Correlation between thyroid-stimulating hormone and risk factors and risk of cardiovascular and cerebrovascular diseases in the elderly
-
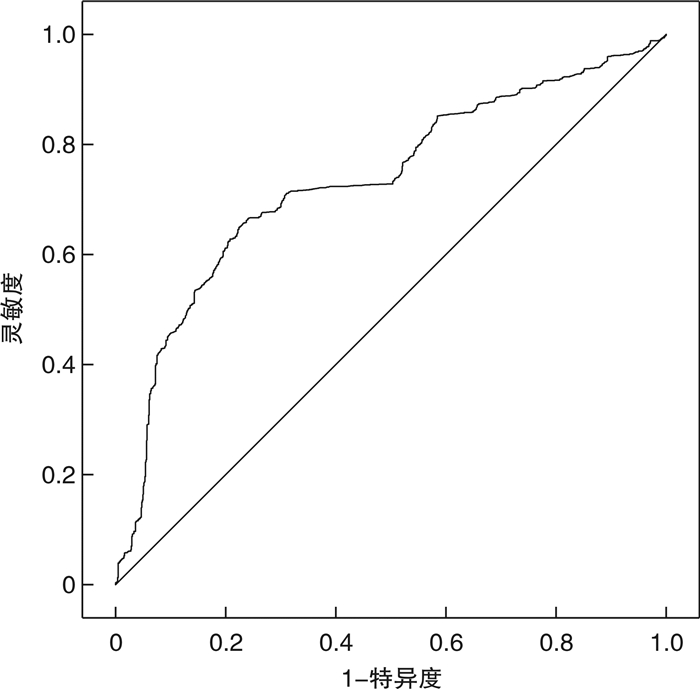
摘要: 目的 评估正常范围内促甲状腺激素(TSH)水平与老年心脑血管病危险因素及患病风险之间的关联。方法 采用回顾性横断面研究分析我院老年心脑血管病患者和健康体检人群的临床资料,基于正常范围内TSH水平分析TSH水平与体重指数(BMI)、高血压、糖尿病、血脂异常等心脑血管病危险因素的相关性。纳入≥60岁以上的研究对象共2 805例,其中心脑血管病患者为观察组(1 756例),健康体检人群为对照组(1 049例),比较分析两组对象的临床资料,采用单因素和多因素logistic回归模型分析老年人发生心脑血管病的影响因素,通过受试者工作特征(ROC)曲线分析正常范围内TSH水平对老年心脑血管病的预测效果。结果 Spearman相关性分析显示,正常范围内TSH水平与血脂异常、总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白胆固醇(LDL-C)均呈正相关(r=0.519、0.475、0.383、0.434,均P<0.001),与高密度脂蛋白胆固醇(HDL-C)呈负相关(r=-0.201,P<0.001)。观察组男性比例、高血压比例、糖尿病比例、血脂异常比例、BMI、TC、LDL-C及TSH水平均显著高于对照组,HDL-C明显低于对照组(均P<0.001)。Logistic回归模型分析发现,老年心脑血管病风险随着正常范围内TSH水平的增加而显著增高(OR=2.920,95%CI:2.560~3.329,P<0.001)。ROC曲线分析表明,正常范围内TSH水平对心脑血管病预测价值的曲线下面积为0.733(95%CI:0.714~0.751)。结论 正常范围内TSH水平与心脑血管病部分危险因素具有相关性,高水平TSH对老年心脑血管病有较佳的预测效果,重视老年人群甲状腺功能的动态检测有助于降低心脑血管病风险。Abstract: Objective To determine the correlation between thyroid-stimulating hormone (TSH) levels within the normal range and risk factors as well as morbidity for cardiovascular and cerebrovascular disease in elderly individuals.Methods A retrospective cross-sectional study was used to analyze the clinical data of elderly patients with cardiovascular and cerebrovascular diseases, as well as a healthy physical examination group in our hospital. The correlation between TSH levels within the normal range and risk factors for cardiovascular and cerebrovascular diseases, including body mass index (BMI), hypertension, diabetes, and dyslipidemia, was analyzed. A total of 2 805 subjects aged ≥ 60 years old were included, with 1 756 patients in the observation group and 1 049 healthy individuals in the control group. The clinical data of the two groups were compared. Univariate and multivariate logistic regression models were used to analyze the influencing factors of cardiovascular and cerebrovascular disease in the elderly. And the predictive effect of TSH level on cardiovascular and cerebrovascular disease in the elderly within normal TSH range was analyzed by the receiver working characteristic (ROC) curve.Results Spearman analysis showed that the TSH level within normal range was positively correlated with dyslipidemia, total cholesterol (TC), triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C) (r=0.519、0.475, 0.383, 0.434, all P<0.001), and negatively correlated with high-density lipoprotein cholesterol (HDL-C) (r=-0.201, P<0.001). The proportion of men, hypertension, diabetes, dyslipidemia, BMI, TC, LDL-C and TSH levels in the observation group were significantly higher than those in the control group, and HDL-C was significantly lower than that in the control group (all P<0.001). Logistic regression model analysis found that the risk of cardiovascular and cerebrovascular diseases in the elderly increased significantly with the increase of TSH level within the normal range (OR=2.920, 95%CI: 2.560-3.329, P<0.001). ROC curve analysis showed that the area under the curve for the predictive value of TSH level within normal range on cardiovascular and cerebrovascular disease was 0.733 (95%CI: 0.714-0.751).Conclusion TSH levels within the normal range is correlated with some risk factors for cardiovascular and cerebrovascular diseases. Elevated TSH levels demonstrate a stronger predictive capacity for cardiovascular and cerebrovascular diseases in the elderly. Monitoring thyroid function dynamically in the elderly population may contribute to a reduced risk of such diseases.
-

-
表 1 对照组和观察组临床资料比较
Table 1. Clinical data
例(%), X±S, M(Q1, Q3) 项目 对照组(1 049例) 观察组(1 756例) 统计量 P值 男性 540(51.48) 979(55.75) 13.509 <0.001 年龄/岁 70.39±7.05 70.83±7.26 1.589 0.112 高血压 408(38.89) 892(50.80) 37.417 <0.001 糖尿病 294(28.03) 693(39.46) 37.672 <0.001 血脂异常 501(47.76) 1065(60.65) 44.242 <0.001 BMI/(kg/m2) 24.63(22.52,26.26) 24.74(22.37,26.82) 2.297 0.022 空腹血糖/(mmol/L) 6.96±2.85 6.99±2.94 0.285 0.776 总胆红素/(μmol/L) 14.58±6.90 14.67±8.05 0.278 0.781 尿酸/(μmol/L) 360.26±108.81 360.81±110.44 0.129 0.898 TC/(mmol/L) 4.28±1.15 4.47±1.40 3.453 <0.001 TG/(mmol/L) 1.36(1.08,1.93) 1.66(1.44,1.86) 1.422 0.155 HDL-C/(mmol/L) 1.28±0.30 1.19±0.26 -8.925 <0.001 LDL-C/(mmol/L) 1.62±0.59 1.82±0.87 16.981 <0.001 ApoA1/(g/L) 1.23(1.11,1.36) 1.22(1.10,1.35) -1.719 0.086 ApoB/(g/L) 1.04±0.19 1.05±0.23 0.283 0.777 TSH/(μIU/L) 1.33(0.92,1.58) 1.98(1.29,2.64) 22.706 <0.001 FT3/(pmol/L) 4.72(4.25,5.13) 4.67(4.27,5.06) -1.349 0.178 FT4/(pmol/L) 14.95(13.60,16.51) 15.09(13.64,16.58) -0.260 0.794 表 2 正常范围内TSH水平与心脑血管病发生关系的logistic回归分析结果
Table 2. The correlation between TSH levels within normal range and cardiovascular and cerebrovascular diseases analyzed by logistic analysis
项目 OR值 95%CI P值 模型1 3.063 2.718~3.450 <0.001 模型2 3.046 2.703~3.432 <0.001 模型3 2.920 2.560~3.329 <0.001 表 3 模型3的logistic回归分析结果
Table 3. Logistic analysis results of the Model 3
变量 OR值 95%CI P值 男性 1.283 1.075~1.531 0.006 BMI 1.005 0.975~1.037 0.729 无高血压 0.622 0.520~0.745 <0.001 无糖尿病 0.617 0.511~0.744 <0.001 TC 1.143 1.070~1.220 <0.001 HDL-C 0.402 0.284~0.569 <0.001 LDL-C 7.072 5.198~9.621 <0.001 ApoA1 1.358 0.872~2.114 0.176 TSH 2.920 2.560~3.329 <0.001 -
[1] Chang YC, Hua SC, Chang CH, et al. High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker[J]. J Clin Med, 2019, 8(6): 817. doi: 10.3390/jcm8060817
[2] Luxia L, Jingfang L, Songbo F, et al. Correlation Between Serum TSH Levels Within Normal Range and Serum Lipid Profile[J]. Horm Metab Res, 2021, 53(1): 32-40. doi: 10.1055/a-1191-7953
[3] Du FM, Kuang HY, Duan BH, et al. Associations Between Thyroid Hormones Within the Euthyroid Range and Indices of Obesity in Obese Chinese Women of Reproductive Age[J]. Metab Syndr Relat Disord, 2019, 17(8): 416-422. doi: 10.1089/met.2019.0036
[4] He W, Li S, Wang B, et al. Dose-response relationship between thyroid stimulating hormone and hypertension risk in euthyroid individuals[J]. J Hypertens, 2019, 37(1): 144-153. doi: 10.1097/HJH.0000000000001826
[5] Jun JE, Jin SM, Jee JH, et al. TSH increment and the risk of incident type 2 diabetes mellitus in euthyroid subjects[J]. Endocrine, 2017, 55(3): 944-953. doi: 10.1007/s12020-016-1221-1
[6] 张丹丹. 邯郸地区妊娠期甲状腺功能正常参考值建立[D]. 河北工程大学, 2020.
[7] 中国超重/肥胖医学营养治疗专家共识编写委员会. 中国超重/肥胖医学营养治疗专家共识(2016年版)[J]. 中华糖尿病杂志, 2016, 8(9): 525-540. doi: 10.3760/cma.j.issn.1674-5809.2016.09.004
[8] 中国老年医学学会高血压分会. 中国老年高血压管理指南2019[J]. 中华高血压杂志, 2019, 27(2): 111-135. doi: 10.16439/j.cnki.1673-7245.2019.02.008
[9] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志, 2021, 13(4): 315-409. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYX202112018.htm
[10] 中国血脂管理指南修订联合专家委员会. 中国血脂管理指南(2023年)[J]. 中华心血管病杂志, 2023, 51(3): 221-255. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202307001.htm
[11] Su X, Chen X, Peng H, et al. Novel insights into the pathological development of dyslipidemia in patients with hypothyroidism[J]. Bosn J Basic Med Sci, 2022, 22(3): 326-339.
[12] van Vliet NA, Bos MM, Thesing CS, et al. Higher thyrotropin leads to unfavorable lipid profile and somewhat higher cardiovascular disease risk: evidence from multi-cohort Mendelian randomization and metabolomic profiling[J]. BMC Med, 2021, 19(1): 266. doi: 10.1186/s12916-021-02130-1
[13] 陈春梅, 刘佳, 贾育梅, 等. 甲状腺功能正常人群血清促甲状腺激素水平与血脂的相关性[J]. 中国心血管杂志, 2020, 25(1): 45-49. doi: 10.3969/j.issn.1007-5410.2020.01.011
[14] Tian L, Song Y, Xing M, et al. A novel role for thyroid-stimulating hormone: up-regulation of hepatic 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase expression through the cyclic adenosine monophosphate/protein kinase A/cyclic adenosine monophosphate-responsive element binding protein pathway[J]. Hepatology, 2010, 52(4): 1401-1409. doi: 10.1002/hep.23800
[15] Moreno-Navarrete JM, Moreno M, Ortega F, et al. TSHB mRNA is linked to cholesterol metabolism in adipose tissue[J]. FASEB J, 2017, 31(10): 4482-4491. doi: 10.1096/fj.201700161R
[16] Zhang X, Song Y, Feng M, et al. Thyroid-stimulating hormone decreases HMG-CoA reductase phosphorylation via AMP-activated protein kinase in the liver[J]. J Lipid Res, 2015, 56(5): 963-971. doi: 10.1194/jlr.M047654
[17] 宋勇峰, 王凯. 甲状腺疾病和脂代谢[J]. 临床心血管病杂志, 2022, 38(9): 692-695. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.09.002
[18] Rizzolo D, Kong B, Taylor RE, et al. Bile acid homeostasis in female mice deficient in Cyp7a1 and Cyp27a1[J]. Acta Pharm Sin B, 2021, 11(12): 3847-3856. doi: 10.1016/j.apsb.2021.05.023
[19] Chambers KF, Day PE, Aboufarrag HT, et al. Polyphenol Effects on Cholesterol Metabolism via Bile Acid Biosynthesis, CYP7A1: A Review[J]. Nutrients, 2019, 11(11): 2588. doi: 10.3390/nu11112588
[20] Song Y, Xu C, Shao S, et al. Thyroid-stimulating hormone regulates hepatic bile acid homeostasis via SREBP-2/HNF-4α/CYP7A1 axis[J]. J Hepatol, 2015, 62(5): 1171-1179. doi: 10.1016/j.jhep.2014.12.006
[21] Santini F, Marzullo P, Rotondi M, et al. Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease[J]. Eur J Endocrinol, 2014, 171(4): R137-152. doi: 10.1530/EJE-14-0067
[22] Reinehr T. Obesity and thyroid function[J]. Mol Cell Endocrinol, 2010, 316(2): 165-171. doi: 10.1016/j.mce.2009.06.005
[23] Yang L, Sun X, Tao H, et al. The association between thyroid homeostasis parameters and obesity in subjects with euthyroidism[J]. J Physiol Pharmacol, 2023, 74(1).
[24] He W, Li S, Wang B, et al. Dose-response relationship between thyroid stimulating hormone and hypertension risk in euthyroid individuals[J]. J Hypertens, 2019, 37(1): 144-153. doi: 10.1097/HJH.0000000000001826
[25] Gu Y, Li H, Bao X, et al. The Relationship Between Thyroid Function and the Prevalence of Type 2 Diabetes Mellitus in Euthyroid Subjects[J]. J Clin Endocrinol Metab, 2017, 102(2): 434-442.
[26] Türemen EE, Çetinarslan B, Şahin T, et al. Endothelial dysfunction and low grade chronic inflammation in subclinical hypothyroidism due to autoimmune thyroiditis[J]. Endocr J, 2011, 58(5): 349-354.
[27] Yang L, Zou J, Zhang M, et al. The relationship between thyroid stimulating hormone within the reference range and coronary artery disease: impact of age[J]. Endocr J, 2013, 60(6): 773-779.
[28] Westerink J, van der Graaf Y, Faber DR, et al. Relation between thyroid-stimulating hormone and the occurrence of cardiovascular events and mortality in patients with manifest vascular diseases[J]. Eur J Prev Cardiol, 2012, 19(4): 864-873.
[29] Reitz C, Kretzschmar K, Roesler A, et al. Relation of plasma thyroid-stimulating hormone levels to vascular lesions and atrophy of the brain in the elderly[J]. Neuroepidemiology, 2006, 27(2): 89-95.
-




 下载:
下载: