A nomogram to predict the risk of worsening chronic heart failure in the elderly and the predictive value of NT-proBNP
-
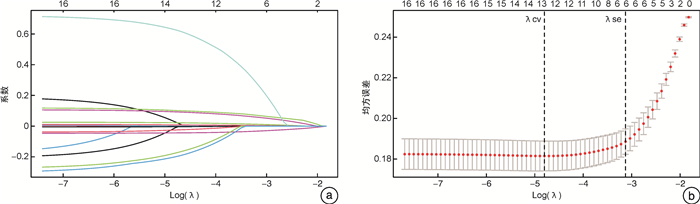
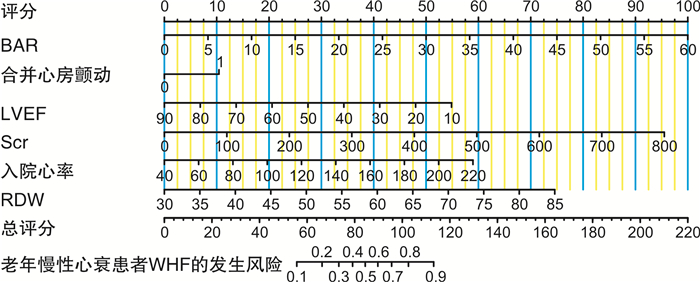
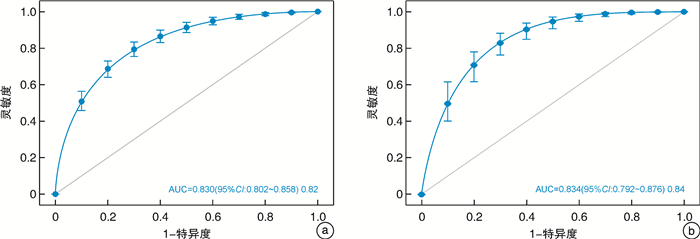
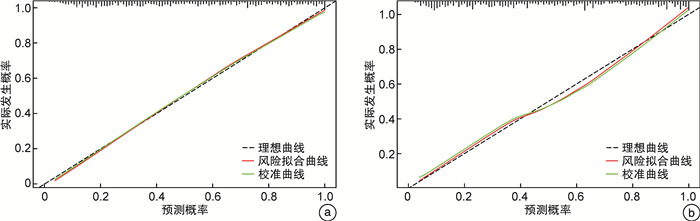
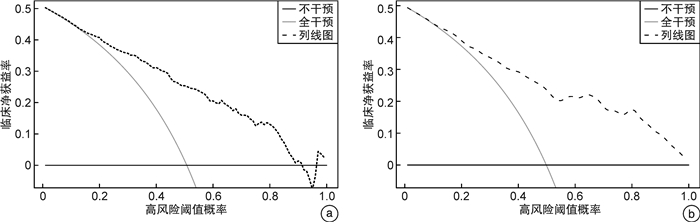
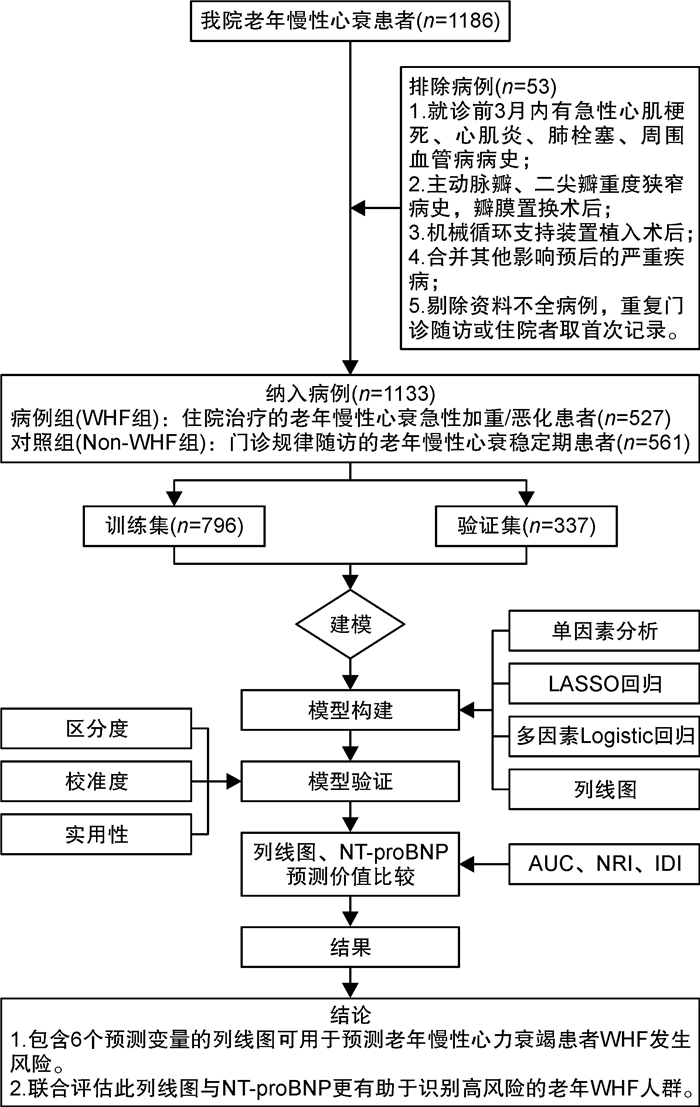
摘要: 目的 构建并验证老年慢性心力衰竭恶化(WHF)的风险预测列线图,并探讨列线图与N末端B型利钠肽前体(NT-proBNP)联合预测WHF的价值。方法 回顾性纳入2018年1月—2022年6月在我院连续就诊的老年WHF患者(WHF组,572例),另纳入同期于我院门诊规律随访的老年慢性心力衰竭稳定期患者561例(Non-WHF组)。比较WHF组与Non-WHF组临床指标的差异。运用LASSO回归联合多因素logistic回归模型构建老年WHF风险预测列线图。由内部验证集评估列线图的可行性,采用受试者工作特征曲线(ROC曲线)、校准曲线和决策曲线(DCA)评价列线图的区分度、校准度及临床实用性。最后通过对比ROC曲线下面积(AUC)、整体鉴别指数(IDI)及净重新分类指数(NRI)来评估列线图、NT-proBNP及其联合使用在老年WHF人群中的预测价值。结果 入院心率、合并心房颤动、左心室射血分数(LVEF)、红细胞分布宽度(RDW)、肌酐(Scr)、血清尿素氮/白蛋白比值(BAR)是WHF发生的独立危险因素(均P<0.05);根据以上6个变量绘制相应的可视化列线图,列线图在训练集和验证集中的AUC分别为0.830(95%CI:0.802~0.858)、0.834(95%CI:0.792~0.876)。DCA提示该列线图的校准度好,临床实用性强。经ROC曲线分析,列线图、NT-proBNP及其联合预测老年WHF的AUC值分别为0.830、0.890和0.924。相对于NT-proBNP,列线图和NT-proBNP联合预测的IDI、NRI分别为0.073、0.065。结论 包含6个预测变量(入院心率、合并心房颤动、LVEF、RDW、Scr和BAR)的列线图可用于预测老年慢性心力衰竭患者WHF发生风险。此列线图与NT-proBNP联合评估更有助于识别高风险的老年WHF人群,协助医务工作者制定临床决策。Abstract: Objective To establish and verify a nomogram for predicting the risk of worsening chronic heart failure(WHF) in elderly patients, as well as to investigate the value of combining the nomogram with N-terminal B-type natriuretic peptide(NT-proBNP) in predicting WHF.Methods We retrospectively reviewed and analyzed the clinical characteristics of 572 elderly patients with WHF(WHF group) and 561 elderly patients with stable chronic heart failure who underwent regular follow-up(Non-WHF group) in our medical center from January 2018 to June 2022. Clinical indexes between the two groups were compared. The elderly WHF nomogram was constructed by LASSO regression combined with multivariate logistic regression analysis. The internal validation set was used to evaluate the feasibility of the nomogram. The receiver operating characteristic curve(ROC), calibration curve, and decision curve analysis(DCA) were adopted to evaluate the discrimination, calibration, and clinical validity of the nomogram. The area under the receiver operating characteristic curve(AUC), integrated discrimination index(IDI), and net reclassification index(NRI) were applied to evaluate the predictive value of the nomogram, NT-proBNP, and their combination in elderly patients with WHF.Results Admission heart rate, concomitant atrial fibrillation, left ventricular ejection fraction, red cell distribution width, creatinine, and blood urea nitrogen/albumin ratio were independent predictors of WHF in elderly patients(P < 0.05). The visual nomogram was drawn based on the six variables, and the AUCs of the nomogram in the training set and validation set were 0.830(95%CI: 0.802-0.858) and 0.834(95%CI: 0.792-0.876). Calibration curves and DCA curves demonstrated perfect calibration and clinical practicability of the nomogram. This study found that the NT-proBNP levels of patients in the WHF group were significantly higher than those in the Non-WHF group(P < 0.001). Meanwhile, the AUCs of the nomogram, NT-proBNP, and their combination were 0.830, 0.890, and 0.924, respectively. Compared with NT-proBNP, the IDI and NRI of their combination were 0.073 and 0.065.Conclusion The nomogram containing six predictors could be used to predict the risk of WHF in elderly patients. The combined assessment of nomogram and NT-proBNP contributes to recognizing the high risk of WHF in elderly patients and helping medical staff to make clinical strategies.
-
Key words:
- elderly /
- chronic heart failure /
- worsening /
- NT-proBNP /
- risk prediction /
- nomogram
-

-
表 1 WHF组与Non-WHF组的临床特征比较
Table 1. Clinical characteristics between the WHF group and Non-WHF group
例(%), X±S, M(P25, P75) 变量 训练集 验证集 WHF组(404例) Non-WHF组(392例) P WHF组(168例) Non-WHF组(169例) P 年龄/岁 79.47±7.72 78.19±9.24 0.772 80.60±10.22 79.67±8.08 0.021 男性 199(49.26) 175(44.64) 0.135 92(54.76) 65(38.46) 0.007 心率/(次/min) 87.81±22.18 78.48±14.55 <0.001 87.56±22.19 78.34±16.66 <0.001 收缩压/mmHg 130.78±24.91 133.45±21.54 0.105 131.86±23.70 135.76±21.71 0.118 舒张压/mmHg 78.11±15.73 77.00±13.50 0.928 77.20±13.88 77.35±14.01 0.136 冠心病 256(63.37) 286(72.96) 0.004 112(66.67) 123(72.78) 0.199 高血压 249(61.63) 287(73.21) 0.030 98(58.33) 115(68.05) <0.001 肺源性心脏病 119(29.46) 106(27.04) 0.094 57(33.93) 36(21.30) 0.232 心肌病 45(11.14) 17(4.34) 0.001 11(6.55) 5(2.96) 0.083 心房颤动 188(46.53) 121(30.87) <0.001 93(55.36) 47(27.81) <0.001 共病数/种 2.47±1.07 2.44±0.94 0.391 2.49±1.02 2.31±0.99 0.384 LAD/mm 42.11±7.43 39.60±6.94 <0.001 42.85±6.72 39.35±6.61 0.001 LVEDD/mm 51.75±10.28 47.49±6.87 <0.001 51.01±9.47 47.65±8.72 <0.001 LVEF/% 56.25±16.58 66.00±11.52 <0.001 56.74±16.59 64.31±12.34 <0.001 Hb/(g/L) 117.75±24.68 122.51±24.72 <0.001 116.65±25.22 122.91±26.87 0.028 WBC/(×109/L) 6.63 (5.26,8.40) 6.06 (4.88,7.91) 0.178 6.51 (5.31,8.62) 6.39 (5.05,8.00) 0.053 RDW/fL 48.0 (45.10,52.30) 45.5 (43.00,47.90) <0.001 47.5 (44.90,51.38) 45.3 (43.40,47.60) <0.001 PDW/fL 15.90 (13.20,16.40) 15.10 (12.33,16.30) 0.318 15.65 (12.40,16.40) 15.60 (12.65,16.40) 0.274 K+/(mmol/L) 4.07 (3.76,4.45) 3.99 (3.71,4.31) <0.001 4.15 (3.74,4.62) 3.95(3.62,4.30) 0.034 Na+/(mmol/L) 139.1 (136.1,141.2) 140.0 (137.1,141.7) 0.050 138.7 (135.8,141.3) 139.9 (137.2,142.1) 0.063 Scr/(μmol/L) 96.80 (73.98,138.85) 77.20 (62.53,100.23) <0.001 91.25 (68.70,140.05) 77.00 (63.65,98.00) <0.001 BAR/(mg/g) 7.15 (5.08,10.55) 5.34 (4.04,6.77) <0.001 7.08 (4.52,10.59) 5.03(3.69,6.34) <0.001 NT-proBNP/(ng/L) 5520.0 (2 482.3,9963.8) 925.5 (366.8,1 800.0) <0.001 4 756.5 (2 319.0,9 291.0) 1 077.0 (424.0,2 042.0) <0.001 表 2 训练集WHF发生风险的多因素logistic回归分析结果
Table 2. Multivariate logistic regression analysis of WHF risk in the elderly in the training set
自变量 回归系数 标准误 Wald χ2 P OR 95%CI 心房颤动 0.797 0.179 4.461 <0.001 2.22 1.56~3.15 心率 0.025 0.005 4.821 <0.001 1.03 1.02~1.04 LVEF -0.052 0.006 -8.286 <0.001 0.95 0.94~0.96 RDW 0.104 0.017 6.07 <0.001 1.11 1.07~1.15 Scr 0.009 0.003 3.611 0.008 1.01 1.00~1.02 BAR 0.127 0.036 3.498 <0.001 1.14 1.06~1.22 常量 -5.842 0.995 -5.870 0.001 - - 表 3 列线图、NT-proBNP及其联合使用在老年WHF人群中的预测价值
Table 3. Predictive value of the nomogram, NT-proBNP, and their combination in the elderly WHF population
项目 AUC 95%CI 灵敏度 特异度 最大约登指数 列线图 0.830 0.802~0.858 0.792 0.719 0.511 NT-proBNP 0.890 0.877~0.909 0.849 0.786 0.635 列线图+NT-proBNP 0.924 0.907~0.942 0.854 0.811 0.665 -
[1] Greene SJ, Bauersachs J, Brugts JJ, et al. Worsening Heart Failure: Nomenclature, Epidemiology, and Future Directions: JACC Review Topic of the Week[J]. J Am Coll Cardiol, 2023, 81(4): 413-424. doi: 10.1016/j.jacc.2022.11.023
[2] Butler J, Djatche LM, Sawhney B, et al. Clinical and Economic Burden of Chronic Heart Failure and Reduced Ejection Fraction Following a Worsening Heart Failure Event[J]. Adv Ther, 2020, 37(9): 4015-4032. doi: 10.1007/s12325-020-01456-1
[3] Ambrosy AP, Parikh RV, Sung SH, et al. Analysis of Worsening Heart Failure Events in an Integrated Health Care System[J]. J Am Coll Cardiol, 2022, 80(2): 111-122. doi: 10.1016/j.jacc.2022.04.045
[4] Butler J, Yang M, Manzi MA, et al. Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection Fraction[J]. J Am Coll Cardiol, 2019, 73(8): 935-944. doi: 10.1016/j.jacc.2018.11.049
[5] 孔洪. 重视慢性心力衰竭恶化的患者管理[J]. 临床心血管病杂志, 2021, 37(4): 289-292. doi: 10.13201/j.issn.1001-1439.2021.04.001
[6] 中华医学会老年医学分会心血管疾病学组, 《老年慢性心力衰竭诊治中国专家共识》编写组. 老年人慢性心力衰竭诊治中国专家共识(2021)[J]. 中华老年医学杂志, 2021, 40(5): 550-561. doi: 10.3760/cma.j.issn.0254-9026.2021.05.002
[7] 中国医师协会检验医师分会心血管专家委员会. B型利钠肽及N末端B型利钠肽前体实验室检测与临床应用中国专家共识[J]. 中华医学杂志, 2022, 102(35): 2738-2754. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYZ201304005.htm
[8] 王华, 梁延春. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYW201910003.htm
[9] Writing Committee, Maddox TM, Januzzi JL Jr, et al. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee[J]. J Am Coll Cardiol, 2021, 77(6): 772-810. doi: 10.1016/j.jacc.2020.11.022
[10] Riley RD, Ensor J, Snell K, et al. Calculating the sample size required for developing a clinical prediction model[J]. BMJ, 2020, 368: m441.
[11] Collins GS, Reitsma JB, Altman DG, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis(TRIPOD): the TRIPOD statement[J]. Ann Intern Med, 2015, 162(1): 55-63. doi: 10.7326/M14-0697
[12] Li C, Chen J, Qin G. Partial Youden index and its inferences[J]. J Biopharm Stat, 2019, 29(2): 385-399. doi: 10.1080/10543406.2018.1535502
[13] Pencina MJ, Sr DRB, Demler OV. Novel metrics for evaluating improvement in discrimination: net reclassification and integrated discrimination improvement for normal variables and nested models[J]. Stat Med, 2012, 31(2): 101-13. doi: 10.1002/sim.4348
[14] Ferrari R, Fox K. Heart rate reduction in coronary artery disease and heart failure[J]. Nat Rev Cardiol, 2016, 13(8): 493-501. doi: 10.1038/nrcardio.2016.84
[15] Alalwan MA, Al-Ohaid F, Alhajjaj HM, et al. Stroke Prevention Therapy and Prevalence of Risk Factors Among Patients With Atrial Fibrillation at King Fahad University Hospital in Al Khobar: A Retrospective, Single-Center Study[J]. Cureus, 2021, 13(1): e12493.
[16] Coll-Vinent B, Varona M, Martin A, et al. Association between acute heart failure and major cardiovascular events in atrial fibrillation patients presenting at the emergency department: an EMERG-AF ancillary study[J]. Eur J Emerg Med, 2021, 28(3): 210-217. doi: 10.1097/MEJ.0000000000000779
[17] Carlisle MA, Fudim M, DeVore AD, et al. Heart Failure and Atrial Fibrillation, Like Fire and Fury[J]. JACC Heart Fail, 2019, 7(6): 447-456. doi: 10.1016/j.jchf.2019.03.005
[18] Santhanakrishnan R, Wang N, Larson MG, et al. Atrial Fibrillation Begets Heart Failure and Vice Versa: Temporal Associations and Differences in Preserved Versus Reduced Ejection Fraction[J]. Circulation, 2016, 133(5): 484-492. doi: 10.1161/CIRCULATIONAHA.115.018614
[19] Ferreira JP, Verdonschot J, Girerd N, et al. Influence of ejection fraction on biomarker expression and response to spironolactone in people at risk of heart failure: findings from the HOMAGE trial[J]. Eur J Heart Fail, 2022, 24(5): 771-778. doi: 10.1002/ejhf.2455
[20] Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in Patients with Heart Failure and Reduced Ejection Fraction[J]. N Engl J Med, 2020, 382(20): 1883-1893. doi: 10.1056/NEJMoa1915928
[21] Lund LH, Pitt B, Metra M. Left ventricular ejection fraction as the primary heart failure phenotyping parameter[J]. Eur J Heart Fail, 2022, 24(7): 1158-1161. doi: 10.1002/ejhf.2576
[22] Silva Litao MK, Kamat D. Back to Basics: Red Blood Cell Distribution Width: Clinical Use beyond Hematology[J]. Pediatr Rev, 2018, 39(4): 204-209. doi: 10.1542/pir.2017-0118
[23] Xanthopoulos A, Tryposkiadis K, Giamouzis G, et al. Larissa Heart Failure Risk Score: a proposed simple score for risk stratification in chronic heart failure[J]. Eur J Heart Fail, 2018, 20(3): 614-616. doi: 10.1002/ejhf.1132
[24] Chen DC, Shlipak MG, Scherzer R, et al. Association of Intra-individual Differences in Estimated GFR by Creatinine Versus Cystatin C With Incident Heart Failure[J]. Am J Kidney Dis, 2022, 80(6): 762-772. doi: 10.1053/j.ajkd.2022.05.011
[25] Bock JS, Gottlieb SS. Cardiorenal syndrome: new perspectives[J]. Circulation, 2010, 121(23): 2592-2600. doi: 10.1161/CIRCULATIONAHA.109.886473
[26] Arques S. Human serum albumin in cardiovascular diseases[J]. Eur J Intern Med, 2018, 52: 8-12. doi: 10.1016/j.ejim.2018.04.014
[27] van Veldhuisen DJ, Ruilope LM, Maisel AS, et al. Biomarkers of renal injury and function: diagnostic, prognostic and therapeutic implications in heart failure[J]. Eur Heart J, 2016, 37(33): 2577-2585. doi: 10.1093/eurheartj/ehv588
[28] Kajimoto K, Sato N, Takano T, et al. eGFR and Outcomes in Patients with Acute Decompensated Heart Failure with or without Elevated BUN[J]. Clin J Am Soc Nephrol, 2016, 11(3): 405-412. doi: 10.2215/CJN.08210815
[29] Lin Z, Zhao Y, Xiao L, et al. Blood urea nitrogen to serum albumin ratio as a new prognostic indicator in critical patients with chronic heart failure[J]. ESC Heart Fail, 2022, 9(2): 1360-1369. doi: 10.1002/ehf2.13825
-

计量
- 文章访问数: 416
- 施引文献: 0



 下载:
下载: