建 74
(9.7%)246
(7.1%)1.47
(1.13~1.90)0.004 1.59
(1.07~2.37)0.023 1.51
(1.15~1.98)0.003 1.27
(0.94~1.72)0.119 支架内血栓 16
(2.1%)55
(1.6%)1.38
(0.79~2.40)0.260 1.22
(0.53~1.82)0.646 1.36
(0.75~2.48)0.305 1.21
(0.62~2.35)0.573 主要不良心血管事件 121
(15.8%)273
(7.9%)2.15
(1.74~2.67)< 0.001 1.53
(1.11~2.12)0.009 2.18
(1.73~2.73)< 0.001 1.45
(1.12~1.87)0.004 -
[1] Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention[J]. Circulation, 2019, 140(3): 240-261. doi: 10.1161/CIRCULATIONAHA.119.040167
[2] Cao D, Mehran R, Dangas G, et al. Validation of the academic research consortium high bleeding risk definition in contemporary PCI patients[J]. J Am Coll Cardiol, 2020, 75(21): 2711-2722. doi: 10.1016/j.jacc.2020.03.070
[3] Al-Hijji MA, Gulati R, Lennon RJ, et al. Outcomes of percutaneous coronary interventions in patients with anemia presenting with acute coronary syndrome[J]. Mayo Clin Proc, 2018, 93(10): 1448-1461. doi: 10.1016/j.mayocp.2018.03.030
[4] Hariri E, Hansra B, Barringhaus KG, et al. Trends, predictors, and outcomes associated with 30-day hospital readmissions after percutaneous coronary intervention in a high-volume center predominantly using radial vascular access[J]. Cardiovasc Revasc Med, 2020, 21(12): 1525-1531. doi: 10.1016/j.carrev.2020.05.017
[5] Fu N, Li X, Yang S, et al. Risk score for the prediction of contrast-induced nephropathy in elderly patients undergoing percutaneous coronary intervention[J]. Angiology, 2013, 64(3): 188-194. doi: 10.1177/0003319712467224
[6] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. Circulation, 2018, 138(20): e618-e651.
[7] Cutlip DE, Nakazawa G, Krucoff MW, et al. Autopsy validation study of the academic research consortium stent thrombosis definition[J]. JACC Cardiovasc Interv, 2011, 4(5): 554-559. doi: 10.1016/j.jcin.2011.01.011
[8] Faggioni M, Baber U, Sartori S, et al. Influence of baseline anemia on dual antiplatelet therapy cessation and risk of adverse events after percutaneous coronary intervention[J]. Circ Cardiovasc Interv, 2019, 12(4): e007133. doi: 10.1161/CIRCINTERVENTIONS.118.007133
[9] Hussein A, Awad MS, Sabra AM, et al. Anemia is a novel predictor for clinical ISR following PCI[J]. Egypt Heart J, 2021, 73(1): 40. doi: 10.1186/s43044-021-00163-8
[10] Gao M, Zhang X, Qin L, et al. Discharge hemoglobin association with long-term outcomes of ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention[J]. Cardiovasc Ther, 2020, 2020: 8647837.
[11] Liu Y, Yang YM, Zhu J, et al. Anaemia and prognosis in acute coronary syndromes: a systematic review and meta-analysis[J]. J Int Med Res, 2012, 40(1): 43-55. doi: 10.1177/147323001204000105
[12] Lawler PR, Filion KB, Dourian T, et al. Anemia and mortality in acute coronary syndromes: a systematic review and meta-analysis[J]. Am Heart J, 2013, 165(2): 143-53. e5. doi: 10.1016/j.ahj.2012.10.024
[13] Singh M, Rihal CS, Roger VL, et al. Comorbid conditions and outcomes after percutaneous coronary intervention[J]. Heart, 2008, 94(11): 1424-1428. doi: 10.1136/hrt.2007.126649
[14] Afilalo J, Lauck S, Kim DH, et al. Frailty in older adults undergoing aortic valve replacement: The FRAILTY-AVR Study[J]. J Am Coll Cardiol, 2017, 70(6): 689-700. doi: 10.1016/j.jacc.2017.06.024
[15] Zazzara MB, Vetrano DL, Carfì A, et al. Frailty and chronic disease[J]. Panminerva Med, 2019, 61(4): 486-492.
[16] Cooper HA, Rao SV, Greenberg MD, et al. Conservative versus liberal red cell transfusion in acute myocardial infarction(the CRIT Randomized Pilot Study)[J]. Am J Cardiol, 2011, 108(8): 1108-1111. doi: 10.1016/j.amjcard.2011.06.014
[17] Chatterjee S, Wetterslev J, Sharma A, et al. Association of blood transfusion with increased mortality in myocardial infarction: a meta-analysis and diversity-adjusted study sequential analysis[J]. JAMA Intern Med, 2013, 173(2): 132-139. doi: 10.1001/2013.jamainternmed.1001
-




 下载:
下载: