-
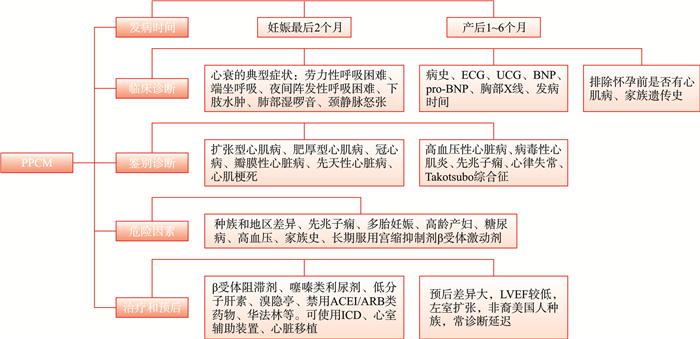
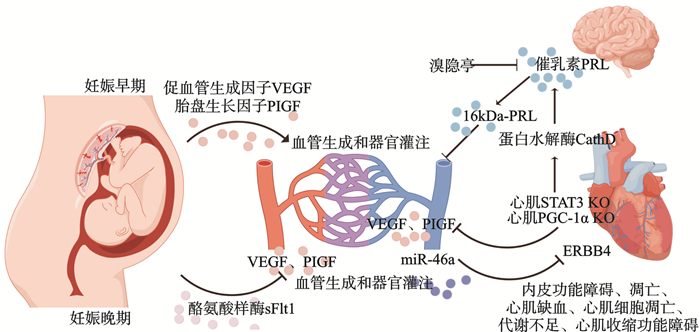
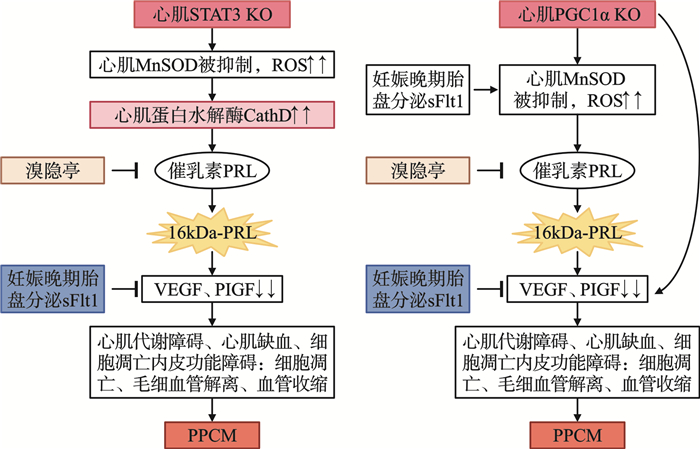
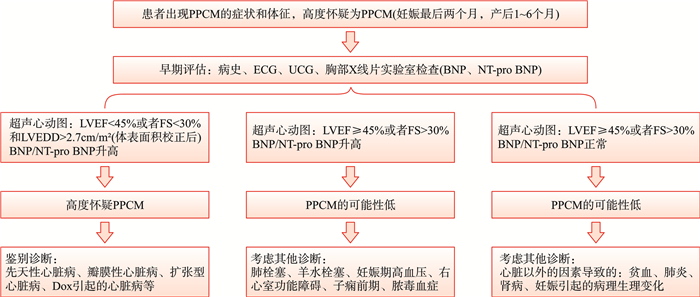
摘要: 围产期心肌病(peripartum cardiomyopathy,PPCM)是在妊娠晚期和分娩后6个月内发生的心肌功能障碍。其发病早期不易诊断,受多种危险因素的影响,病理生理机制复杂,预后差异大,近年来逐渐引起关注。本文将详细综述PPCM在临床表现、诊断、治疗、预后、发病机制和研究现状等方面的进展。Abstract: Peripartum cardiomyopathy(PPCM) is a myocardial dysfunction that occurs in late pregnancy or within 6 months after delivery. The early diagnosis of PPCM is difficult, and the disease is influenced by multiple risk factors, with a complex pathophysiological mechanism and significant variability in prognosis. In recent years, it has gradually attracted attention. This article will comprehensively review the progress of PPCM in clinical manifestations, diagnosis, treatment, prognosis, pathogenesis, and research status.
-
Key words:
- peripartum cardiomyopathy /
- heart failure /
- angiogenesis /
- oxidative stress
-

-
表 1 PPCM的鉴别诊断
Table 1. Differential diagnosis of PPCM
疾病 鉴别要点 发病时间 生物标志物 UCG特点 与PPCM的区别 PPCM 没有已知的心脏病,怀孕前没有心衰体征和(或)症状 妊娠末期和产后1~6个月内 利钠肽、BNP、pro-BNP 左心室收缩功能降低,LVEF < 45% 扩张型心肌病 心衰体征和(或)症状和(或)怀孕前已知的心脏病,劳力性呼吸困难、双下肢水肿、颈静脉怒张、心音增强 怀孕中期 利钠肽 收缩性左心室功能下降,可能出现右心室功能障碍、心室腔扩大、心室壁运动减弱 病史、UCG、心脏MRI 肥厚型心肌病 呼吸困难、胸痛、心室腔变小、室间隔增厚、蹲踞和服用β受体阻滞剂后有好转、青少年运动员和家族遗传史多见 怀孕中期 利钠肽 左心室肥厚,典型的心肌晚期增强模式,左心室流出道梗阻(肥厚型梗阻性心肌病) 病史、UCG、心脏MRI 高血压性心脏病/重度先兆子痫 有长期高血压病史或新发高血压、蛋白尿 怀孕中期 利钠肽 左心室肥厚、舒张功能障碍、一过性左心室功能障碍 病史、UCG 冠心病 劳力型心绞痛、胸痛呈放射性、发病时头晕黑矇,舌下含服硝酸甘油可以缓解、持续时间不超过15 min 怀孕中期 CM-MB、TnI 病史、ECG、冠状动脉造影、心脏MRI 心肌梗死 剧烈胸痛、持续时间大于15 min、舌下含服硝酸甘油不能缓解、呼吸困难、大汗淋漓、恶心呕吐 急性发作、怀孕期间或分娩后立即 CM-MB、TnI 局部室壁运动异常、缺血性心肌瘢痕 病史、ECG、冠状动脉造影、心脏MRI 先兆子痫 孕产妇有高血压、糖尿病、多胎妊娠、流产史 怀孕中期 收缩功能保留 高血压病史、蛋白尿、UCG Takotsubo综合征 胸痛、分娩压力很大或胎儿并发症导致的紧急情况 急性发作、分娩期间或分娩后立即 利钠肽 具有典型解剖模式的区域壁运动异常 病史、UCG 先天性心脏病 可能在妊娠期间首次通过UCG诊断,怀孕前心衰体征和(或)症状、已知心脏病、既往心脏手术 怀孕中期 利钠肽 心脏结构异常或心脏血液反流等 UCG、病史 瓣膜性心脏病 怀孕前的心衰体征和(或)症状,已知的心脏病。UCG检查结果先天性主动脉瓣狭窄、风湿性心脏病引起的二尖瓣狭窄。PPCM患者也可能有瓣膜疾病,即二尖瓣反流 怀孕中期 利钠肽 瓣膜狭窄或反流、人工心脏瓣膜关闭不全 UCG、病史 阿霉素诱导的心肌病 阿霉素药物治疗史、心衰的典型症状 怀孕中期 利钠肽 左心扩大、左心收缩功能降低 UCG、病史 病毒性心肌炎 感染病毒前驱症状、组织学诊断、暴发性表现 病毒感染后急性或亚急性发作 肌钙蛋白和CRP升高 左心室收缩功能正常或降低,典型的心肌晚期钆增强模式,心包积液 心脏MRI、心肌活检 心律失常 存在特定的潜在节律异常,窦性心动过速可能继发于妊娠期心衰 怀孕中期 ECG 注:MRI:磁共振成像;CM-MB:肌酸激酶同工酶;TnI:肌钙蛋白I;CRP:C反应蛋白。 -
[1] Davis MB, Arany Z, McNamara DM, et al. Peripartum Cardiomyopathy: JACC State-of-the-Art Review[J]. J Am Coll Cardiol, 2020, 75(2): 207-221. doi: 10.1016/j.jacc.2019.11.014
[2] 唐婷婷, 廖玉华. 2023 ESC急性和慢性心力衰竭诊断和治疗指南更新要点解读[J]. 临床心血管病杂志, 2023, 39(10): 749-752. doi: 10.13201/j.issn.1001-1439.2023.10.003
[3] McNamara DM, Elkayam U, Alharethi R, et al. Clinical Outcomes for Peripartum Cardiomyopathy in North America: Results of the IPAC Study(Investigations of Pregnancy-Associated Cardiomyopathy)[J]. J Am Coll Cardiol, 2015, 66(8): 905-914. doi: 10.1016/j.jacc.2015.06.1309
[4] Irizarry OC, Levine LD, Lewey J, et al. Comparison of Clinical Characteristics and Outcomes of Peripartum Cardiomyopathy Between African American and Non-African American Women[J]. JAMA Cardiol, 2017, 2(11): 1256-1260. doi: 10.1001/jamacardio.2017.3574
[5] Ntusi NBA, Badri M, Gumedze F, et al. Pregnancy-Associated Heart Failure: A Comparison of Clinical Presentation and Outcome between Hypertensive Heart Failure of Pregnancy and Idiopathic Peripartum Cardiomyopathy[J]. PloS One, 2015, 10(8): e0133466.
[6] Sliwa K, Hilfiker-Kleiner D, Petrie MC, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy[J]. Eur J Heart Fail, 2010, 12(8): 767-778. doi: 10.1093/eurjhf/hfq120
[7] Sliwa K, Mebazaa A, Hilfiker-Kleiner D, et al. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy(PPCM): EURObservational Research Programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM[J]. Eur J Heart Fail, 2017, 19(9): 1131-1141. doi: 10.1002/ejhf.780
[8] Bauersachs J, Arrigo M, Hilfiker-Kleiner D, et al. Current management of patients with severe acute peripartum cardiomyopathy: practical guidance from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy[J]. Eur J Heart Fail, 2016, 18(9): 1096-1105. doi: 10.1002/ejhf.586
[9] Honigberg MC, Givertz MM. Peripartum cardiomyopathy[J]. BMJ, 2019, 364: k5287.
[10] 廖玉华, 廖梦阳, 袁璟. 心力衰竭防治的新机制与新途径[J]. 临床心血管病杂志, 2024, 40(1): 1-4. doi: 10.13201/j.issn.1001-1439.2024.01.001
[11] Hoevelmann J, Viljoen CA, Manning K, et al. The prognostic significance of the 12-lead ECG in peripartum cardiomyopathy[J]. Int J Cardiol, 2019, 276: 177-184. doi: 10.1016/j.ijcard.2018.11.008
[12] Li W, Li H, Long Y. Clinical Characteristics and Long-term Predictors of Persistent Left Ventricular Systolic Dysfunction in Peripartum Cardiomyopathy[J]. Can J Cardiol, 2016, 32(3): 362-368. doi: 10.1016/j.cjca.2015.07.733
[13] Patten IS, Rana S, Shahul S, et al. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy[J]. Nature, 2012, 485(7398): 333-338. doi: 10.1038/nature11040
[14] Bauersachs J. Poor Outcomes in Poor Patients?Peripartum Cardiomyopathy-Not Just Black and White[J]. JAMA Cardiol, 2017, 2(11): 1261-1262. doi: 10.1001/jamacardio.2017.3605
[15] Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy[J]. Kardiol Pol, 2019, 77(3): 245-326. doi: 10.5603/KP.2019.0049
[16] Selle T, Renger I, Labidi S, et al. Reviewing peripartum cardiomyopathy: current state of knowledge[J]. Future Cardiol, 2009, 5(2): 175-189. doi: 10.2217/14796678.5.2.175
[17] Hilfiker-Kleiner D, Sliwa K. Pathophysiology and epidemiology of peripartum cardiomyopathy[J]. Nat Rev Cardiol, 2014, 11(6): 364-370. doi: 10.1038/nrcardio.2014.37
[18] van Spaendonck-Zwarts KY, Posafalvi A, van den Berg MP, et al. Titin gene mutations are common in families with both peripartum cardiomyopathy and dilated cardiomyopathy[J]. Eur Heart J, 2014, 35(32): 2165-2173. doi: 10.1093/eurheartj/ehu050
[19] Gunderson EP, Croen LA, Chiang V, et al. Epidemiology of peripartum cardiomyopathy: incidence, predictors, and outcomes[J]. Obstet Gynecol, 2011, 118(3): 583-591. doi: 10.1097/AOG.0b013e318229e6de
[20] Elkayam U, Goland S, Pieper PG, et al. High-Risk Cardiac Disease in Pregnancy: Part II[J]. J Am Coll Cardiol, 2016, 68(5): 502-516. doi: 10.1016/j.jacc.2016.05.050
[21] Dhesi S, Savu A, Ezekowitz JA, et al. Association Between Diabetes During Pregnancy and Peripartum Cardiomyopathy: A Population-Level Analysis of 309, 825 Women[J]. Can J Cardiol, 2017, 33(7): 911-917. doi: 10.1016/j.cjca.2017.02.008
[22] Spracklen TF, Chakafana G, Schwartz PJ, et al. Genetics of Peripartum Cardiomyopathy: Current Knowledge, Future Directions and Clinical Implications[J]. Genes(Basel), 2021, 12(1): 103.
[23] Tamrat R, Kang Y, Scherrer-Crosbie M, et al. Women with peripartum cardiomyopathy have normal ejection fraction, but abnormal systolic strain, during pregnancy[J]. ESC Heart Fail, 2021, 8(4): 3382-3386. doi: 10.1002/ehf2.13323
[24] Horne BD, Rasmusson KD, Alharethi R, et al. Genome-wide significance and replication of the chromosome 12p11.22 locus near the PTHLH gene for peripartum cardiomyopathy[J]. Circ Cardiovasc Genet, 2011, 4(4): 359-366. doi: 10.1161/CIRCGENETICS.110.959205
[25] Bello NA, Arany Z. Molecular mechanisms of peripartum cardiomyopathy: A vascular/hormonal hypothesis[J]. Trends Cardiovasc Med, 2015, 25(6): 499-504. doi: 10.1016/j.tcm.2015.01.004
[26] Chung E, Yeung F, Leinwand LA. Calcineurin activity is required for cardiac remodelling in pregnancy[J]. Cardiovasc Res, 2013, 100(3): 402-410. doi: 10.1093/cvr/cvt208
[27] Koczo A, Marino A, Rocco J, et al. Proinflammatory TH17 cytokine activation, disease severity and outcomes in peripartum cardiomyopathy[J]. Int J Cardiol, 2021, 339: 93-98. doi: 10.1016/j.ijcard.2021.06.022
[28] Sarojini A, Sai Ravi Shanker A, Anitha M. Inflammatory Markers-Serum Level of C-Reactive Protein, Tumor Necrotic Factor-α, and Interleukin-6 as Predictors of Outcome for Peripartum Cardiomyopathy[J]. J Obstet Gynaecol India, 2013, 63(4): 234-239. doi: 10.1007/s13224-013-0428-9
[29] Sliwa K, Förster O, Libhaber E, et al. Peripartum cardiomyopathy: inflammatory markers as predictors of outcome in 100 prospectively studied patients[J]. Eur Heart J, 2006, 27(4): 441-446. doi: 10.1093/eurheartj/ehi481
[30] Melchiorre K, Sharma R, Khalil A, et al. Maternal Cardiovascular Function in Normal Pregnancy: Evidence of Maladaptation to Chronic Volume Overload[J]. Hypertension, 2016, 67(4): 754-762. doi: 10.1161/HYPERTENSIONAHA.115.06667
[31] De Haas S, Ghossein-Doha C, Geerts L, et al. Cardiac remodeling in normotensive pregnancy and in pregnancy complicated by hypertension: systematic review and meta-analysis[J]. Ultrasound Obstet Gynecol, 2017, 50(6): 683-696. doi: 10.1002/uog.17410
[32] Hilfiker-Kleiner D, Haghikia A, Nonhoff J, et al. Peripartum cardiomyopathy: current management and future perspectives[J]. Eur Heart J, 2015, 36(18): 1090-1097. doi: 10.1093/eurheartj/ehv009
[33] European Society of Gynecology(ESG), Association for European Paediatric Cardiology(AEPC), German Society for Gender Medicine(DGesGM), et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2011, 32(24): 3147-3197. doi: 10.1093/eurheartj/ehr218
[34] Arany Z, Elkayam U. Peripartum Cardiomyopathy[J]. Circulation, 2016, 133(14): 1397-1409. doi: 10.1161/CIRCULATIONAHA.115.020491
[35] Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy[J]. Eur Heart J, 2018, 39(34): 3165-3241. doi: 10.1093/eurheartj/ehy340
[36] Loyaga-Rendon RY, Pamboukian SV, Tallaj JA, et al. Outcomes of patients with peripartum cardiomyopathy who received mechanical circulatory support. Data from the Interagency Registry for Mechanically Assisted Circulatory Support[J]. Circ Heart Fail, 2014, 7(2): 300-309. doi: 10.1161/CIRCHEARTFAILURE.113.000721
[37] Dutt S, Wong F, Spurway JH. Fatal myocardial infarction associated with bromocriptine for postpartum lactation suppression[J]. Aust N Z J Obstet Gynaecol, 1998, 38(1): 116-117. doi: 10.1111/j.1479-828X.1998.tb02977.x
[38] Hilfiker-Kleiner D, Haghikia A, Berliner D, et al. Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study[J]. Eur Heart J, 2017, 38(35): 2671-2679. doi: 10.1093/eurheartj/ehx355
[39] Koczo A, Marino A, Jeyabalan A, et al. Breastfeeding, Cellular Immune Activation, and Myocardial Recovery in Peripartum Cardiomyopathy[J]. JACC Basic Transl Sci, 2019, 4(3): 291-300. doi: 10.1016/j.jacbts.2019.01.010
[40] Iffy L, Lindenthal J, Mcardle JJ, et al. Severe cerebral accidents postpartum in patients taking bromocriptine for milk suppression[J]. Isr J Med Sci, 1996, 32(5): 309-312.
[41] Eltonsy S, Martin B, Ferreira E, et al. Systematic procedure for the classification of proven and potential teratogens for use in research[J]. Birth Defects Res A Clin Mol Teratol, 2016, 106(4): 285-297. doi: 10.1002/bdra.23491
[42] Bozkurt B, Colvin M, Cook J, et al. Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement From the American Heart Association[J]. Circulation, 2016, 134(23): e579-e646.
[43] Duncker D, Westenfeld R, Konrad T, et al. Risk for life-threatening arrhythmia in newly diagnosed peripartum cardiomyopathy with low ejection fraction: a German multi-centre analysis[J]. Clin Res Cardiol, 2017, 106(8): 582-589. doi: 10.1007/s00392-017-1090-5
[44] Rasmusson K, Brunisholz K, Budge D, et al. Peripartum cardiomyopathy: post-transplant outcomes from the United Network for Organ Sharing Database[J]. J Heart Lung Transplant, 2012, 31(2): 180-186. doi: 10.1016/j.healun.2011.11.018
[45] Peters A, Caroline M, Zhao HQ, et al. Initial Right Ventricular Dysfunction Severity Identifies Severe Peripartum Cardiomyopathy Phenotype With Worse Early and Overall Outcomes: A 24-Year Cohort Study[J]. J Am Heart Assoc, 2018, 7(9): e008378. . doi: 10.1161/JAHA.117.008378
[46] Sliwa K, Petrie MC, Hilfiker-Kleiner D, et al. Long-term prognosis, subsequent pregnancy, contraception and overall management of peripartum cardiomyopathy: practical guidance paper from the Heart Failure Association of the European Society of Cardiology Study Group on Peripartum Cardiomyopathy[J]. Eur J Heart Fail, 2018, 20(6): 951-962. doi: 10.1002/ejhf.1178
[47] Stuart JJ, Bairey Merz CN, Berga SL, et al. Maternal recall of hypertensive disorders in pregnancy: a systematic review[J]. J Womens Health(Larchmt), 2013, 22(1): 37-47. doi: 10.1089/jwh.2012.3740
[48] Haghikia A, Röntgen P, Vogel-Claussen J, et al. Prognostic implication of right ventricular involvement in peripartum cardiomyopathy: a cardiovascular magnetic resonance study[J]. ESC Heart Fail, 2015, 2(4): 139-149. doi: 10.1002/ehf2.12059
[49] Kodogo V, Azibani F, Sliwa K. Role of pregnancy hormones and hormonal interaction on the maternal cardiovascular system: a literature review[J]. Clin Res Cardiol, 2019, 108(8): 831-846. doi: 10.1007/s00392-019-01441-x
[50] Rajakumar A, Cerdeira AS, Rana S, et al. Transcriptionally active syncytial aggregates in the maternal circulation may contribute to circulating soluble fms-like tyrosine kinase 1 in preeclampsia[J]. Hypertension, 2012, 59(2): 256-264. doi: 10.1161/HYPERTENSIONAHA.111.182170
[51] Levine RJ, Maynard SE, Qian C, et al. Circulating angiogenic factors and the risk of preeclampsia[J]. New Engl J Med, 2004, 350(7): 672-683. doi: 10.1056/NEJMoa031884
[52] Halkein J, Tabruyn SP, Ricke-Hoch M, et al. MicroRNA-146a is a therapeutic target and biomarker for peripartum cardiomyopathy[J]. J Clin Invest, 2013, 123(5): 2143-2154. doi: 10.1172/JCI64365
[53] Odiete O, Hill MF, Sawyer DB. Neuregulin in cardiovascular development and disease[J]. Circ Res, 2012, 111(10): 1376-1385. doi: 10.1161/CIRCRESAHA.112.267286
[54] Feyen E, Ricke-Hoch M, Van Fraeyenhove J, et al. ERBB4 and Multiple MicroRNAs That Target ERBB4 Participate in Pregnancy-Related Cardiomyopathy[J]. Circ Heart Fail, 2021, 14(7): e006898.
[55] Venkatesha S, Topprsian M, Lam C, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia[J]. Nat Med, 2006, 12(6): 642-649. doi: 10.1038/nm1429
[56] Rowe GC, Jiang A, Arany Z. PGC-1 coactivators in cardiac development and disease[J]. Circ Res, 2010, 107(7): 825-838. doi: 10.1161/CIRCRESAHA.110.223818
[57] Handschin C, Spiegelman BM. Peroxisome proliferator-activated receptor gamma coactivator 1 coactivators, energy homeostasis, and metabolism[J]. Endocr Rev, 2006, 27(7): 728-735. doi: 10.1210/er.2006-0037
[58] Hilfiker-Kleiner D, Kaminski K, Podewski E, et al. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy[J]. Cell, 2007, 128(3): 589-600. doi: 10.1016/j.cell.2006.12.036
[59] Arany Z, Foo SY, Ma Y, et al. HIF-independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC-1alpha[J]. Nature, 2008, 451(7181): 1008-1012. doi: 10.1038/nature06613
[60] Chinsomnoon J, Ruas J, Gupta RK, et al. The transcriptional coactivator PGC-1alpha mediates exercise-induced angiogenesis in skeletal muscle[J]. Proc Natl Acad Sci U S A, 2009, 106(50): 21401-21406. doi: 10.1073/pnas.0909131106
[61] Hoes MF, Tromp J, Ouwerkerk W, et al. The role of cathepsin D in the pathophysiology of heart failure and its potentially beneficial properties: a translational approach[J]. Eur J Heart Fail, 2020, 22(11): 2102-2111. doi: 10.1002/ejhf.1674
[62] Chiarello DI, Abad C, Rojas D, et al. Oxidative stress: Normal pregnancy versus preeclampsia[J]. Biochim Biophys Acta Mol Basis Dis, 2020, 1866(2): 165354. doi: 10.1016/j.bbadis.2018.12.005
[63] Redondo-Angulo I, Mas-Stachurska A, Sitges M, et al. Fgf21 is required for cardiac remodeling in pregnancy[J]. Cardiovasc Res, 2017, 113(13): 1574-1584. doi: 10.1093/cvr/cvx088
[64] Lehman JJ, Barger PM, Kovacs A, et al. Peroxisome proliferator-activated receptor gamma coactivator-1 promotes cardiac mitochondrial biogenesis[J]. J Clin Invest, 2000, 106(7): 847-856. doi: 10.1172/JCI10268
[65] Stapel B, Kohlhaas M, Ricke-Hoch M, et al. Low STAT3 expression sensitizes to toxic effects of β-adrenergic receptor stimulation in peripartum cardiomyopathy[J]. Eur Heart J, 2017, 38(5): 349-361.
[66] Ricke-Hoch M, Bultmann I, Stapel B, et al. Opposing roles of Akt and STAT3 in the protection of the maternal heart from peripartum stress[J]. Cardiovasc Res, 2014, 101(4): 587-596. doi: 10.1093/cvr/cvu010
[67] Kouzu H, Tatekoshi Y, Chang HC, et al. ZFP36L2 suppresses mTORc1 through a P53-dependent pathway to prevent peripartum cardiomyopathy in mice[J]. J Clin Invest, 2022, 132(10): e154491. doi: 10.1172/JCI154491
-

计量
- 文章访问数: 347
- 施引文献: 0



 下载:
下载: