The correlation between neutrophil-to-platelet ratio and premature coronary heart disease
-
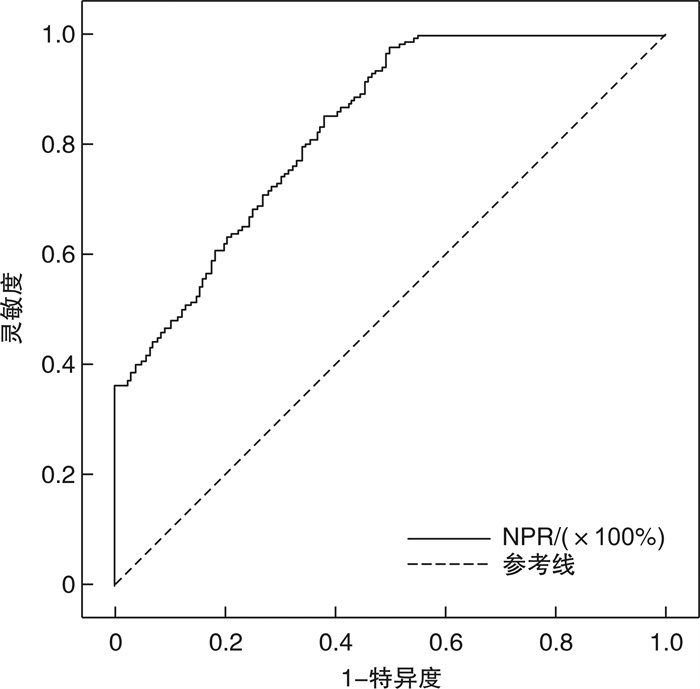
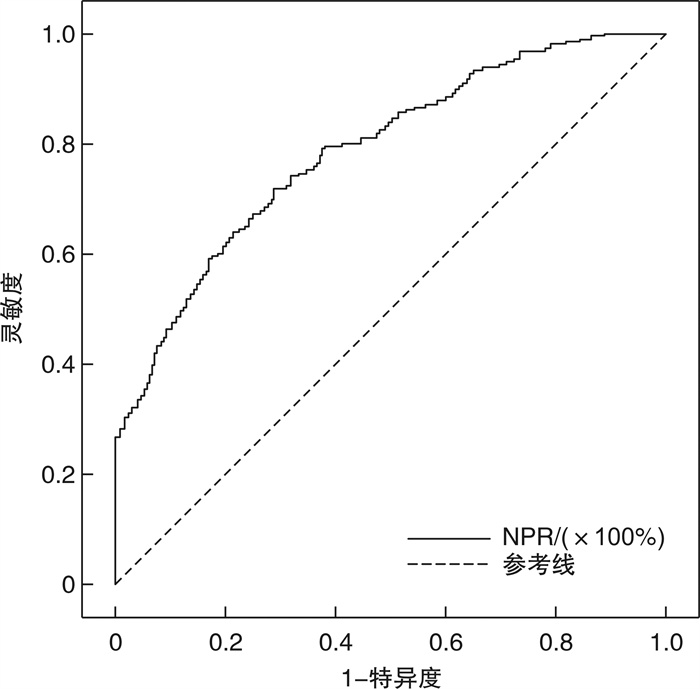
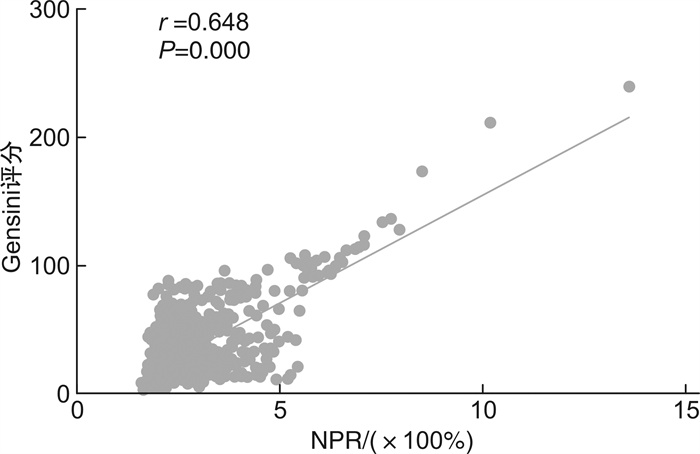
摘要: 目的 评估中性粒细胞与血小板比值(neutrophil to lymphocyte ratio,NPR)与早发冠心病(premature coronary heart disease,PCHD)及冠状动脉(冠脉)病变程度的相关性。 方法 入选于江苏省苏北人民医院住院并首次行冠脉造影检查者共980例(男性 < 55岁,女性 < 65岁),将入组患者分为早发冠心病组(PCHD组,648例)及非冠心病组(NCHD组,332例),并根据Gensini评分将PCHD组患者分为低分组(≤24分)和高分组(>24分),比较各组组间资料的差异性,并运用统计学软件进行统计分析。 结果 ① PCHD组NPR水平显著高于NCHD组(P<0.05),PCHD高分组NPR水平显著高于低分组(P<0.05)。②相关性分析中,NPR水平与Gensini评分呈正相关(r=0.602,P<0.001)。③多因素logistic回归分析显示,高血压病(OR=1.652,95%CI:1.157~2.360,P=0.006)、糖尿病(OR=2.196,95%CI:1.331~3.624,P=0.002)、饮酒史(OR=2.371,95%CI:1.394~4.034,P=0.001)、白细胞(OR=1.286,95%CI:1.064~1.554,P=0.009)及NPR(OR=4.224,95%CI:2.859~6.242,P<0.001)为PCHD患病的独立危险因素;性别(OR=2.105,95%CI:1.330~3.334,P=0.002)、吸烟史(OR=2.427,95%CI:1.545~3.812,P<0.001)、白细胞(OR=1.386,95%CI:1.155~1.663,P<0.001)及NPR(OR=2.389,95%CI:1.808~3.157,P<0.001)为PCHD重度冠脉病变的独立危险因素。④ROC曲线分析中,NPR对PCHD患病有一定的预测价值,曲线下面积(AUC)为0.832,截断值为1.630,灵敏度为0.978,特异度为0.497;NPR对PCHD重度病变具有一定的预测作用,AUC为0.790,截断值为2.522,灵敏度为0.716,特异度为0.719。 结论 在PCHD患者中,NPR水平较高,且NPR越高,冠脉病变程度越重。NPR可在一定程度上预测PCHD的发生以及冠脉病变严重程度。
-
关键词:
- 冠心病,早发 /
- 中性粒细胞与血小板比值 /
- 预测价值
Abstract: Objective To evaluate the correlation between neutrophil to lymphocyte ratio(NPR) and premature coronary heart disease(PCHD) and the degree of coronary artery disease. Methods A total of 980 patients(male < 55 years old, female < 65 years old) who were hospitalized in Northern Jiangsu People's Hospital of Jiangsu Province and underwent coronary angiography for the first time were selected. All enrolled patients were divided into the PCHD group(n=648) and the non-coronary heart disease group(NCHD group, n=332), and according to the Gensini score, patients in the PCHD group were divided into the low score group(≤24 points) and high score group(>24 points). Compare the differences in data between each group, and use statistical software for statistical analysis. Results ① The NPR level of the PCHD group was significantly higher than that of the NCHD group(P < 0.05), and the NPR level of the high score group was higher than that of the low score group(P < 0.05). ②In the correlation analysis, the NPR level was positively correlated with the Gensini score(r=0.602, P < 0.001). ③Multifactor logistic correlation analysis showed that hypertension(OR=1.652, 95%CI: 1.157-2.360, P=0.006), diabetes(OR=2.196, 95%CI: 1.331-3.624, P=0.002), drinking history(OR=2.371, 95%CI: 1.394-4.034, P=0.001), white blood cells(OR=1.286, 95%CI: 1.064-1.554, P=0.009) and NPR(OR=4.224, 95%CI: 2.859-6.242, P < 0.001) were independent risk factors for PCHD; Gender(OR=2.105, 95%CI: 1.330-3.334, P=0.002), smoking history(OR=2.427, 95%CI: 1.545-3.812, P < 0.001), white blood cells(OR=1.386, 95%CI: 1.155-1.663, P < 0.001), and NPR(OR=2.389, 95%CI: 1.808-3.157, P < 0.001) were independent risk factors for severe coronary artery disease in PCHD. ④In the ROC curve analysis, NPR had some values in predicting the prevalence of PCHD. The area under the ROC curve(AUC) was 0.832, the cutoff value was 1.630, the sensitivity was 0.978, and the specificity was 0.497. NPR also has some values in predicting the severe PCHD lesion, the AUC was 0.790, the cutoff value was 2.522, the sensitivity was 0.716, and the specificity was 0.719. Conclusion In patients with PCHD, the level of NPR is high, and the higher the NPR, the more severe the coronary artery disease. NPR predicts the occurrence of PCHD and the severity of coronary artery lesions to a certain extent. -

-
表 1 Gensini评分标准
Table 1. Gensini scoring criteria
病变程度 评分 病变部位 系数 1%~25% 1 左主干 5.0 26%~50% 2 左前降支近段、回旋支近段 2.5 51%~75% 4 左前降支中段 1.5 76%~90% 8 左前降支远段、回旋支中段、回旋支远段 1.0 91%~99% 16 右冠脉、对角支、钝缘支、后降支 1.0 100% 32 其他小分支 0.5 表 2 NCHD组和PCHD组一般资料及实验室指标比较
Table 2. General information and laboratory indicators in the NCHD group and PCHD group
例(%), M(P25, P75) 项目 NCHD组(332例) PCHD组(648例) Z/χ2 P 男性 113(34.0) 354(54.6) 37.322 <0.001 年龄/岁 53(49.0,56.8) 52(48,55) -1.515 0.130 高血压病 124(37.3) 380(58.6) 39.844 <0.001 糖尿病 31(9.3) 165(25.5) 35.678 <0.001 吸烟史 55(16.6) 277(42.7) 67.172 <0.001 饮酒史 28(8.4) 140(21.6) 26.812 <0.001 收缩压/mmHg 129(121.25,140.00) 131(122,142) -1.334 0.182 舒张压/mmHg 78(71,86) 80(74,89) -3.644 <0.001 BMI/(kg/m2) 24.77(22.66,26.67) 25.40(23.67,27.68) -4.216 <0.001 HGB/(g/L) 141(132,153) 146(134,156) -1.937 0.053 PLT/(×109/L) 204(169,240) 198(163,239) -1.689 0.091 WBC/(×109/L) 5.52(4.72,6.50) 7.53(6.03,9.43) -15.155 <0.001 N/(×109/L) 3.34(2.76,4.09) 4.88(3.92,6.64) -15.951 <0.001 L/(×109/L) 1.67(1.38,2.05) 1.72(1.34,2.23) -1.004 0.315 TC/(mmol/L) 4.47(3.79,5.08) 4.45(3.63,5.18) -0.351 0.725 TG/(mmol/L) 1.45(0.99,2.04) 1.80(1.29,2.62) -6.303 0.000 LDL-C/(mmol/L) 2.73(2.04,3.24) 2.64(2.01,3.32) -0.532 0.595 HDL-C/(mmol/L) 1.22(1.01,1.47) 1.01(0.85,1.20) -9.545 0.000 SCr/(μmol/L) 65(56.00,76.45) 69(57,81) -2.874 0.004 NLR 1.98(1.56,2.51) 2.91(2.09,4.06) -12.282 0.000 PLR 119.09(96.09,150.89) 114.83(84.11,150.36) -2.222 0.026 NPR/(×100%) 1.64(1.31,2.10) 2.49(1.97,3.41) -17.018 0.000 表 3 低分组与高分组一般资料及实验室指标比较
Table 3. General information and laboratory indicators in the low score group and high score group
例(%), M(P25, P75) 项目 低分组(342例) 高分组(306例) Z/χ2 P 男性 137(40.1) 217(70.9) 62.039 <0.001 年龄/岁 52.00(48.75,55.00) 52.00(48.00,54.00) -1.074 0.283 高血压病 195(57.0) 185(60.5) 0.788 0.375 糖尿病 78(22.8) 87(28.4) 2.692 0.101 吸烟史 87(25.4) 190(62.1) 88.651 <0.001 饮酒史 68(19.9) 72(23.5) 1.268 0.260 收缩压/mmHg 131(122,142) 130.5(120,142) -1.020 0.308 舒张压/mmHg 80(74,88) 81(74,90) -0.991 0.322 BMI/(kg/m2) 25.35(23.64,27.34) 25.71(23.91,27.76) -1.465 0.143 HGB/(g/L) 145(133,154) 147(135,157) -1.662 0.097 PLT/(×109/L) 202.50(166.75,242.00) 194.00(157.00,232.25) -2.285 0.022 WBC/(×109/L) 6.61(5.61,8.16) 8.51(7.14,10.80) -10.648 <0.001 N/(×109/L) 4.31(3.55,5.50) 5.76(4.47,8.11) -9.783 <0.001 L/(×109/L) 1.71(1.36,2.19) 1.74(1.31,2.31) -0.047 0.962 TC/(mmol/L) 4.35(3.47,5.05) 4.63(3.87,5.32) -3.571 0.000 TG/(mmol/L) 1.78(1.24,2.50) 1.82(1.33,2.69) -1.058 0.290 LDL-C/(mmol/L) 2.46(1.82,3.13) 2.77(2.22,3.43) -4.567 <0.001 HDL-C/(mmol/L) 1.07(0.89,1.27) 0.97(0.81,1.15) -4.610 <0.001 SCr/(μmol/L) 69.00(57.00,80.25) 69.00(57.08,81.08) -0.400 0.689 NLR 2.56(1.92,3.50) 3.41(2.36,5.17) -7.302 <0.001 PLR 115.91(87.00,150.48) 111.38(80.38,150.09) -1.343 0.179 NPR/(×100%) 2.10(1.79,2.63) 3.04(2.41,4.18) -12.746 <0.001 表 4 PCHD患病危险因素的logistic回归分析
Table 4. Risk factors for PCHD analyzed by logistic regression analysis
变量 β OR 95%CI P 高血压病 0.502 1.652 1.157~2.360 0.006 糖尿病 0.787 2.196 1.331~3.624 0.002 饮酒史 0.863 2.371 1.394~4.034 0.001 WBC 0.252 1.286 1.064~1.554 0.009 NPR 1.441 4.224 2.859~6.242 <0.001 表 5 PCHD组冠脉严重程度危险因素的logistic回归分析
Table 5. Risk factors for coronary severity of PCHD analyzed by logistic regression analysis
变量 β OR 95%CI P 男性 0.744 2.105 1.330~3.334 0.002 吸烟史 0.887 2.427 1.545~3.812 <0.001 WBC 0.326 1.386 1.155~1.663 <0.001 NPR 0.871 2.389 1.808~3.157 <0.001 -
[1] Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study[J]. J Am Coll Cardiol, 2020, 76(25): 2982-3021. doi: 10.1016/j.jacc.2020.11.010
[2] Wei A, Liu J, Wang L, et al. Correlation of triglyceride-glucose index and dyslipidaemia with premature coronary heart diseases and multivessel disease: a cross-sectional study in Tianjin, China[J]. BMJ Open, 2022, 12(9): e065780. doi: 10.1136/bmjopen-2022-065780
[3] Xie J, Qi J, Mao H, et al. Coronary plaque tissue characterization in patients with premature coronary artery disease[J]. Int J Cardiovasc Imaging, 2020, 36(6): 1003-1011. doi: 10.1007/s10554-020-01794-9
[4] 徐慧, 刘芳. 早发冠状动脉粥样硬化性心脏病相关危险因素的研究进展[J]. 上海交通大学学报(医学版), 2020, 40(8): 1148-1151. doi: 10.3969/j.issn.1674-8115.2020.08.025
[5] Alan B, Akpolat V, Aktan A, et al. Relationship between osteopenic syndrome and severity of coronary artery disease detected with coronary angiography and Gensini score in men[J]. Clin Interv Aging, 2016, 11: 377-382.
[6] Vasan RS, Song RJ, van den Heuvel ER. Temporal Trends in Incidence of Premature Cardiovascular Disease Over the Past 7 Decades: The Framingham Heart Study[J]. J Am Heart Assoc, 2022, 11(19): e026497. doi: 10.1161/JAHA.122.026497
[7] Chacko M, Sarma PS, Harikrishnan S, et al. Family history of cardiovascular disease and risk of premature coronary heart disease: A matched case-control study[J]. Wellcome Open Res, 2020, 5: 70. doi: 10.12688/wellcomeopenres.15829.2
[8] Person AF, Patterson C. Therapeutic options for premature coronary artery disease[J]. Curr Treat Options Cardiovasc Med, 2008, 10(4): 294-303. doi: 10.1007/s11936-008-0050-9
[9] Li S, Chen H, Zhou L, et al. Neutrophil-to-lymphocyte ratio predicts coronary artery lesion severity and long-term cardiovascular mortality in patients with unstable angina pectoris[J]. Acta Cardiol, 2022, 77(8): 708-715. doi: 10.1080/00015385.2021.1963564
[10] Han M, Sun Y, Li N. Relationship between platelet-to-lymphocyte ratio and Coronary Artery Lesion in non-diabetic patients with coronary heart disease[J]. J Pak Med Assoc, 2022, 72(7): 1426-1428.
[11] 张文婧. 单核细胞与高密度脂蛋白胆固醇比值与早发冠心病严重程度的相关性分析[D]. 山西医科大学, 2022.
[12] Somaschini A, Cornara S, Demarchi A, et al. Neutrophil to platelet ratio: A novel prognostic biomarker in ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention[J]. Eur J Prev Cardiol, 2020, 27(19): 2338-2340. doi: 10.1177/2047487319894103
[13] Li Z, Gao Q, Ren Z, et al. Nomogram based on neutrophil-to-platelet ratio to predict in-hospital mortality in infective endocarditis[J]. Biomark Med, 2021, 15(14): 1233-1243. doi: 10.2217/bmm-2021-0085
[14] Jin P, Li X, Chen J, et al. Platelet-to-neutrophil ratio is a prognostic marker for 90-days outcome in acute ischemic stroke[J]. J Clin Neurosci, 2019, 63: 110-115. doi: 10.1016/j.jocn.2019.01.028
[15] Silvestre-Roig C, Braster Q, Ortega-Gomez A, et al. Neutrophils as regulators of cardiovascular inflammation[J]. Nat Rev Cardiol, 2020, 17(6): 327-340. doi: 10.1038/s41569-019-0326-7
[16] Mandel J, Casari M, Stepanyan M, et al. Beyond Hemostasis: Platelet Innate Immune Interactions and Thromboinflammation[J]. Int J Mol Sci, 2022, 23(7): 3868. doi: 10.3390/ijms23073868
[17] 蒋红周. 术前血红蛋白和血小板对心胸外科围手术期红细胞输注的危险预测[J]. 临床血液学杂志, 2022, 35(6): 439-442. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202206012.htm
[18] 潘宗岱, 薛静, 孙士鹏, 等. 血小板及其衍生物的保存方案和应用进展[J]. 临床血液学杂志, 2022, 35(12): 900-904. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202212015.htm
[19] Lordan R, Tsoupras A, Zabetakis I. Platelet activation and prothrombotic mediators at the nexus of inflammation and atherosclerosis: Potential role of antiplatelet agents[J]. Blood Rev, 2021, 45: 100694.
[20] Kaiser R, Escaig R, Erber J, et al. Neutrophil-Platelet Interactions as Novel Treatment Targets in Cardiovascular Disease[J]. Front Cardiovasc Med, 2021, 8: 824112.
[21] Libby P, Buring JE, Badimon L, et al. Atherosclerosis[J]. Nat Rev Dis Primers, 2019, 5(1): 56.
[22] Stähli BE, Gebhard C, Duchatelle V, et al. Effects of the P-Selectin Antagonist Inclacumab on Myocardial Damage After Percutaneous Coronary Intervention According to Timing of Infusion: Insights From the SELECT-ACS Trial[J]. J Am Heart Assoc, 2016, 5(11): e004255.
[23] Herrero-Cervera A, Soehnlein O, Kenne E. Neutrophils in chronic inflammatory diseases[J]. Cell Mol Immunol, 2022, 19(2): 177-191.
-

计量
- 文章访问数: 306
- 施引文献: 0



 下载:
下载: