The relationship between vegetation size and embolic events, all-cause mortality in infective endocarditis patients: a meta-analysis
-
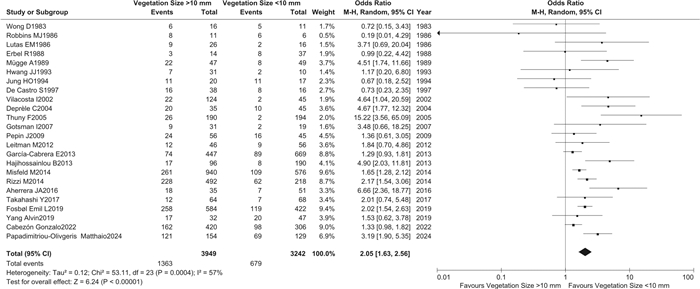
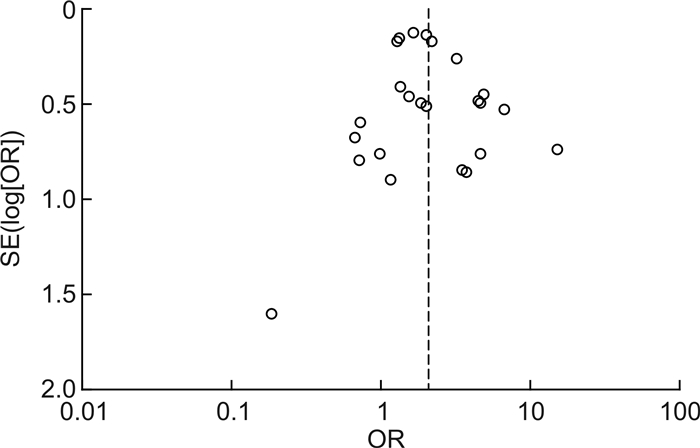
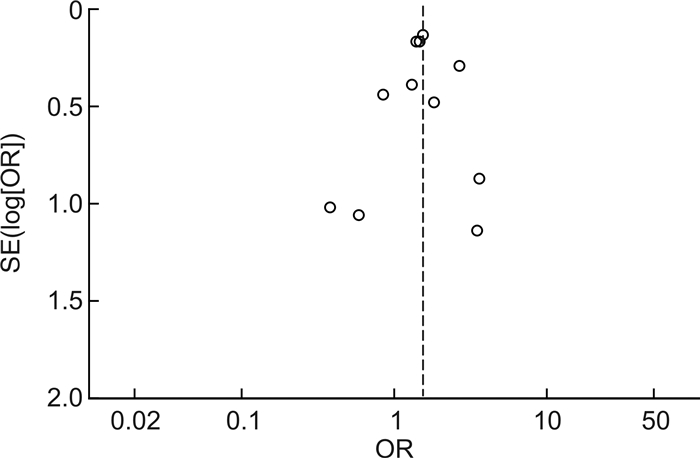
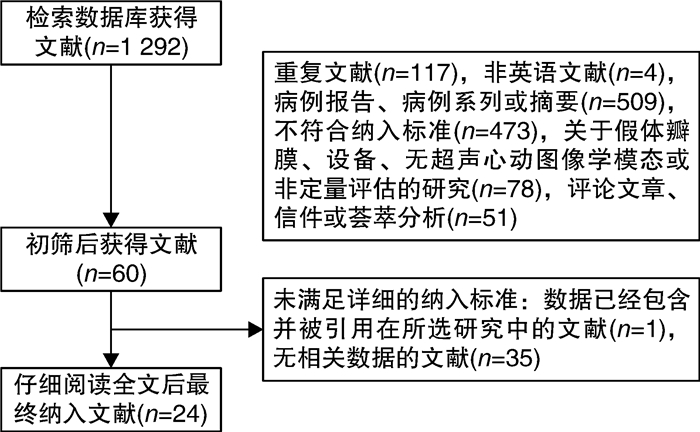
摘要: 目的 评价赘生物大小与感染性心内膜炎患者栓塞事件和全因死亡率的相关性。方法 检索EMBASE、Pubmed、Elservise及Cochrane数据库截至2024年3月提供赘生物≥10 mm与<10 mm两组患者栓塞事件和(或)全因死亡率数据的研究,然后按照Newcastle-Ottawa量表进行严格的文献评价后进行meta分析。结果 纳入24项研究,共8 873例感染性心内膜炎患者,其中7 191例有赘生物大小的资料。荟萃分析结果显示,与赘生物<10 mm相比,赘生物≥10 mm明显增加了感染性心内膜炎患者的栓塞事件发生率(OR=2.05,95%CI:1.63~2.56,P<0.001)和全因死亡率(OR=1.51,95%CI:1.28~1.78,P<0.001),这种相关性随着时间的积累越来越明显。结论 赘生物≥10 mm明显增加感染性心内膜炎患者的栓塞事件发生率和全因死亡率。Abstract: Objective To evaluate the correlation between vegetation size and embolism and all-cause mortality in patients with infective endocarditis by meta-analysis.Methods Relevant trials reported before March 2024 were identified in EMBASE, Pubmed, Elservise and Cochrane. The outcomes included the association of a vegetation size ≥10 mm and<10 mm with embolic events and all-cause mortality in patients with infective endocarditis. A meta-analysis was conducted after a rigorous literature evaluation using the Newcastle Ottawa scale.Results Twenty-four studies with a total of 8 873 patients with infective endocarditis were included, of which 7 191 had data on the size of vegetations. The meta-analysis results showed that compared to vegetations<10 mm, vegetations ≥10 mm significantly increased the incidence of embolic events(OR=2.05, 95%CI: 1.63-2.56, P<0.001) and all-cause mortality(OR=1.51, 95%CI: 1.28-1.78, P<0.001) in patients with infective endocarditis. This correlation became increasingly evident over time.Conclusion Vegetation ≥10 mm significantly increases the incidence of embolic events and all-cause mortality in patients with infective endocarditis.
-
Key words:
- infective endocarditis /
- vegetation /
- embolic events /
- all-cause mortality /
- meta-analysis
-

-
表 1 纳入研究的基本特征
Table 1. Basic characteristics of included studies
研究 国家与地区 研究类型 IE样本量/例 有赘生物大小数据/例 栓塞事件类型 Wong 1983[31] 美国 前瞻性 34 27 脾栓塞、脑栓塞、肺栓塞、肾脏栓塞、
骨栓塞Robbins 1986[32] 美国 前瞻性 21 17 肺栓塞 Lutas 1986[33] 美国 回顾性 77 42 - Erbel 1988[34] 美国 前瞻性 96 51 - Mügge 1989[35] 联邦德国 前瞻性 105 96 脾栓塞、脑栓塞、肺栓塞、肾脏栓塞 Hwang 1993[36] 中国台湾 前瞻性 41 41 脾栓塞、脑栓塞、肺栓塞、肾脏栓塞、
四肢栓塞、视网膜动脉栓塞Jung 1994[24] 韩国 回顾性 80 37 脾栓塞、脑栓塞、肺栓塞、肾脏栓塞、四肢栓塞、冠状
动脉栓塞De Castro 1997[37] 意大利 前瞻性 57 54 外周动脉栓塞、脑栓塞、肺栓塞、冠状
动脉栓塞Vilacosta 2002[38] 阿根廷 前瞻性 211 169 脾栓塞、脑栓塞、肾脏栓塞、四肢栓塞 Deprèle 2004[39] 法国 回顾性 80 80 皮肤栓塞、脑栓塞、肺栓塞、冠状
动脉栓塞、脾栓塞、肾脏栓塞Thuny 2005[19] 法国+意大利 前瞻性 384 384 外周动脉栓塞、脑栓塞、肺栓塞、冠状
动脉栓塞、脾栓塞、肾脏栓塞、视网膜
动脉栓塞Gotsman 2007[40] 以色列 回顾性 100 50 动脉栓塞、脑出血、肺栓塞、感染性动
脉瘤Pepin 2009[41] 加拿大 回顾性 241 101 缺血性脑栓塞、冠状动脉栓塞、脾栓
塞、肾脏栓塞、肠系膜动脉栓塞、其他
外周动脉栓否塞Leitman 2012[42] 以色列 回顾性 146 102 脾栓塞、脑栓塞、肺栓塞、肾脏栓塞、
四肢栓塞、冠状动脉栓塞;感染性关
节炎、感染性动脉瘤;脑出血Hajihossainlou 2013[20] 伊朗 回顾性 286 286 脑栓塞 García-Cabrera 2013[43] 西班牙 前瞻性 1345 1116 缺血性脑栓塞 Misfeld 2014[18] 德国 回顾性 1571 1516 脑栓塞 Rizzi 2014[44] 意大利 回顾性 1456 710 脾栓塞、脑栓塞、肺栓塞、四肢栓塞 Aherrera 2016[45] 菲律宾 前瞻性 87 86 肺栓塞、动脉栓塞、感染性动脉瘤、脑
出血Fosbøl 2019[25] 欧洲 前瞻性 1006 1006 脑栓塞、动脉栓塞 Takahashi 2017[17] 日本 回顾性 166 132 脾栓塞、脑栓塞、四肢栓塞、冠状动脉
栓塞Yang 2019[28] 加拿大 回顾性 116 79 脾栓塞、脑栓塞、四肢栓塞、肠道动脉
栓塞Cabezón 2022[29] 西班牙 回顾性 726 726 外周动脉栓塞、脑栓塞、肺栓塞、肝动
脉栓塞、脾栓塞、肾脏栓塞Papadimitriou-Olivgeris 2024[30] 瑞士 双向性 441 283 皮肤栓塞、外周动脉栓塞、脑栓塞、肺
栓塞、肝动脉栓塞、脾栓塞、肾脏栓
塞、视网膜动脉栓塞、感染性关节炎、
感染性动脉瘤、脑脓肿、脑出血,脉络
膜视网膜炎、球结膜出血、甲床出血研究 IE累及的瓣膜 IE诊断标准 金葡菌
菌血症栓塞事件
是否区分
超声前后赘生物测
量是否使
用TEEWong 1983[31] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜 同时存在至少3项:发热、反流
性杂音、栓塞表现或菌血症16/34
(47.1%)否 否 Robbins 1986[32] 三尖瓣和肺动脉瓣的自体瓣膜或人工瓣
膜主要标准:超声心动图提示赘
生物、发热;次要标准:菌血
症、栓塞事件、心脏杂音(需要
2个主要标准或1个主要标准
+3个次要标准)11/23
(47.8%)否 否 Lutas 1986[33] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜- 血培养22/76
(28.9%)否 否 Erbel 1988[34] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜至少1项:持续性发热、间断性
寒战、夜间盗汗、关节痛、心脏
杂音、栓塞表现- 否 是(100%) Mügge 1989[35] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜临床标准:发热、反流性杂音、
菌血症相关的贫血;手术标本
或尸检组织学标准血培养24/97
(24.74%)是 是(100%) Hwang 1993[36] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜手术标本或尸检组织学标准;
临床可能诊断采用Von Reyn
标准血培养7/50
(14%)否 是(100%) Jung 1994[24] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜或人工瓣膜①术中直接的IE证据或栓塞
物培养阳性;②两次或两次以
上血培养阳性+以下至少3项
标准:发热(>38℃)、心脏基
础疾病、新的反流性杂音、系
统性栓塞、赘生物;③培养阳
性+发热+心脏基础病或新
的反流性杂音;④血培养阴
性:发热+心脏基础病+赘生
物或系统性栓塞血培养12/51
(23.5%)否 否 De Castro 1997[37] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜Duke标准 - 是 是(100%) Vilacosta 2002[38] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 Duke标准 38/211(18%) 是 是(100%) Deprèle 2004[39] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜Duke标准 6/80(7.5%) 是 是(100%) Thuny 2005[19] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜或人工瓣膜Duke标准 82/384(21.4%) 是 是(100%) Gotsman 2007[40] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜Duke标准 16/96(16.7%) 否 是(69%) Pepin 2009[41] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 118/241(49%) 否 - Leitman 2012[42] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜、右心起搏导线/ICD导线心内膜炎Duke标准 否 是(87.25%) Hajihossainlou 2013[20] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜Duke标准 87/286(30.4%) - - García-Cabrera 2013[43] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 263/1 345
(19.6%)否 是(仅部分患者) Misfeld 2014[18] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜或人工瓣膜修订的Duke标准 否 - Rizzi 2014[44] 主动脉瓣、二尖瓣、三尖瓣自体瓣膜或人
工瓣膜、右心起搏导线/ICD导线心内膜炎修订的Duke标准 283/1456(19.4%) 是 - Aherrera 2016[45] 主动脉瓣、二尖瓣、三尖瓣、肺动脉瓣自体
瓣膜或人工瓣膜修订的Duke标准 13/87(14.9%) 否 - Fosbøl 2019[25] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 235/1006(23.36%) 否 - Takahashi 2017[17] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 26/166(15.66%) 是 是(68%) Yang 2019[28] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 27/116(23.28%) 是 是(100%) Cabezón 2022[29] 主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 142/726(19.56%) 否 是(100%) Papadimitriou-Olivgeris
2024[30]主动脉瓣、二尖瓣自体瓣膜或人工瓣膜 修订的Duke标准 164/441(37.19%) 是 是(81%) -
[1] 王世杰, 王寅, 董念国. 《感染性心内膜炎外科治疗中国专家共识》解读[J]. 临床心血管病杂志, 2022, 38(9): 696-699. doi: 10.13201/j.issn.1001-1439.2022.09.003
[2] Cahill TJ, Prendergast BD. Infective endocarditis[J]. Lancet, 2016, 387(10021): 882-893. doi: 10.1016/S0140-6736(15)00067-7
[3] Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications[J]. Circulation, 2015, 132(15): 1435-1486. doi: 10.1161/CIR.0000000000000296
[4] Delgado V, Ajmone Marsan N, de Waha S, et al. ESC Scientific Document Group. 2023 ESC Guidelines for the management of endocarditis[J]. Eur Heart J, 2023, 44(39): 3948-4042. doi: 10.1093/eurheartj/ehad193
[5] Pettersson GB, Coselli JS, Hussain ST, et al. 2016 The American Association for Thoracic Surgery(AATS)consensus guidelines: Surgical treatment of infective endocarditis: Executive summary[J]. J Thorac Cardiovasc Surg, 2017, 153(6): 1241-1258. e29. doi: 10.1016/j.jtcvs.2016.09.093
[6] Nakatani S, Ohara T, Ashihara K, et al. JCS 2017 guideline on prevention and treatment of infective endocarditis[J]. Circ J, 2019, 83(8): 1767-1809. doi: 10.1253/circj.CJ-19-0549
[7] Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease[J]. Circulation, 2021, 143(5): e72-e227.
[8] Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013[J]. JAMA, 2017, 317(16): 1652-1660. doi: 10.1001/jama.2017.4287
[9] Jensen AD, Østergaard L, Petersen JK, et al. Temporal trends of mortality in patients with infective endocarditis: a nationwide study[J]. Eur Heart J Qual Care Clin Outcomes, 2022, 9(1): 24-33. doi: 10.1093/ehjqcco/qcac011
[10] Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study[J]. Arch Intern Med, 2009, 169(5): 463-473. doi: 10.1001/archinternmed.2008.603
[11] Habib G, Erba PA, Lung B, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO(European infective endocarditis)registry: a prospective cohort study[J]. Eur Heart J, 2019, 40(39): 3222-3232. doi: 10.1093/eurheartj/ehz620
[12] Yanagawa B, Pettersson GB, Habib G, et al. Surgical management of infective endocarditis complicated by embolic stroke: practical recommendations for clinicians[J]. Circulation, 2016, 134(17): 1280-1292. doi: 10.1161/CIRCULATIONAHA.116.024156
[13] Cooper HA, Thompson EC, Laureno R, et al. Subclinical brain embolization in left-sided infective endocarditis: results from the evaluation by MRI of the brains of patients with left-sided intracardiac solid masses(EMBOLISM)pilot study[J]. Circulation, 2009, 120(7): 585-591. doi: 10.1161/CIRCULATIONAHA.108.834432
[14] Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis[J]. N Engl J Med, 2012, 366(26): 2466-2473. doi: 10.1056/NEJMoa1112843
[15] Hwang JJ, Shyu KG, Chen JJ, et al. Usefulness of transesophageal echocardiography in the treatment of critically ill patients[J]. Chest, 1993, 104(3): 861-866. doi: 10.1378/chest.104.3.861
[16] Hasbun R, Vikram HR, Barakat LA, et al. Complicated left-sided native valve endocarditis in adults: risk classification for mortality[J]. JAMA, 2003, 289(15): 1933-1940. doi: 10.1001/jama.289.15.1933
[17] Takahashi Y, Izumi C, Miyake M, et al. Diagnostic accuracy of the Embolic Risk French Calculator for symptomatic embolism with infective endocarditis among Japanese population[J]. J Cardiol, 2017, 70(6): 607-614. doi: 10.1016/j.jjcc.2017.04.003
[18] Misfeld M, Girrbach F, Etz CD, et al. Surgery for infective endocarditis complicated by cerebral embolism: a consecutive series of 375 patients[J]. J Thorac Cardiovasc Surg, 2014, 147(6): 1837-1844. doi: 10.1016/j.jtcvs.2013.10.076
[19] Thuny F, Di Salvo G, Belliard O, et al. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study[J]. Circulation, 2005, 112(1): 69-75. doi: 10.1161/CIRCULATIONAHA.104.493155
[20] Hajihossainlou B, Heidarnia MA, Sharif Kashani B. Changing pattern of infective endocarditis in Iran: a 16 years survey[J]. Pak J Med Sci, 2013, 29(1): 85-90.
[21] Tischler MD, Vaitkus PT. The ability of vegetation size on echocardiography to predict clinical complications: a meta-analysis[J]. J Am Soc Echocardiogr, 1997, 10(5): 562-568. doi: 10.1016/S0894-7317(97)70011-7
[22] Mohananey D, Mohadjer A, Pettersson G, et al. Association of vegetation size with embolic risk in patients with infective endocarditis: a systematic review and meta-analysis[J]. JAMA Intern Med, 2018, 178(4): 502-510. doi: 10.1001/jamainternmed.2017.8653
[23] Di Salvo G, Habib G, Pergola V, et al. Echocardiography predicts embolic events in infective endocarditis[J]. J Am Coll Cardiol, 2001, 37(4): 1069-1076. doi: 10.1016/S0735-1097(00)01206-7
[24] Jung HO, Seung KB, Kang DH, et al. A clinical consideration of systemic embolism complicated to infective endocarditis in Korea[J]. Korean J Intern Med, 1994, 9(2): 80-87. doi: 10.3904/kjim.1994.9.2.80
[25] Fosbøl EL, Park LP, Chu VH, et al. The association between vegetation size and surgical treatment on 6-month mortality in left-sided infective endocarditis[J]. Eur Heart J, 2019, 40(27): 2243-2251. doi: 10.1093/eurheartj/ehz204
[26] Sambola A, Lozano-Torres J, Boersma E, et al. Predictors of embolism and death in left-sided infective endocarditis: the European Society of Cardiology Eurobservational Research Programme European Infective Endocarditis registry[J]. Eur Heart J, 2023, 44(43): 4566-4575. doi: 10.1093/eurheartj/ehad507
[27] Song SJ, Kim JH, Ku NS, et al. Vegetation size, multiplicity, and position in patients with infective endocarditis[J]. Ann Thorac Surg, 2022, 114(6): 2253-2260. doi: 10.1016/j.athoracsur.2021.10.071
[28] Yang A, Tan C, Adhikari N, et al. Time-sensitive predictors of embolism in patients with left-sided endocarditis: Cohort study[J]. PLoS One, 2019, 14(4): e0215924. doi: 10.1371/journal.pone.0215924
[29] Cabezón G, López J, Vilacosta I, et al. Reassessment of vegetation size as a sole indication for surgery in left-sided infective endocarditis[J]. J Am Soc Echocardiogr, 2022, 35(6): 570-575. doi: 10.1016/j.echo.2021.12.013
[30] Papadimitriou-Olivgeris M, Guery B, Ianculescu N, et al. Risk of embolicevents before and after antibiotic treatment initiation among patients with left-side infective endocarditis[J]. Infection, 2024, 52(1): 117-128. doi: 10.1007/s15010-023-02066-z
[31] Wong D, Chandraratna AN, Wishnow RM, et al. Clinical implications of large vegetations in infectious endocarditis[J]. Arch Intern Med, 1983, 143(10): 1874-1877. doi: 10.1001/archinte.1983.00350100036011
[32] Robbins MJ, Frater RW, Soeiro R, et al. Influence of vegetation size on clinical outcome of right-sided infective endocarditis[J]. Am J Med, 1986, 80(2): 165-171. doi: 10.1016/0002-9343(86)90004-5
[33] Lutas EM, Roberts RB, Devereux RB, et al. Relation between the presence of echocardiographic vegetations and the complication rate in infective endocarditis[J]. Am Heart J, 1986, 112(1): 107-113. doi: 10.1016/0002-8703(86)90687-3
[34] Erbel R, Rohmann S, Drexler M, et al. Improved diagnostic value of echocardiography in patients with infective endocarditis by transoesophageal approach: a prospective study[J]. Eur Heart J, 1988, 9(1): 43-53. doi: 10.1093/ehj/9.1.43
[35] Mügge A, Daniel WG, Frank G, et al. Echocardiography in infective endocarditis: reassessment of prognostic implications of vegetation size determined by the transthoracic and the transesophageal approach[J]. J Am Coll Cardiol, 1989, 14(3): 631-638. doi: 10.1016/0735-1097(89)90104-6
[36] Hwang JJ, Shyu KG, Chen JJ, et al. Infective endocarditis in the transesophageal echocardiographic era[J]. Cardiology, 1993, 83(4): 250-257. doi: 10.1159/000175978
[37] De Castro S, Magni G, Beni S, et al. Role of transthoracic and transesophageal echocardiography in predicting embolic events in patients with active infective endocarditis involving native cardiac valves[J]. Am J Cardiol, 1997, 80(8): 1030-1034. doi: 10.1016/S0002-9149(97)00598-5
[38] Vilacosta I, Graupner C, San Román JA, et al. Risk of embolization after institution of antibiotic therapy for infective endocarditis[J]. J Am Coll Cardiol, 2002, 39(9): 1489-1495. doi: 10.1016/S0735-1097(02)01790-4
[39] Deprèle C, Berthelot P, Lemetayer F, et al. Risk factors for systemic emboli in infective endocarditis[J]. Clin Microbiol Infect, 2004, 10(1): 46-53. doi: 10.1111/j.1469-0691.2004.00735.x
[40] Gotsman I, Meirovitz A, Meizlish N, et al. Clinical and echocardiographic predictors of morbidity and mortality in infective endocarditis: the significance of vegetation size[J]. Isr Med Assoc J, 2007, 9(5): 365-369.
[41] Pepin J, Tremblay V, Bechard D, et al. Chronic antiplatelet therapy and mortality among patients with infective endocarditis[J]. Clin Microbiol Infect, 2009, 15(2): 193-199. doi: 10.1111/j.1469-0691.2008.02665.x
[42] Leitman M, Dreznik Y, Tyomkin V, et al. Vegetation size in patients with infective endocarditis[J]. Eur Heart J Cardiovasc Imaging, 2012, 13(4): 330-338. doi: 10.1093/ejechocard/jer253
[43] García-Cabrera E, Fernández-Hidalgo N, Almirante B, et al. Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study[J]. Circulation, 2013, 127(23): 2272-2284. doi: 10.1161/CIRCULATIONAHA.112.000813
[44] Rizzi M, Ravasio V, Carobbio A, et al. Predicting the occurrence of embolic events: an analysis of 1456 episodes of infective endocarditis from the Italian Study on Endocarditis(SEI)[J]. BMC Infect Dis, 2014, 14: 230. doi: 10.1186/1471-2334-14-230
[45] Aherrera JA, Abola MT, Balabagno MM, et al. Prediction of symptomatic embolism in Filipinos with infective endocarditis using the embolic risk French calculator[J]. Cardiol Res, 2016, 7(4): 130-139. doi: 10.14740/cr490w
[46] Desch S, Freund A, de Waha S, et al. Outcome in patients with left-sided native-valve infective endocarditis and isolated large vegetations[J]. Clin Cardiol, 2014, 37(10): 626-633. doi: 10.1002/clc.22315
-

计量
- 文章访问数: 234
- 施引文献: 0



 下载:
下载: