Risk factors for delayed extubation after off-pump coronary artery bypass grafting and the prediction nomogram model
-
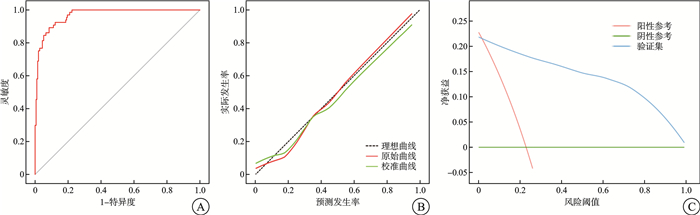
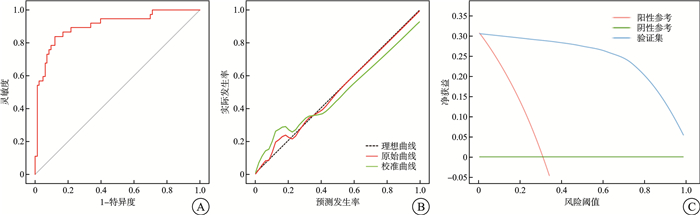
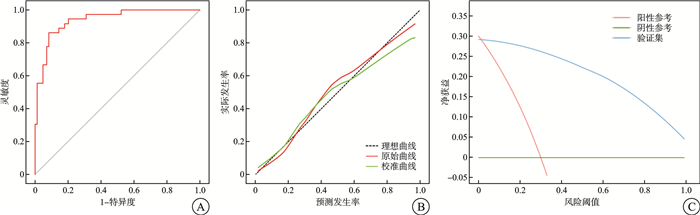
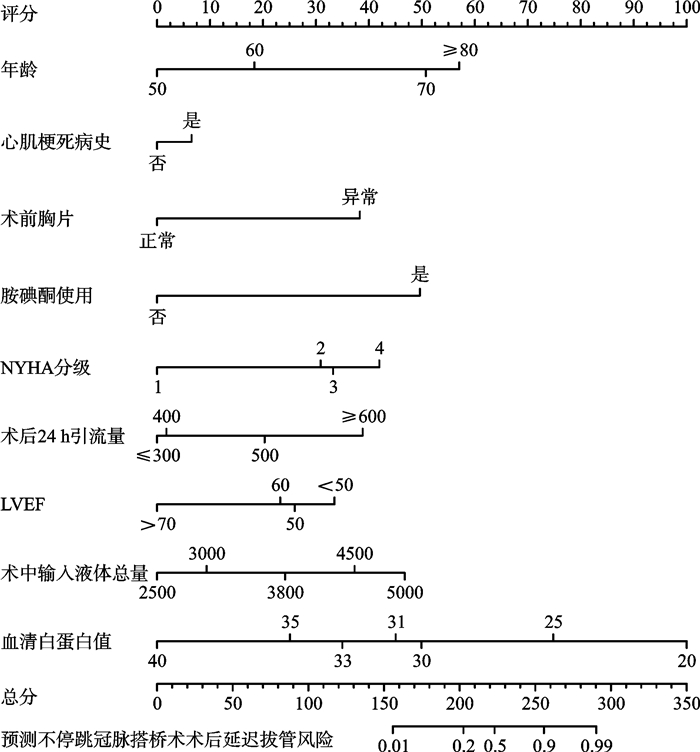
摘要: 目的 探讨不停跳冠状动脉旁路移植(OPCABG)术后延迟拔管的影响因素,构建其风险预测列线图模型,并进行内外部验证。方法 采用方便抽样法,选取2022年8月—2023年12月于首都医科大学附属北京朝阳医院心脏大血管外科行OPCABG的400例患者为研究对象,按照7∶3的比例将其随机分为建模集(280例)和内部验证集(120例)。另选取2024年1—9月该医院分院区行OPCABG的100例患者作为外部验证集。收集所有患者的临床资料信息,运用logistic回归模型分析术后延迟拔管的危险因素。基于多因素logistic回归分析结果,构建OPCABG术后延迟拔管风险预测列线图模型。采用Hosmer-Lemeshow检验、校准曲线评估该列线图模型的拟合程度,采用ROC曲线评估该列线图的预测效能。结果 Logistic回归分析结果显示,年龄、吸烟史、脑血管病史、慢性肾病史、心肌梗死病史、术前胸X线片异常、使用胺碘酮、NYHA分级、术后48 h胸X线片异常、术后24 h引流量、左心室射血分数(LVEF)、术中输入液体总量、血清白蛋白值是OPCABG术后延迟拔管的影响因素(均P<0.05)。基于上述因素构建OPCABG术后延迟拔管风险预测列线图模型。Hosmer-Lemeshow拟合优度检验结果显示,在建模集、内部验证集和外部验证集中,该列线图模型拟合较好(χ2=1.76,P=0.93;χ2=3.65,P=0.88;χ2=2.69,P=0.95)。ROC曲线分析结果显示,该列线图模型预测建模集、内部验证集和外部验证集OPCABG术后延迟拔管的AUC分别为0.96(95%CI 0.89~0.98)、0.89(95%CI 0.82~0.94)和0.93(95%CI 0.88~0.97)。结论 年龄50~60岁、NYHA分级Ⅲ级、心肌梗死病史、术前胸X线片异常、使用胺碘酮、术后24 h引流量≤300 mL、LVEF、术中输入液体总量、血清白蛋白值是OPCABG术后延迟拔管的危险因素。依据上述影响因素构建的用于评估OPCABG术后延迟拔管风险的预测列线图模型拟合情况较好。
-
关键词:
- 不停跳冠状动脉旁路移植 /
- 延迟拔管 /
- 危险因素 /
- 列线图 /
- 预测模型
Abstract: Objective To explore the influencing factors of delayed extubation after off-pump coronary artery bypass grafting(OPCABG) and to establish a risk prediction nomogram model with internal and external validation.Methods A total of 400 patients who underwent OPCABG in the Department of Cardiac Macrovascular Surgery, Beijing Chaoyang Hospital, Capital Medical University from August 2022 to December 2023 were selected as the study objects by convenient sampling method. They were randomly divided into the modeling set(n=280) and the internal validation set(n=120) according to a ratio of 7∶3. A total of 100 patients who underwent OPCABG from January to September 2024 in this hospital branch were selected as the external validation set. The clinical data of all patients were collected, and the risk factors of delayed extubation were analyzed by logistic regression models. Based on the results of logistic regression analysis, the risk prediction model of delayed extubation after OPCABG was constructed. Hosmer-Lemeshow test and calibration curves were used to evaluate the fitting degree of the nomogram model, and the ROC curve was used to evaluate the prediction efficiency of the nomogram model.Results Logistic regression analysis showed that age, smoking history, cerebrovascular history, chronic kidney disease history, myocardial infarction history, preoperative chest X-ray abnormalities, amiodarone use, NYHA grade, 48 h postoperative chest X-ray abnormalities, 24 h postoperative drainage volume, left ventricular ejection fraction(LVEF), total intraoperative fluid input, and serum albumin value were influencing factors of delayed extubation after OPCABG operation(all P<0.05). A nomogram model predicting the risk of delayed extubation after OPCABG was developed using the identified risk factors. The Hosmer-Lemeshow test indicated good model fit in the modeling set(χ2=1.76, P=0.93), internal validation set(χ2=3.65, P=0.88), and external validation set(χ2=2.69, P=0.95). The AUC values for predicting delayed extubation were 0.96(95%CI 0.89-0.98), 0.89(95%CI 0.82-0.94) and 0.93(95%CI 0.88-0.97) in the modeling, internal validation, and external validation sets, respectively.Conclusion Age 50-60 years old, NYHA grade Ⅲ, myocardial infarction history, preoperative chest X-ray abnormalities, amiodarone use, postoperative 24-hour drainage≤300 mL, LVEF, total intraoperative fluid input, and serum albumin are risk factors for delayed extubation after OPCABG. The nomogram model incorporating these factors showed good fit and predictive performance. -

-
表 1 临床资料比较
Table 1. Comparison of clinical data
例(%), X±S 项目 非延迟拔管组(299例) 延迟拔管组(101例) t/χ2 P 性别 0.601 0.438 男 222(74.2) 71(70.3) 女 77(25.8) 30(29.7) 年龄 -10.407 < 0.001 50~60岁 171(57) 13(13) 61~70岁 71(24) 73(72) 70~80岁 43(14) 5(5) >80岁 14(5) 10(10) 吸烟史 193(64.5) 47(46.5) 10.208 0.001 高血压病史 206(68.6) 59(58.4) 3.463 0.063 糖尿病病史 137(45.5) 39(38.6) 1.448 0.229 脑血管病史 34(11) 27(26.7) 14.588 < 0.001 慢性肾病史 5(1.7) 13(12.9) 22.033 < 0.001 心肌梗死病史 73(24.4) 36(35.6) 4.802 0.028 PCI病史 55(18.4) 22(21.8) 0.557 0.455 室壁瘤 79(26.4) 31(30.7) 0.691 0.406 术前胸X线片异常 23(7.7) 36(35.6) 46.908 < 0.001 胺碘酮使用 70(23.4) 35(34.7) 4.929 0.026 NYHA分级 -6.726 < 0.010 Ⅰ级 147(49) 7(7) Ⅱ级 115(38) 75(74) Ⅲ级 31(10) 11(11) Ⅳ级 6(2) 8(8) BMI -0.011 0.991 正常(≥18.5且<25) 98(33) 34(34) 超重(≥25且<30) 69(23) 24(24) 肥胖Ⅰ级(≥30且<35) 69(23) 19(19) 肥胖Ⅱ级(≥35且<40) 36(12) 13(13) 肥胖Ⅲ级(≥40) 28(9) 11(11) 术后48 h内胸X线片 -9.448 < 0.010 双肺纹理增重 241(81) 31(31) 渗出性改变 50(17) 52(51) 气胸 0(0) 4(4) 胸腔积液 8(3) 14(14) 住院天数 -0.442 0.658 <10 d 11(3) 7(7) 11~20 d 212(71) 69(69) 21~30 d 51(17) 14(14) >30 d 25(9) 11(10) 术中出血量 -0.127 0.899 <200 mL 110(37) 35(35) 201~400 mL 80(27) 29(29) 401~600 mL 59(20) 22(22) 601~800 mL 41(13) 12(11) >800 mL 9(3) 3(3) 术中红细胞输注量 -1.808 0.071 0~200 mL 207(69) 59(58) 201~400 mL 67(22) 34(33) 400~600 mL 6(2) 1(1) 601~800 mL 14(5) 3(3) >800 mL 5(2) 4(5) 术后24 h引流量 -5.161 < 0.01 ≤300 mL 49(16) 8(8) 301~400 mL 119(40) 22(22) 401~500 mL 53(18) 21(21) 501~600 mL 57(19) 25(25) ≥600 mL 21(7) 25(25) LVEF/% 56.39±8.811 53.79±8.776 5.074 < 0.001 LVEDD/mm 48.88±4.957 52.86±5.945 -0.578 0.564 手术时长/h 4.04±0.286 4.37±0.594 -1.151 0.252 术中输入液体总量/mL 3 858.93±665.818 3 836.54±575.221 -3.901 < 0.001 血清白蛋白/(g/L) 31.63±5.384 30.75±4.996 13.279 < 0.001 表 2 自变量赋值方式
Table 2. Assignment of predictor
自变量 赋值方式 慢性肾病史 是=1,否=0 吸烟史 是=1,否=0 脑血管病史 是=1,否=0 心肌梗死病史 是=1,否=0 术前胸X线片 异常=1,正常=0 胺碘酮使用 是=1,否=0 LVEF 原值录入 术中输入液体总量 原值录入 血清白蛋白值 原值录入 年龄 50~60岁=1,61~70岁=2,70~80岁=3,>80岁=4 NYHA分级 Ⅰ级=1,Ⅱ级=2,Ⅲ级=3,Ⅳ级=4 术后48 h内胸X线片 双肺纹理增重=1,渗出性改变=2,气胸=3,胸腔积液=4 术后24 h引流量 ≤300 mL=1,301~400 mL=2,401~500 mL=3,501~600 mL=4 表 3 OPCABG术后延迟拔管的logistic多因素分析
Table 3. Multivariate logistic analysis of delayed extubation after OPCABG
因素 OR 95%CI P 心肌梗死病史 3.794 1.084~13.280 0.037 术前胸X线片异常 15.121 3.600~63.505 < 0.001 胺碘酮使用 8.147 2.302~28.827 0.001 年龄50~60岁 3.023 3.001~3.380 0.008 NYHA分级Ⅲ级 2.014 1.001~5.195 0.002 术后24 h引流量≤ 300 mL 2.065 1.010~2.442 0.005 LVEF 1.267 1.125~1.427 < 0.001 术中输入液体总量 1.001 1.000~1.002 0.008 血清白蛋白值 1.547 1.442~14.677 < 0.001 -
[1] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2021概要[J]. 中国循环杂志, 2022, 37(6): 553-578. doi: 10.3969/j.issn.1000-3614.2022.06.001
[2] 国家卫生健康委员会. 中国卫生健康统计年鉴2021[M]. 北京: 中国协和医科大学出版社, 2021.
[3] 苏国宝, 席茜, 刘晓晨, 等. 不停跳和体外循环下冠状动脉搭桥术后患者心肺功能、血液动力学和炎症变化[J]. 中华实验外科杂志, 2022, 39(5): 844-846. doi: 10.3760/cma.j.cn421213-20210915-01274
[4] 欧阳春. 不停跳与停跳体外循环冠状动脉搭桥术心肌保护的临床研究[D]. 广东: 汕头大学, 2020.
[5] Kumalasari RI, Kosasih CE, Priambodo AP. A Scoping Review of Factors Associated with Delayed Extubation in Post Cardiac Surgery Patients[J]. Vasc Health Risk Manag, 2025, 21: 1-15. doi: 10.2147/VHRM.S479352
[6] 耿晨, 张苗, 张丽丽, 等. 多学科联合五阶梯渐进式活动方案在ICU机械通气病人中的应用[J]. 护理研究, 2025, 39(2): 285-290.
[7] Li C, Zhang P, Zhang ZC, et al. Effect of breathing exercises to prevent pulmonary complications in patients undergoing coronary artery bypass graft surgery: a prospective randomized controlled trials study protocol[J]. Front Med(Lausanne), 2024, 11: 1424291.
[8] 冯硕. 非体外循环冠状动脉旁路移植术患者术后延迟拔除气管导管的危险因素分析[D]. 河北: 河北医科大学, 2017.
[9] Huang X, Luo Z, Liang W, et al. Survival nomogram for young breast cancer patients based on the SEER database and an external validation cohort[J]. Ann Surg Oncol, 2022, 29(9): 5772-5781. doi: 10.1245/s10434-022-11911-8
[10] 兰怡昕, 邱小芩, 黄兰青, 等. 老年慢性心力衰竭患者发生低蛋白血症的影响因素分析及其风险预测列线图模型构建及验证[J]. 实用心脑肺血管病杂志, 2024, 32(5): 42-48.
[11] 李鹏, 朱静文, 许开伟, 等. 基于随机森林算法建立非急诊大手术后延迟拔管的预测模型[J]. 临床麻醉学杂志, 2024, 40(1): 7-12.
[12] 王馨培, 傅强, 王子玉. 不同心脏手术风险评价系统预测单中心OPCABG患者术后延长机械通气的效能分析[J]. 山东医药, 2020, 60(23): 54-56. doi: 10.3969/j.issn.1002-266X.2020.23.014
[13] 韩琳, 王东信. 术后肺部并发症及其对临床结局的影响研究进展[J]. 中国医药导报, 2024, 21(27): 45-49.
[14] 张倩倩, 于欢, 范永娟, 等. 冠状动脉旁路移植术延迟气管导管拔管的影响因素分析[J]. 国际麻醉学与复苏杂志, 2024, 45(4): 354-360. doi: 10.3760/cma.j.cn321761-20231128-01009
[15] 郭强. 急性Stanford A型主动脉夹层术后延迟拔管的危险因素分析[D]. 江西: 南昌大学, 2023.
[16] 陈秀梅, 张俐鹏, 黄鑫, 等. 低射血分数非体外循环冠状动脉旁路移植术患者围手术期积极康复治疗的效果[J]. 中国医药, 2023, 18(5): 676-680.
[17] 周元, 杨秀滨. 非体外循环冠状动脉旁路移植术后机械通气时间延长的危险因素及预后分析[J/CD]. 中华危重症医学杂志(电子版), 2020, 13(3): 181-187.
[18] 张叶霞, 杨斯钰, 张丽萍, 等. 冠状动脉搭桥手术患者机械通气延长风险预测模型的系统评价[J]. 当代护士(中旬刊), 2024, 31(9): 44-49.
[19] 李芮柯, 魏珂. 术后无创呼吸支持的研究进展[J]. 临床麻醉学杂志, 2024, 40(6): 639-643.
[20] Trudzinski FC, Neetz B, Bornitz F, et al. Risk Factors for Prolonged Mechanical Ventilation and Weaning Failure: A Systematic Review[J]. Respiration, 2022, 101(10): 959-969. doi: 10.1159/000525604
[21] Ghauri SK, Javaeed A, Mustafa KJ, et al. Predictors of prolonged mechanical ventilation in patients admitted to intensive care units: A systematic review[J]. Int J Health Sci(Qassim), 2019, 13(6): 31-38.
[22] 高曼, 张飞飞, 郝清卿, 等. 左室射血分数恢复对STEMI伴射血分数中间值患者的长期预后及影响因素分析[J]. 临床心血管病杂志, 2021, 37(9): 824-829. doi: 10.13201/j.issn.1001-1439.2021.09.009
[23] 阿布都赛米·艾尼. 全腔镜体外循环下心脏手术后机械通气时间延长(PMV)的危险因素分析[D]. 新疆: 新疆医科大学, 2023.
[24] 王俊华. 体外循环、非体外循环下冠脉搭桥术对患者心肺功能的影响分析[J]. 黑龙江医学, 2020, 44(7): 891-893. doi: 10.3969/j.issn.1004-5775.2020.07.009
[25] 张辰宇, 穆心苇. 人血白蛋白在心脏加速康复外科中的作用[J]. 中国体外循环志, 2023, 21(3): 179-182, 188.
[26] 聂有和, 魏美霞, 吴全忠. 早期肠内营养支持在危重症病人中的应用[J]. 智慧健康, 2020, 6(24): 74-75.
[27] Shahidi Delshad E, Sanadgol H. Fluid Balance Has Effects on the Length of Hospital Stay After Coronary Artery Bypass Grafting Surgery[J]. Iran J Kidney Dis, 2020, 14(1): 36-43.
[28] Shahsanaei F, Behrooj S, Petrudi NR, et al. The Overall Prevalence and Main Determinants of Prolonged Mechanical Ventilation in Patients Undergoing Coronary Artery Bypass Grafting: A Systematic Review[J]. Heart Views, 2023, 24(4): 188-193. doi: 10.4103/heartviews.heartviews_71_23
[29] 朱明珠, 薛庆生, 于布为. 非体外循环冠状动脉旁路移植术的循环管理与术后心肌损伤[J]. 上海医学, 2023, 46(3): 192-196.
[30] Li X, Zhang H, Luo Y, et al. Amiodarone use and prolonged mechanical ventilation after cardiac surgery: a single-center analysis[J]. BMC Cardiovasc Disord, 2025, 25(1): 129. doi: 10.1186/s12872-025-04576-0
[31] Zhang QQ, Xu J, Huang QH, et al. Risk factors for delayed extubation after pediatric perineal anaplasty in patients less than 1 year of age: a retrospective study[J]. BMC Pediatr, 2024, 24(1): 307. doi: 10.1186/s12887-024-04781-4
[32] 张永苹, 雷黎明, 凌云, 等. 156例体外循环心脏术后严重高乳酸血症患者的护理[J]. 护理学报, 2023, 30(4): 66-68.
[33] 周羽靖, 梁法禹, 曲扬. 心脏瓣膜置换术后病人异常出血的判断与处理[J]. 护理研究, 2020, 34(10): 1863-1866. doi: 10.12102/j.issn.1009-6493.2020.10.043
-

计量
- 文章访问数: 37
- 施引文献: 0



 下载:
下载: