Relationship between the hemodynamic changes of passive leg raising and the death of cardiovascular disease in elderly frail patients
-
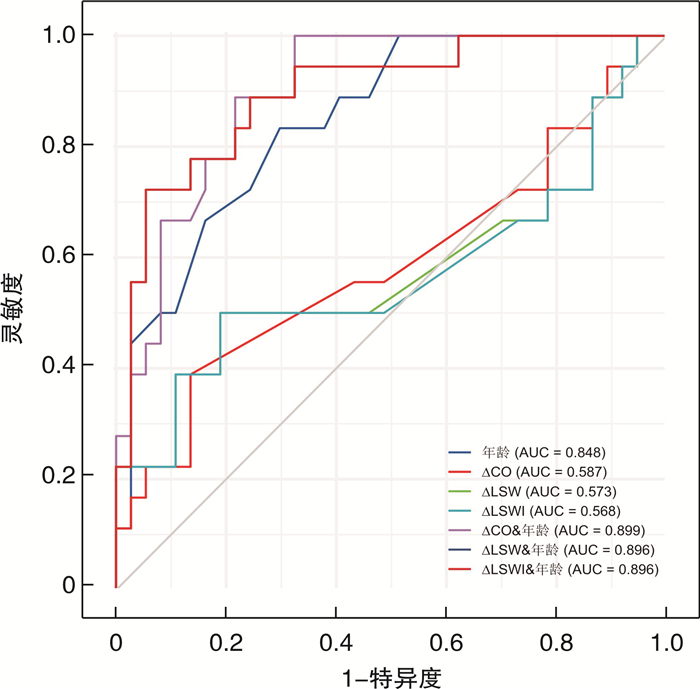
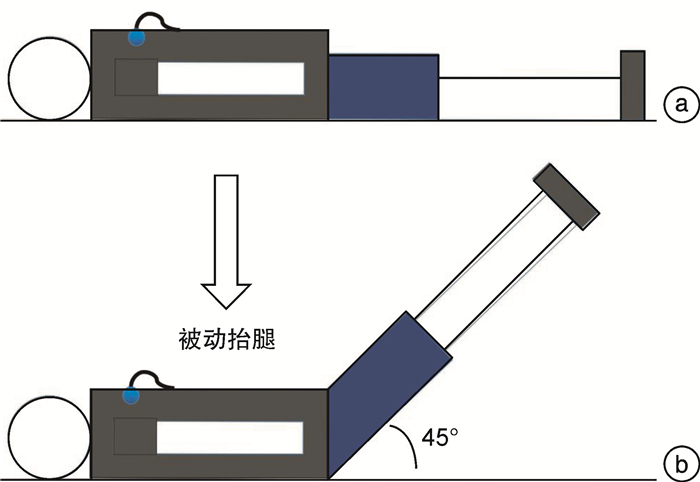
摘要: 目的 探究被动抬腿(PLR)的血流动力学变化与老年衰弱患者心血管病死亡的关系。方法 回顾性纳入2017年6月—2017年11月于我院老年病科住院年龄≥70岁的患者,经筛选得到同时进行过阻抗微分心动图(ICG)检查和进行过衰弱评估并被诊断为衰弱的患者共55例。采用logistic回归分析PLR的血流动力学变化与老年衰弱患者心血管病死亡的关系。受试工作者曲线(ROC)评价PLR的血流动力学指标变化对老年衰弱患者心血管病死亡风险的预测效能。结果 在校正潜在混杂变量后,PLR的心输出量(CO)、左心做功(LSW)、左心做功指数(LSWI)变化的OR值及95%CI分别为0.79(0.64~0.98)、0.77(0.61~0.98)和0.78(0.60~0.97),PLR的CO、LSW、LSWI变化结合年龄预测老年衰弱患者心血管病死亡的ROC曲线下面积分别为0.899、0.896和0.896。结论 PLR的CO、LSW、LSWI变化可能与老年衰弱患者的心血管病死亡风险独立相关,PLR后CO、LSW、LSWI增加,老年衰弱患者心血管病死亡风险下降。Abstract: Objective To explore the relationship between the hemodynamic changes of passive leg raising (PLR) and the death of cardiovascular disease in elderly frail patients.Methods Patients aged ≥70 years were retrospectively included in our geriatrics department from June 2017 to November 2017. And a total of 55 patients who had simultaneously undergone impedance cardiography (ICG) examination and frailty assessment were obtained. The logistic regression analyzed the relationship between PLR hemodynamic changes and cardiovascular death in elderly frail patients.The receiver operator curve (ROC) was applied to evaluate the predictive power of PLR's hemodynamic index.Results After correcting for potential confounding variables, the OR values and 95% confidence intervals of changes in PLR's cardiac output (CO), left stroke work (LSW), and left stroke work index (LSWI) were 0.79(0.64-0.98), 0.77(0.61-0.98), and 0.78(0.60-0.97), respectively. The area under the ROC curve of CO, LSW, and LSWI were 0.899, 0.896, and 0.896, respectively.Conclusion CO, LSW, and LSWI after PLR may be protective factors for cardiovascular death in frail elderly patients.
-
Key words:
- frailty /
- passive leg raising /
- cardiovascular disease /
- death /
- impedance cardiography
-

-
表 1 基线资料
Table 1. baseline data
例(%), M(P25, P75), X±S 项目 对照组(26例) 反应组(29例) P 年龄/岁 79.50(72.00,86.00) 87.00(83.00,91.00) < 0.01 男性 18(69.23) 23(79.31) 0.39 身高/cm 167.00(158.00,169.00) 167.00(160.00,168.00) 0.62 体重/kg 67.00(58.00,71.00) 68.00(60.00,70.00) 0.97 BMI/(kg·m-2) 24.38(23.18,26.04) 24.38(23.03,25.46) 0.54 心率/(次·min-1) 64.92±10.29 71.55±9.68 < 0.05 收缩压/mmHg 124.50(124.00,131.00) 127.00(117.00,138.00) 0.65 舒张压/mmHg 68.00(63.00,69.00) 67.00(63.00,70.00) 0.66 平均动脉压/mmHg 86.30±7.95 87.64±7.78 0.53 LVEF/% 63.12±5.41 60.07±11.48 0.11 合并症 冠心病 22(84.62) 18(62.07) 0.06 房颤 5(19.23) 5(17.24) 1.00 高血压 22(84.62) 17(58.62) < 0.05 贫血 11(42.31) 19(65.52) 0.08 糖尿病 9(34.62) 8(27.59) 0.57 COPD 9(34.62) 10(34.48) 0.99 CKD 3(11.54) 5(17.24) 0.71 骨质疏松 8(30.77) 10(34.48) 0.77 PAD 12(46.15) 12(41.38) 0.72 Hb/(g·L-1) 121.50(110.00,134.00) 109.00(101.00,123.00) < 0.05 ALB/(g·L-1) 40.95(37.00,44.00) 35.60(33.00,38.00) < 0.01 BNP/(pg·mL-1) 175.60(70.50,208.60) 187.20(48.70,251.50) 0.42 BUN/(mmol·L-1) 6.57±2.01 7.14±3.11 0.43 CREA/(μmol·L-1) 93.42±34.42 92.71±42.42 0.95 TC/(mmol·L-1) 4.00±1.01 4.24±1.49 0.50 TG/(mmol·L-1) 1.19(1.00,1.43) 1.36(0.90,1.59) 0.81 HDL-C/(mmol·L-1) 1.03±0.30 0.96±0.31 0.38 LDL-C/(mmol·L-1) 2.28±0.80 2.38±0.76 0.66 FRAIL评分/分 2.46±1.36 3.31±1.49 < 0.05 死亡 10(38.46) 8(27.59) 0.39 表 2 仰卧位血流动力学参数的比较
Table 2. Comparisons of hemodynamic parameters at supine position
X±S 项目 对照组(26例) 反应组(29例) P CO/(L·min-1) 2.97±0.98 2.91±0.91 0.81 CI/(L·min-1·m-2) 1.72±0.51 1.70±0.41 0.89 SV/(mL·beat-1) 48.96±18.31 42.69±14.92 0.17 SVI/(mL·beat-1·m-2) 28.46±9.77 24.69±7.45 0.11 SSVR/(dynes·cm-5) 428.90±161.82 526.83±200.78 0.05 SSVRI/(dyne·cm-5·m-2) 254.48±91.69 303.82±109.77 0.08 LSW/(g·m) 51.27±19.87 45.14±17.74 0.23 LSWI/(g·m·m-2) 29.72±10.35 26.08±9.02 0.17 表 3 PLR试验前后组间血流动力学参数的比较
Table 3. Comparison of hemodynamic parameters between groups before and after PLR test
X±S 项目 对照组(26例) 反应组(29例) 抬腿前 抬腿后 P 抬腿前 抬腿后 P CO/(L·min-1) 2.97±0.98 2.90±0.99 < 0.01 2.91±0.91 3.11±0.94 < 0.01 CI/(L·min-1·m-2) 1.72±0.51 1.68±0.50 < 0.01 1.70±0.47 1.81±0.55 < 0.01 SV/(mL·beat-1) 48.96±18.31 47.74±18.04 < 0.01 42.69±14.92 45.25±15.26 < 0.01 SVI/(mL·beat-1·m-2) 28.46±9.77 27.91±9.59 0.06 24.69±7.45 26.55±8.03 < 0.01 SSVR/(dynes·cm-5) 428.90±161.82 437.68±172.06 0.28 526.83±200.78 501.63±192.80 < 0.01 SSVRI/(dyne·cm-5·m-2) 254.49±91.69 257.95±91.07 0.49 303.82±109.77 290.84±106.25 < 0.01 LSW/(g·m) 51.27±19.87 50.34±19.80 0.11 45.14±17.74 49.35±19.99 < 0.01 LSWI/(g·m·m-2) 29.72±10.35 29.21±10.40 0.14 26.08±9.02 28.53±10.34 < 0.01 心率/(次·min-1) 64.92±10.29 60.08±7.06 < 0.01 71.55±9.68 72.14±17.36 0.84 表 4 PLR试验与衰弱的logistic回归分析
Table 4. Logistic regression analysis of passive leg raising test and frailty
变量 模型1 模型2 模型3 OR(95%CI) P OR(95%CI) P OR(95%CI) P △CO 0.95(0.87~1.04) 0.27 0.82(0.70~0.97) < 0.05 0.79(0.64~0.98) < 0.05 △CI 1.01(0.94~1.10) 0.76 0.95(0.86~1.05) 0.32 0.93(0.82~1.05) 0.24 △SV 0.96(0.89~1.04) 0.34 0.91(0.83~1.00) 0.06 0.89(0.79~1.01) 0.07 △SVI 0.97(0.90~1.06) 0.53 0.91(0.82~1.01) 0.08 0.89(0.77~1.01) 0.08 △SSVR 1.00(0.93~1.08) 0.98 1.02(0.94~1.12) 0.58 1.01(0.91~1.12) 0.80 △SSVRI 1.01(0.94~1.10) 0.78 1.03(0.94~1.14) 0.50 1.02(0.92~1.13) 0.78 △LSW 0.96(0.89~1.03) 0.23 0.88(0.79~0.98) < 0.05 0.77(0.61~0.98) < 0.05 △LSWI 0.96(0.89~1.03) 0.23 0.89(0.80~0.99) < 0.05 0.78(0.60~0.97) < 0.05 注:模型1:未校正;模型2:校正年龄、性别、BMI;模型3:校正年龄、性别、BMI、心率、收缩压、舒张压、Hb、BNP、ALB、冠心病、糖尿病、高血压、房颤、CKD、PAD、贫血、FRAIL评分。 表 5 PLR及其联合年龄预测死亡的准确性
Table 5. Accuracy of PLR and its combined age in predicting death
变量 最佳截断值 AUC(95%CI) 灵敏度 特异度 约登指数 年龄 85.50 0.848(0.746~0.951) 0.83 0.40 0.23 △CO -1.61 0.587(0.412~0.762) 0.39 0.87 0.25 △LSW 0.61 0.573(0.387~0.759) 0.50 0.81 0.31 △LSWI 0.51 0.568(0.381~0.755) 0.50 0.81 0.31 △CO & 年龄 - 0.899(0.820~0.977) 1.00 0.68 0.68 △LSW & 年龄 - 0.896(0.807~0.986) 0.72 0.95 0.67 △LSWI & 年龄 - 0.896(0.807~0.986) 0.72 0.95 0.67 -
[1] Collard RM, Boter H, Schoevers RA, et al. Prevalence of frailty in community-dwelling older persons: a systematic review[J]. J Am Geriatr Soc, 2012, 60(8): 1487-1492. doi: 10.1111/j.1532-5415.2012.04054.x
[2] Ma L, Tang Z, Zhang L, et al. Prevalence of Frailty and Associated Factors in the Community-Dwelling Population of China[J]. J Am Geriatr Soc, 2018, 66(3): 559-564. doi: 10.1111/jgs.15214
[3] GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013[J]. Lancet, 2015, 385(9963): 117-171. doi: 10.1016/S0140-6736(14)61682-2
[4] Villani ER, Tummolo AM, Palmer K, et al. Frailty and atrial fibrillation: A systematic review[J]. Eur J Intern Med, 2018, 56: 33-38. doi: 10.1016/j.ejim.2018.04.018
[5] Dou Q, Wang W, Wang H, et al. Prognostic value of frailty in elderly patients with acute coronary syndrome: a systematic review and meta-analysis[J]. BMC Geriatr, 2019, 19(1): 222. doi: 10.1186/s12877-019-1242-8
[6] Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta-analysis[J]. BMJ Open, 2018, 8(12): e024406. doi: 10.1136/bmjopen-2018-024406
[7] Mudge AM, Pelecanos A, Adsett JA. Frailty implications for exercise participation and outcomes in patients with heart failure[J]. J Am Geriatr Soc, 2021, 69(9): 2476-2485. doi: 10.1111/jgs.17145
[8] Sze S, Pellicori P, Zhang J, et al. Effect of frailty on treatment, hospitalisation and death in patients with chronic heart failure[J]. Clin Res Cardiol, 2021, 110(8): 1249-1258. doi: 10.1007/s00392-020-01792-w
[9] Zheng PP, Yao SM, Shi J, et al. Prevalence and Prognostic Significance of Frailty in Gerontal Inpatients With Pre-clinical Heart Failure: A Subgroup Analysis of a Prospective Observational Cohort Study in China[J]. Front Cardiovasc Med, 2020, 7: 607439. doi: 10.3389/fcvm.2020.607439
[10] Kilkenny MF, Phan HT, Lindley RI, et al. Utility of the Hospital Frailty Risk Score Derived From Administrative Data and the Association With Stroke Outcomes[J]. Stroke, 2021, 52(9): 2874-2881. doi: 10.1161/STROKEAHA.120.033648
[11] Pinho J, Küppers C, Nikoubashman O, et al. Frailty is an outcome predictor in patients with acute ischemic stroke receiving endovascular treatment[J]. Age Ageing, 2021, 50(5): 1785-1791. doi: 10.1093/ageing/afab092
[12] Fan J, Yu C, Guo Y, et al. Frailty index and all-cause and cause-specific mortality in Chinese adults: a prospective cohort study[J]. Lancet Public Health, 2020, 5(12): e650-e660. doi: 10.1016/S2468-2667(20)30113-4
[13] Monnet X, Marik P, Teboul JL. Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis[J]. Intensive Care Med, 2016, 42(12): 1935-1947. doi: 10.1007/s00134-015-4134-1
[14] Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype[J]. J Gerontol A Biol Sci Med Sci, 2001, 56(3): M146-M156. doi: 10.1093/gerona/56.3.M146
[15] Piggott DA, Bandeen-Roche K, Mehta SH, et al. Frailty transitions, inflammation, and mortality among persons aging with HIV infection and injection drug use[J]. AIDS, 2020, 34(8): 1217-1225. doi: 10.1097/QAD.0000000000002527
[16] Wu MY, Li CJ, Hou MF, et al. New Insights into the Role of Inflammation in the Pathogenesis of Atherosclerosis[J]. Int J Mol Sci, 2017, 18(10).
[17] Habigt MA, Krieger M, Gesenhues J, et al. Non-linearity of end-systolic pressure-volume relation in afterload increases is caused by an overlay of shortening deactivation and the Frank-Starling mechanism[J]. Sci Rep, 2021, 11(1): 3353. doi: 10.1038/s41598-021-82791-3
[18] Kayhan N, Bodem JP, Vahl CF, et al. The positive staircase (force-frequency relationship) and the Frank-Starling mechanism are altered in atrial myocardium of patients in end-stage heart failure transplanted for dilative cardiomyopathy[J]. Transplant Proc, 2002, 34(6): 2185-2191. doi: 10.1016/S0041-1345(02)03197-4
[19] Weil J, Eschenhagen T, Hirt S, et al. Preserved Frank-Starling mechanism in human end stage heart failure[J]. Cardiovasc Res, 1998, 37(2): 541-548. doi: 10.1016/S0008-6363(97)00227-7
[20] Sivakorn C, Schultz MJ, Dondorp AM. How to monitor cardiovascular function in critical illness in resource-limited settings[J]. Curr Opin Crit Care, 2021, 27(3): 274-281. doi: 10.1097/MCC.0000000000000830
[21] Zhou HL, Ding L, Mi T, et al. Values of hemodynamic variation in response to passive leg raising in predicting exercise capacity of heart failure with preserved ejection fraction[J]. Medicine(Baltimore), 2016, 95(44): e5322.
[22] 壮可, 丁筱雪, 张云梅, 等. 射血分数降低的心力衰竭患者舒张功能不全与运动耐量的关系[J]. 临床心血管病杂志, 2020, 36(2): 148-152. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202002012.htm
[23] Micek ST, McEvoy C, McKenzie M, et al. Fluid balance and cardiac function in septic shock as predictors of hospital mortality[J]. Crit Care, 2013, 17(5): R246. doi: 10.1186/cc13072
-




 下载:
下载: