Correlation analysis of serum FGF21 level and myocardial fibrosis in patient with acute myocardial infarction and its influence on long-term prognosis
-
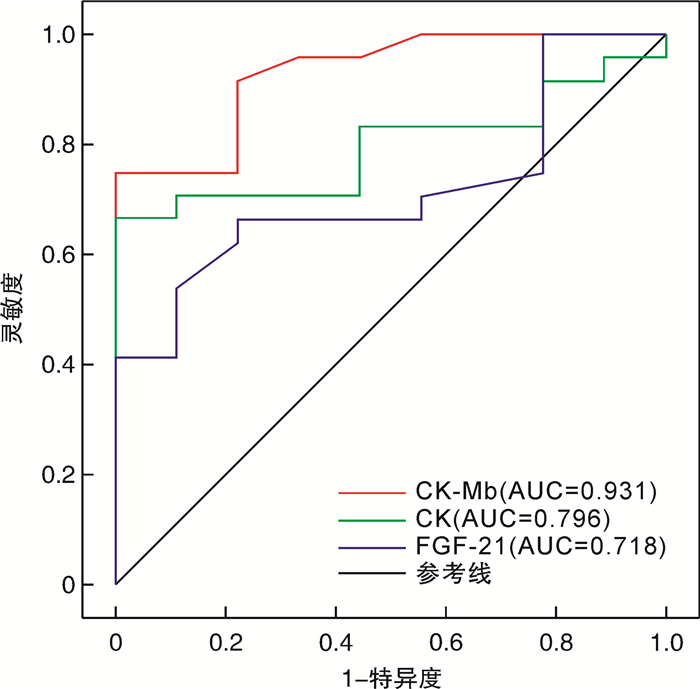
摘要: 目的 研究急性心肌梗死(acute myocardial infarction,AMI)患者中,血清成纤维细胞生长因子21(FGF21)浓度与心肌纤维化程度的相关性,探讨FGF21水平对患者预后的影响。方法 选取2018年1月—2020年12月就诊于上海交通大学医学院附属第九人民医院确诊为AMI的患者24例(AMI组)与健康志愿者18例(对照组)。所有对象均完成心脏磁共振检查,应用第三方软件CVI42分析磁共振图像,分析得出左心室心功能参数及心肌纤维化程度LGE%,并测定血清FGF21浓度,进行统计学分析。进一步根据血清FGF21浓度将AMI组分为FGF21浓度正常组(13例)和增高组(11例),通过住院电子病历系统收集患者的临床资料,电话或门诊随访患者的长期预后,包括心源性死亡、再发心肌梗死、恶性心律失常等不良心血管事件及出院后1年的心脏超声检查结果,随访时间截至2022年12月31日。结果 ① AMI患者的血清FGF21浓度显著高于对照组,差异有统计学意义(P<0.05)。②相关性分析结果显示FGF21浓度与LGE(r=0.763,P<0.01)、LDL(r=0.314,P=0.043)、CK-MB(r=0.444,P<0.01)、CK(r=0.455,P=0.026)呈正相关,与HDL(r=-0.423,P<0.01)呈负相关。在心肌纤维化预测中,FGF21的截断值为0.14 ng/mL时,曲线下面积(AUC)为0.718,灵敏度为66.7%,特异度为77.8%。③预后分析结果发现FGF21增高组与正常组复合终点事件发生率无统计学差异,但FGF21增高组出院后LVEF改善显著,差异有统计学意义(P<0.05)。结论 在AMI患者中,FGF21浓度显著升高,且与心肌纤维化程度具有显著正相关性,同时AMI早期FGF21浓度高对患者长期预后有益。
-
关键词:
- 心脏磁共振 /
- 成纤维细胞生长因子21 /
- 急性心肌梗死 /
- 心肌纤维化
Abstract: Objective To investigate the correlation between serum FGF21 concentration and myocardial fibrosis degree in patients with acute myocardial infarction(AMI), and to explore the effect of FGF21 level on the prognosis of patients.Methods A total of 24 patients diagnosed with AMI(AMI group) and 18 healthy volunteers(control group) were collected. All subjects completed cardiac magnetic resonance examination(CMR), and the third-party software CVI42 was used to analyze the magnetic resonance images, and the left ventricular cardiac function parameters and myocardial fibrosis degree LGE% were analyzed, and the serum FGF21 concentration was measured for statistical analysis. According to serum FGF21 concentration, AMI group was further divided into FGF21 normal group(13 cases) and increased group(11 cases). Clinical data of patients were collected in the inpatient electronic medical record system, and the long-term prognosis of patients was followed up by telephone or outpatient. Adverse cardiovascular events and cardiac ultrasound results were followed up.Results ① The serum FGF21 concentration in AMI patients was significantly higher than that in control group(P<0.05). ②Correlation analysis results showed that FGF21 concentration was positively correlated with LGE(r=0.763, P<0.01), LDL(r=0.314, P=0.043), CK-MB(r=0.444, P<0.01), CK(r=0.455, P=0.026), and HDL(r=-0.423, P=0.026). P<0.01) had a negative correlation. When the cutoff value of FGF21 in the prediction of myocardial fibrosis was 0.14 ng/ml, the area under ROC curve(AUC) was 0.718, with a sensitivity of 66.7% and a specificity of 77.8%. ③The increased group had a significant improvement in LVEF after discharge(P<0.05).Conclusion In AMI patients, the concentration of FGF21 is significantly increased, and has a significant positive correlation with the degree of myocardial fibrosis, and the high concentration of FGF21 in the early stage of MI is beneficial to the long-term prognosis of patients. -

-
表 1 基本信息及心功能参数
Table 1. Basic information and cardiac function parameters
项目 对照组(18例) AMI组(24例) P 年龄/岁 61±9 55±15 0.182 男性 8(44.4) 17(70.8) 0.085 高血压病 6(33.3) 14(58.3) 0.209 糖尿病病 0(0) 9(37.5) 0.005 BMI/(kg/m2) 25.01±2.11 25.53±4.02 0.583 血糖/(mmol/L) 5.1±0.6 7.6±3.3 <0.010 TC/(mmol/L) 4.34±1.26 4.71±1.19 0.336 LDL/(mmol/L) 2.56±1.21 3.13±1.02 0.110 HDL/(mmol/L) 1.39±0.43 1.03±0.44 0.013 TG/(mmol/L) 1.37±0.95 2.15±1.89 0.120 CK-MB/(ng/mL) 15.00±6.1 188.2±191.8 <0.010 CK/(ng/mL) 77.2±25.1 1776.0±2340.7 <0.010 TnI/(ng/mL) 0.14±0.24 17.15±27.98 <0.010 LVEDV/mL 123.6±31.9 133.53±36.82 0.366 LVESV/mL 48.78±16.72 72.75±40.32 0.023 SV/mL 74.81±23.46 60.78±18.67 0.037 HR/(次/min) 65±9 73±15 0.056 CO/(L/min) 4.8±1.3 4.2±1.5 0.173 LVEF/% 60.7±8.9 51.9±11.8 0.011 LVMI/(g/m2) 40.40±11.98 54.58±13.09 <0.010 BNP/(pg/mL) 39.22±33.56 308.45±451.53 <0.010 LGE/% 0.4±0.3 6.8±3.9 <0.010 FGF21/(ng/mL) 0.10±0.06 0.21±0.15 <0.010 例(%),X±S 表 2 FGF21与人体测量参数和生化指标的相关性
Table 2. Correlations of serum FGF21 levels with anthropometric parameters and biochemical indexes
指标 r P LGE 0.763 <0.01 年龄 0.039 0.855 性别 -0.017 0.938 TG 0.130 0.413 TC 0.142 0.507 HDL-C -0.423 <0.01 LDL-C 0.314 0.043 BMI 0.295 0.162 TnI -0.012 0.957 BNP -0.080 0.614 CRP 0.013 0.952 GLU 0.210 0.324 CK-MB 0.444 <0.01 CK 0.455 0.026 LVMI 0.270 0.202 表 3 两组心功能和血清学指标比较
Table 3. Comparison of cardiac function and serological indexes between the two groups
X±S 项目 FGF21正常组(13例) FGF21增高组(11例) P TC/(mmol/L) 4.52±1.19 4.95±1.21 0.395 LDL/(mmol/L) 2.84±0.97 3.48±1.02 0.128 HDL/(mmol/L) 1.13±0.56 0.92±0.23 0.271 TG/(mmol/L) 2.03±2.33 2.20±1.30 0.751 CK-MB/(ng/mL) 90.3±89.4 303.8±218.6 0.010 CK/(ng/mL) 699.9±949.1 3 027.8±2 869.9 0.024 TnI/(ng/mL) 0.14±0.24 17.15±27.98 0.524 BNP /(pg/mL) 432.1±567.9 162.4±196.5 0.129 LVEDV/mL 129.5±26.4 138.4±47.3 0.567 LVESV/mL 70.1±33.2 75.9±49.0 0.735 SV/mL 59.3±17.4 62.5±20.8 0.691 HR/(次/min) 76±16 68±14 0.218 CO/(L/min) 4.1±1.6 4.2±1.5 0.872 LVEF/% 53.7±12.7 49.7±10.7 0.416 Myo-index/(g/m2) 53.05±12.47 56.39±14.18 0.546 LGE/% 4.5±2.6 9.6±3.5 <0.01 表 4 两组患者的心血管结局发生率
Table 4. Incidence of cardiovascular outcomes
例% 结局事件 FGF21正常组(13例) FGF21增高组(11例) P 再发心肌梗死 0 1(9.09) 0.458 不稳定型心绞痛 4(30.8) 5(45.5) 0.751 心力衰竭 3(23.1) 1(9.09) 0.714 恶性心律失常 0 0 1 心源性死亡 0 0 1 复合终点事件 7(53.8) 7(63.6) 0.945 表 5 两组左心功能预后比较
Table 5. Prognostic analysis of left ventricular function between two groups X±S
心功能 FGF21正常组(9例) FGF21增高组(10例) 住院时 出院后 P 住院时 出院后 P SV/mL 59.3±17.4 64.1±11.1 0.461 62.5±20.8 68.4±13.0 0.442 CO/(L/min) 4.14±1.56 5.31±1.55 0.101 4.25±1.49 4.55±0.78 0.566 LVEF/% 53.7±12.7 59.6±8.1 0.235 49.7±10.7 59.8±3.8 0.012 -
[1] Humeres C, Frangogiannis NG. Fibroblasts in the infarcted, remodeling, and failing heart[J]. JACC Basic Transl Sci, 2019, 4(3): 449-467. doi: 10.1016/j.jacbts.2019.02.006
[2] Packer M. What causes sudden death in patients with chronic heart failure and a reduced ejection fraction?[J]. Eur Heart J, 2020, 41(18): 1757-1763. doi: 10.1093/eurheartj/ehz553
[3] Adamczak DM, Oko-Sarnowska Z. Sudden cardiac death in hypertrophic cardiomyopathy[J]. Cardiol Rev, 2018, 26(3): 145-151. doi: 10.1097/CRD.0000000000000184
[4] Thiene G. Ischaemic myocardial fibrosis is the villain of sudden coronary death[J]. Eur Heart J, 2022, 43(47): 4931-4932. doi: 10.1093/eurheartj/ehac571
[5] 万俊, 徐凤, 程景林, 等. 低氧诱导因子1α在急性ST段抬高型心肌梗死患者左心室重构及预后中的作用[J]. 临床急诊杂志, 2022, 23(4): 242-246.
[6] Phan P, Saikia BB, Sonnaila S, et al. The Saga of Endocrine FGFs[J]. Cells, 2021, 10(9): 110.
[7] Bao L, Yin J, Gao W, et al. A long-acting FGF21 alleviates hepatic steatosis and inflammation in a mouse model of non-alcoholic steatohepatitis partly through an FGF21-adiponectin-IL17A pathway[J]. Br J Pharmacol, 2018, 175(16): 3379-3393. doi: 10.1111/bph.14383
[8] Chen A, Liu J, Zhu J, et al. FGF21 attenuates hypoxia-induced dysfunction and apoptosis in HPAECs through alleviating endoplasmic reticulum stress[J]. Int J Mol Med, 2018, 42(3): 1684-1694.
[9] Ma Y, Kuang Y, Bo W, et al. Exercise training alleviates cardiac fibrosis through increasing fibroblast growth factor 21 and regulating TGF-β1-Smad2/3-MMP2/9 signaling in mice with myocardial infarction[J]. Int J Mol Sci, 2021, 22(22): 110.
[10] Li S, Zhu Z, Xue M, et al. Fibroblast growth factor 21 protects the heart from angiotensin Ⅱ-induced cardiac hypertrophy and dysfunction via SIRT1[J]. Biochim Biophys Acta Mol Basis Dis, 2019, 1865(6): 1241-1252. doi: 10.1016/j.bbadis.2019.01.019
[11] Gu L, Jiang W, Zheng R, et al. Fibroblast growth factor 21 correlates with the prognosis of dilated cardiomyopathy[J]. Cardiology, 2021, 146(1): 27-33. doi: 10.1159/000509239
[12] Ferrer-Curriu G, Guitart-Mampel M, Rupérez C, et al. The protective effect of fibroblast growth factor-21 in alcoholic cardiomyopathy: a role in protecting cardiac mitochondrial function[J]. J Pathol, 2021, 253(2): 198-208. doi: 10.1002/path.5573
[13] Lu M, Zhu L, Prasad SK, et al. Magnetic resonance imaging mimicking pathology detects myocardial fibrosis: a door to hope for improving the whole course management[J]. Sci Bull(Beijing), 2023, 68(9): 864-867.
[14] Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology(CSC)guidelines for the diagnosis and management of patients with ST-segment elevation myocardial infarction[J]. Zhonghua Xin Xue Guan Bing Za Zhi, 2019, 47(10): 766-783.
[15] Suomalainen A, Elo JM, Pietiläinen KH, et al. FGF-21 as a biomarker for muscle-manifesting mitochondrial respiratory chain deficiencies: a diagnostic study[J]. Lancet Neurol, 2011, 10(9): 806-818. doi: 10.1016/S1474-4422(11)70155-7
[16] 陈凤英, 邓颖, 李燕, 等. 急性心力衰竭中国急诊管理指南(2022)[J]. 临床急诊杂志, 2022, 23(8): 519-547.
[17] Groenewegen A, Rutten FH, Mosterd A, et al. Epidemiology of heart failure[J]. Eur J Heart Fail, 2020, 22(8): 1342-1356. doi: 10.1002/ejhf.1858
[18] Gil H, Goldshtein M, Etzion S, et al. Defining the timeline of periostin upregulation in cardiac fibrosis following acute myocardial infarction in mice[J]. Sci Rep, 2022, 12(1): 21863. doi: 10.1038/s41598-022-26035-y
[19] Kholmovski EG, Morris AK, Chelu MG. Cardiac MRI and fibrosis quantification[J]. Card Electrophysiol Clin, 2019, 11(3): 537-549. doi: 10.1016/j.ccep.2019.04.005
[20] Zhang W, Chu S, Ding W, et al. Serum level of fibroblast growth factor 21 is independently associated with acute myocardial infarction[J]. PLoS One, 2015, 10(6): e0129791. doi: 10.1371/journal.pone.0129791
[21] Chen H, Lu N, Zheng M. A high circulating FGF21 level as a prognostic marker in patients with acute myocardial infarction[J]. Am J Transl Res, 2018, 10(9): 2958-2966.
[22] Hu X, Yang X, Jiang H. Role of sympathetic nervous system in myocardial ischemia injury: beneficial or deleterious?[J]. Int J Cardiol, 2012, 157(2): 269. doi: 10.1016/j.ijcard.2012.03.016
[23] Sunaga H, Koitabashi N, Iso T, et al. Activation of cardiac AMPK-FGF21 feed-forward loop in acute myocardial infarction: Role of adrenergic overdrive and lipolysis byproducts[J]. Sci Rep, 2019, 9(1): 11841. doi: 10.1038/s41598-019-48356-1
[24] Pöyhönen P, Kylmälä M, Vesterinen P, et al. Peak CK-MB has a strong association with chronic scar size and wall motion abnormalities after revascularized non-transmural myocardial infarction-a prospective CMR study[J]. BMC Cardiovasc Disord, 2018, 18(1): 27. doi: 10.1186/s12872-018-0767-7
[25] Chia S, Senatore F, Raffel OC, et al. Utility of cardiac biomarkers in predicting infarct size, left ventricular function, and clinical outcome after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction[J]. JACC Cardiovasc Interv, 2008, 1(4): 415-423. doi: 10.1016/j.jcin.2008.04.010
[26] Planavila A, Redondo I, Hondares E, et al. Fibroblast growth factor 21 protects against cardiac hypertrophy in mice[J]. Nat Commun, 2013, 4: 2019. doi: 10.1038/ncomms3019
[27] Ferrer-Curriu G, Redondo-Angulo I, Guitart-Mampel M, et al. Fibroblast growth factor-21 protects against fibrosis in hypertensive heart disease[J]. J Pathol, 2019, 248(1): 30-40. doi: 10.1002/path.5226
[28] 于费, 马勇翔, 黄文军, 等. HDL-C水平与冠脉病变严重程度的关系及对介入预后的影响[J]. 临床急诊杂志, 2022, 23(4): 269-273.
[29] Bacmeister L, Schwarzl M, Warnke S, et al. Inflammation and fibrosis in murine models of heart failure[J]. Basic Res Cardiol, 2019, 114(3): 19.
[30] Li J, Gong L, Zhang R, et al. Fibroblast growth factor 21 inhibited inflammation and fibrosis after myocardial infarction via EGR1[J]. Eur J Pharmacol, 2021, 910: 174470.
[31] Bo W, Ma Y, Xi Y, et al. The Roles of FGF21 and ALCAT1 in Aerobic Exercise-Induced Cardioprotection of Postmyocardial Infarction Mice[J]. Oxid Med Cell Longev, 2021, 2021: 8996482.
-




 下载:
下载: