Utilization of multimodal imaging for the evaluation of left ventricular remodeling and risk stratification in severe aortic regurgitation
-
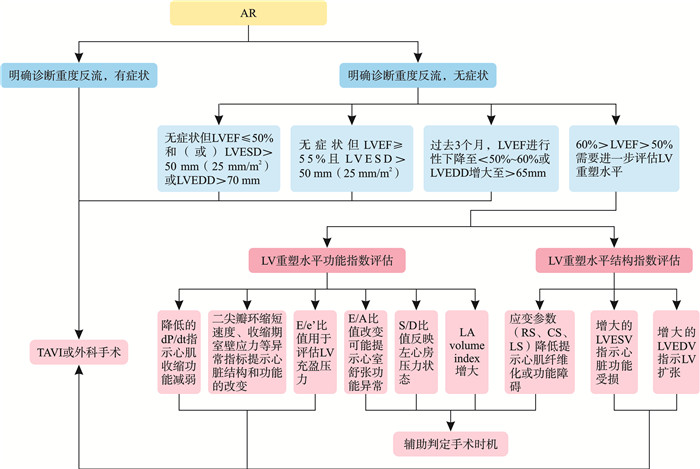
摘要: 主动脉瓣反流(aortic regurgitation,AR)严重程度和左心室(left ventricular,LV)重塑水平密切相关,确定AR干预时机对患者长期预后至关重要,心脏超声、心脏磁共振、CT及生物标记物等多模态影像均可用于评估AR的严重程度,但对LV重塑水平评估存在一定不足。本文指出多模态影像评估从功能参数、结构参数等角度来评价AR患者LV重塑水平,并总结其对AR临床决策制定的指导意义,为临床运用提供参考。Abstract: The severity of aortic regurgitation(AR) is closely associated with the extent of left ventricular(LV) remodeling. The timing of AR intervention plays a pivotal role in determining the long-term prognosis for patients. Various multimodal techniques, including cardiac ultrasound, cardiac magnetic resonance imaging, computed tomography, and biomarkers, can evaluate the severity of AR disease. However, there are certain limitations in assessing LV remodeling. This article emphasizes that multimodal imaging assessment enables the evaluation of LV remodeling level in AR patients from both functional and structural perspectives and summarizes its significant implications for clinical decision-making regarding AR management, thereby providing valuable insights for practical application.
-

-
表 1 重度AR的LV不同重塑水平参数
Table 1. Parameters of different levels of LV remodeling in severe AR
项目 正常参考值 LV高水平重塑 LV中等水平重塑 LV低水平重塑 功能参数 LVEF[6] ≥55%~70% < 50% 50~55% >55% dP/dt/(mmHg/s)[26] >1 200 < 1 000 1 000~1 200 E峰/A峰比值[27] 0.8~2 ≥2 E峰/e′比值[27] < 8 >14 8~14 S峰/D峰比值[28] 1~2 >2 1-2 < 1 结构参数 LA volume index/(mL/m2)[22] 正常值因性别、体表面积而异 >49(>34) 41~49 ≤40 LVEDV/mL[18] 男性:181.2±73.6
女性:133.6±38.9< 246 246~470 >470 全局纵向应变[8] 男性:(-19.0±3.4)%
女性:(-12.2±2.6)%>-19% -22%~-19% ≤-22% LVEF:左室射血分数;dP/dt:左室压力上升最大速率;E峰/A峰比值:二尖瓣舒张早期血流速度(E峰)和舒张晚期血流速度(A峰)的比值;E峰/e′比值:二尖瓣舒张早期血流速度(E峰)和二尖瓣环组织多普勒早期舒张速度(e′)的比值;S峰/D峰比值:肺静脉血流的收缩期(S峰)和舒张期(D峰)速度比值;LA volume index:左心房容积指数;LVESV:左心室收缩末期容积;LVEDV:左心室舒张末期容积。 表 2 重度AR风险分类及分层
Table 2. Classification and stratification of severe AR
危险分层 分类标准 关键指标 处理建议 高风险 有症状的重度反流 存在临床症状(呼吸困难、胸痛等)
多模态成像确认重度反流TAVI或外科手术 中风险 无症状但存在以下任一情况:
①LVEF≤50%
②60%>LVEF>50%需评估LV重塑水平
③左心室扩张LVEF≤50%或动态下降至50%~60%
LVESD>50 mm(或>25 mm/m2)
LVEDD>70 mm(或进行性增长>65 mm)定期监测
结合LV重塑评估决定是否手术低风险 无症状且左心室功能/结构正常 LVEF>60%
LVESD≤50 mm(或≤25 mm/m2)
LVEDD≤65 mm保守治疗(每6~12个月随访) 注:LV重塑水平评估内容:功能指标:二尖瓣环应变、E/e′比值、缩短速度、dP/dt、收缩期充盈压力。结构指标:LVESV、LVEDV、室壁应力、CS/LS、心肌纤维化(心脏MRI)。异常提示:若出现心肌应变异常、心室容积增大或纤维化,需升级至高风险并干预。TAVI:经导管主动脉瓣置换术。 -
[1] Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology(ESC)and the European Association for Cardio-Thoracic Surgery(EACTS)[J]. Rev Esp Cardiol(Engl Ed), 2022, 75(6): 524.
[2] Lee JKT, Franzone A, Lanz J, et al. Early detection of subclinical myocardial damage in chronic aortic regurgitation and strategies for timely treatment of asymptomatic patients[J]. Circulation, 2018, 137(2): 184-196. doi: 10.1161/CIRCULATIONAHA.117.029858
[3] Siani A, Perone F, Costantini P, et al. Aortic regurgitation: a multimodality approach[J]. J Clin Ultrasound, 2022, 50(8): 1041-1050. doi: 10.1002/jcu.23299
[4] Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance[J]. J Am Soc Echocardiogr, 2017, 30(4): 303-371. doi: 10.1016/j.echo.2017.01.007
[5] 徐娟, 陈秋兰, 李晓旋, 等. 二维超声心动图结合自动功能成像技术对房颤患者左室收缩功能的初步评价[J]. 中国临床新医学, 2020, 13(6): 587-591.
[6] Lancellotti P, Pibarot P, Chambers J, et al. Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper[J]. Eur Heart J Cardiovasc Imaging, 2022, 23(5): e171-e232. doi: 10.1093/ehjci/jeab253
[7] Zhao QH, Zhang B, Ye YQ, et al. Prognostic impact of left ventricular ejection fraction in patients with moderate aortic regurgitation: potential implications for treatment decision-making[J]. Front Cardiovasc Med, 2021, 8: 800961.
[8] Alashi A, Mentias A, Abdallah A, et al. Incremental prognostic utility of left ventricular global longitudinal strain in asymptomatic patients with significant chronic aortic regurgitation and preserved left ventricular ejection fraction[J]. JACC Cardiovasc Imaging, 2018, 11(5): 673-682. doi: 10.1016/j.jcmg.2017.02.016
[9] Alashi A, Khullar T, Mentias A, et al. Long-term outcomes after aortic valve surgery in patients with asymptomatic chronic aortic regurgitation and preserved LVEF: impact of baseline and follow-up global longitudinal strain[J]. JACC Cardiovasc Imaging, 2020, 13(1 Pt 1): 12-21.
[10] 孙文娜. 左室压力-应变环对冠心病患者左心室心肌做功的定量研究[D]. 大理: 大理大学, 2021.
[11] 江欢欢, 袁新春. 超声新技术评估慢性主动脉瓣反流患者左室心肌功能的研究进展[J]. 实用医学杂志, 2023, 39(19): 2446-2449.
[12] 李皓洁, 保苏丽, 郑丽慧, 等. 左室压力-应变环超声技术在心血管疾病中的应用进展[J]. 临床心血管病杂志, 2024, 40(10): 798-803. doi: 10.13201/j.issn.1001-1439.2024.10.005
[13] 于艾嘉, 刘刚, 吕清. 基于3D-STI左室区域应变参数对室壁运动正常CAD患者的诊断价值[J]. 中国超声医学杂志, 2018, 34(6): 525-528.
[14] Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease[J]. Eur Heart J, 2022, 43(7): 561-632.
[15] Guglielmo M, Pontone G. Risk stratification in cardiomyopathies(dilated, hypertrophic, and arrhythmogenic cardiomyopathy)by cardiac magnetic resonance imaging[J]. Eur Heart J Suppl, 2021, 23(Suppl E): E118-E122.
[16] Rabbat MG, Kwong RY, Heitner JF, et al. The future of cardiac magnetic resonance clinical trials[J]. JACC Cardiovasc Imaging, 2022, 15(12): 2127-2138.
[17] Ko ková R, Línková H, Hlubocká Z, et al. Multiparametric strategy to predict early disease decompensation in asymptomatic severe aortic regurgitation[J]. Circ Cardiovasc Imaging, 2022, 15(12): e014901.
[18] Myerson SG, D'Arcy J, Mohiaddin R, et al. Aortic regurgitation quantification using cardiovascular magnetic resonance: association with clinical outcome[J]. Circulation, 2012, 126(12): 1452-1460.
[19] Malahfji M, Senapati A, Tayal B, et al. Myocardial scar and mortality in chronic aortic regurgitation[J]. J Am Heart Assoc, 2020, 9(23): e018731.
[20] Fernandez-Golfin C, Hinojar-Baydes R, Gonzalez-Gomez A, et al. Prognostic implications of cardiac magnetic resonance feature tracking derived multidirectional strain in patients with chronic aortic regurgitation[J]. Eur Radiol, 2021, 31(7): 5106-5115. doi: 10.1007/s00330-020-07651-6
[21] Ewe SH, Haeck MLA, Ng ACT, et al. Detection of subtle left ventricular systolic dysfunction in patients with significant aortic regurgitation and preserved left ventricular ejection fraction: speckle tracking echocardiographic analysis[J]. Eur Heart J Cardiovasc Imaging, 2015, 16(9): 992-999.
[22] 廖玉华, 杨杰孚, 张健, 等. 舒张性心力衰竭诊断和治疗专家共识[J]. 临床心血管病杂志, 2020, 36(1): 1-10. doi: 10.13201/j.issn.1001-1439.2020.01.001
[23] 刘然, 付贺, 谢萌, 等. 主动脉瓣反流的影像学评估与治疗策略[J]. 中国循环杂志, 2023, 38(5): 573-578.
[24] 中华医学会核医学分会, 中华医学会心血管病学分会. 核素心肌显像临床应用指南(2018)[J]. 中华心血管病杂志, 2019, 47(7): 519-527.
[25] Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines[J]. Circulation, 2021, 143(5): e72-e227.
[26] Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American society of echocardiography[J]. J Am Soc Echocardiogr, 2019, 32(1): 1-64. http://www.zhangqiaokeyan.com/journal-foreign-detail/0704025881983.html
[27] 尹万红, 王小亭, 刘大为, 等. 重症超声临床应用技术规范[J]. 中华内科杂志, 2018, 57(6): 397-417.
[28] 中华医学会超声医学分会超声心动图学组, 中国医师协会心血管分会超声心动图专业委员会. 超声心动图评估心脏收缩和舒张功能临床应用指南[J]. 中华超声影像学杂志, 2020, 29(6): 461-477.
[29] Guglielmo M, Rovera C, Rabbat MG, et al. The role of cardiac magnetic resonance in aortic stenosis and regurgitation[J]. J Cardiovasc Dev Dis, 2022, 9(4): 108.
[30] Dujardin KS, Enriquez-Sarano M, Schaff HV, et al. Mortality and morbidity of aortic regurgitation in clinical practice. A long-term follow-up study[J]. Circulation, 1999, 99(14): 1851-1857.
-

计量
- 文章访问数: 21
- 施引文献: 0



 下载:
下载: