Predictive value of homocysteine combined with CRP/Alb ratio on the no-reflow phenomenon after emergency PCI in ST-segment elevation myocardial infarction patients with metabolic syndrome
-
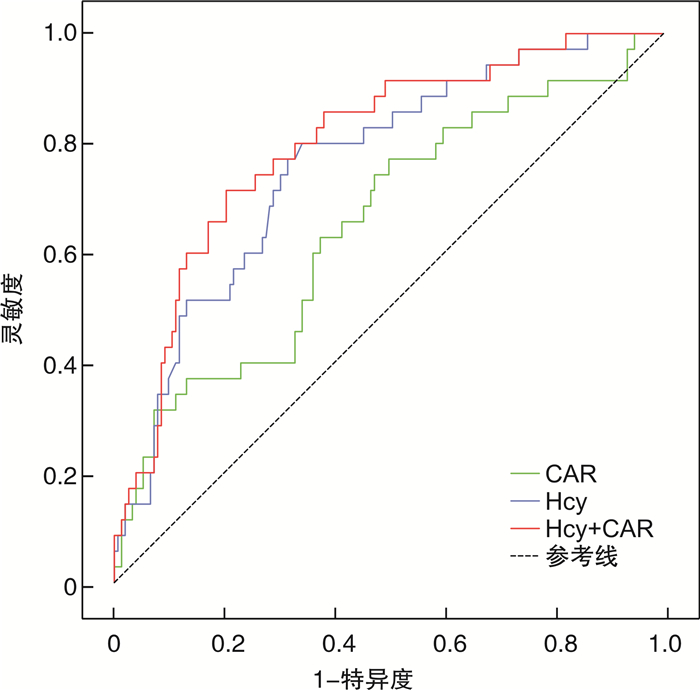
摘要: 目的 探究同型半胱氨酸(Hcy)联合C反应蛋白/白蛋白比值(CAR)对急性ST段抬高型心肌梗死(STEMI)合并代谢综合征(MS)患者急诊行经皮冠状动脉介入(PCI)术后无复流(NRP)的预测价值。方法 连续收集2017年12月—2019年10月于宁夏医科大学总医院行急诊PCI术的STEMI合并MS患者187例,根据冠脉造影结果分为正常血流组(152例)和NRP组(35例),比较2组一般资料及临床特征。采用单因素和多因素logistic回归分析NRP的影响因素,绘制ROC曲线评估Hcy、CAR及两者联合对NRP的预测效能。结果 纳入患者187例,NRP发生率为18.71%。通过调整混杂因素后,二元Logistic回归显示术前Hcy(OR=1.053,95%CI:1.027~1.081,P< 0.001),CAR(OR=2.745,95%CI:1.029~7.322,P=0.044),舒张压(OR=0.959,95%CI:0.926~0.993,P=0.018)及梗死血管RCA(OR=0.378,95%CI:0.148~0.963,P=0.042)是NRP发生的危险因素。在NRP预测中,Hcy在ROC曲线下面积为0.761(95%CI:0.676~0.845),灵敏度为80%,特异度为65.2%,最佳临界值为18.86μmol/L;CAR在ROC曲线下面积为0.652(95%CI:0.549~0.755),灵敏度为77.1%,特异度为50%,最佳临界值为0.167。Hcy联合CAR(联合预测因子)在ROC曲线下面积为0.799(95%CI:0.719~0.878),灵敏度为71.4%,特异度为80.6%。结论 Hcy、CAR是STEMI合并MS患者发生NRP的危险因素,二者联合检测有助于NRP的早期识别。
-
关键词:
- 同型半胱氨酸 /
- C反应蛋白/白蛋白 /
- 无复流 /
- 代谢综合征 /
- ST段抬高型心肌梗死
Abstract: Objective To investigate the predictive value of homocysteine(Hcy) combined with C-reactive protein/albumin ratio(CAR) on the no-reflow phenomenon(NRP) after emergency percutaneous coronary intervention in acute ST-segment elevation myocardial infarction with metabolic syndrome(MS).Methods One hundred and eighty-seven STEMI patients with MS treated with emergency PCI at Ningxia Medical University General Hospital from December 2017 to October 2019 were consecutively selected. According to coronary angiography results, they were divided into two groups: the normal flow group(n=152) and the no-reflow group(n=35). The general dates and clinical characteristics of the two groups were compared. Binary-way logistic regression was used to analyze the independent factors of NRP, and ROC curves were performed to assess the predictive efficacy of HCY, CAR, and the combined factors on NRP.Results The incidence of NRP was 18.71% in 187 included patients. After adjusting for confounding factors, binary-logistic regression showed that Hcy(OR=1.053, 95%CI: 1.027~1.081,P< 0.001), CAR(OR=2.745, 95%CI: 1.029~7.322,P=0.044), diastolic blood pressure level(OR=0.959, 95%CI: 0.926~0.993,P=0.018) and infarct vessel RCA(OR=0.378, 95%CI: 0.148~0.963,P=0.042) were independent predictors of no-reflow. In the predictive value of no-reflow, the area under the ROC curve(AUC) of Hcy was 0.761(95%CI: 0.676~0.845), its sensitivity was 80% and specificity was 65.2%, and the best critical value was 18.86μmol/L. The AUC of CAR was 0.652(95%CI: 0.549~0.755), its sensitivity was 77.1% and specificity was 50%, and the critical value was 0.167. The AUC of Hcy combined with CAR was 0.799(95%CI: 0.719~0.878), its sensitivity was 71.4% and specificity was 80.6%.Conclusion Hcy and CRP/Alb are independent predictors of the no-reflow phenomenon.Hcy combined CAR is a better factor to predict the NRP in acute ST-elevation myocardial infarction with metabolic syndrome after PCI, and can help in the early identification of NRP. -

-
表 1 2组基线资料比较
Table 1. Comparison of baseline characteristics between two groups
例(%), X±S 项目 血流正常组(152例) NRP组(35例) χ2/t P 年龄/岁 69.61±12.21 63.57±12.89 1.712 0.089 男性 119(78.28) 24(68.57) 1.493 0.222 高血压病 120(78.94) 32(91.43) 2.913 0.088 糖尿病 88(57.89) 19(54.28) 0.151 0.697 高脂血症 74(48.68) 15(42.86) 4.486 0.534 吸烟史 95(62.50) 20(57.14) 0.387 0.557 冠心病家族史 38(25.00) 3(8.57) 4.486 0.034 BMI/(kg·m-2) 26.00±3.31 25.48±3.52 -0.835 0.405 入院心率/(次·min-1) 79.70±12.56 83.14±18.63 1.325 0.187 入院SBP/mmHg 126.58±21.54 109.29±20.15 -4.296 < 0.001 入院DBP/mmHg 79.07±13.77 69.11±13.92 -3.848 < 0.001 入院Killip分级 4.272 0.234 Ⅰ级 127(83.55) 25(71.43) Ⅱ~Ⅳ级 25(16.45) 10(28.57) 表 2 2组血液生化及心脏彩超相关资料比较
Table 2. Comparison of laboratory and echocardiography results between two groups
X±S 项目 血流正常组(152例) NRP组(35例) t P值 Hcy/(μmol·L-1) 20.38±12.41 33.19±19.65 4.872 0.000 CRP/(mg·dL-1) 13.24±5.21 15.91±4.67 2.179 0.031 Alb/(g·L-1) 39.45±4.17 36.57±8.46 -2.942 0.004 CAR 0.26±0.03 0.50±0.10 3.129 0.002 TG/(mmol·L-1) 2.82±1.50 2.69±1.80 -0.465 0.643 TC/(mmol·L-1) 4.22±0.87 4.37±0.79 0.898 0.370 LDL/(mmol·L-1) 1.99±0.61 2.06±0.61 0.600 0.550 HDL/(mmol·L-1) 0.79±0.14 0.84±0.17 1.556 0.121 入院血糖//(mmol·L-1) 9.53±4.48 10.25±5.10 0.831 0.407 白细胞总数/(×109·L-1) 11.31±3.35 11.85±3.65 0.838 0.643 中性粒细胞计数/(×109·L-1) 9.22±3.28 9.85±3.69 0.987 0.325 淋巴细胞计数/(×109·L-1) 1.46±0.67 1.36±0.67 -0.793 0.429 血红蛋白/(g·dL-1) 147.45±18.90 140.75±19.17 -1.887 0.061 血小板计数/(×109·L-1) 233.93±67.79 230.40±54.46 -0.288 0.774 血肌酐/(μmol·L-1) 69.71±18.55 75.25±24.64 1.491 0.138 D-二聚体/(ng·mL-1) 0.58±0.45 0.52±0.45 0.670 0.504 LVEF/% 52.16±7.61 50.48±7.41 -1.063 0.289 表 3 2组介入相关数据比较
Table 3. Comparison of Intervention related data between two groups
例(%), X±S 项目 血流正常组(152例) NRP组(35例) χ2/t P 病变血管数量 0.902 0.342 1支 44(28.95) 13(37.14) >1支 108(71.05) 22(62.86) 术前TIMI血流 1.527 0.408 0~1级 143(94.08) 33(94.28) 2~3级 9(9.21) 2(11.43) 梗死相关动脉 LAD 68(44.74) 10(28.57) 0.058 0.080 LCX 19(12.50) 2(5.71) 1.514 0.252 RCA 65(42.76) 23(65.71) 6.015 0.014 IABP 35(23.03) 9(25.71) 0.981 0.401 血栓抽吸 32(21.05) 7(20.00) 0.837 0.272 支架数量/个 1.49±0.76 1.43±0.66 2.973 0.643 支架直径/mm 3.22±0.46 3.38±0.45 1.954 0.052 支架长度/mm 25.85±7.83 26.34±8.45 0.332 0.741 表 4 NRP现象的单因素logistic回归分析
Table 4. Univariate logistic analysis of no-reflow phenomenon
变量 B S.E. Wald OR 95%CI P SBP -0.039 0.010 15.380 0.962 0.943~0.981 0.001 DBP -0.057 0.016 12.864 0.945 0.916~0.975 < 0.001 CRP 0.023 0.012 3.917 1.024 1.002~1.048 0.048 Alb -0.089 0.036 6.253 0.915 0.853~0.981 0.012 CAR 1.088 0.422 6.651 2.967 1.298~6.781 0.010 Hcy 0.047 0.012 16.272 1.048 1.024~1.072 < 0.001 RCA -0.942 0.392 5.775 0.390 0.181~0.841 0.016 冠心病家族史 -1.269 0.632 4.029 0.281 0.081~0.971 0.045 表 5 NRP现象的多因素logistic回归分析
Table 5. Multivariate logistic analysis of no-reflow phenomenon
变量 B S.E. Wald OR 95%CI P DBP -0.042 0.018 5.580 0.959 0.926~0.993 0.018 CAR 1.010 0.501 4.069 2.745 1.029~7.322 0.044 Hcy 0.052 0.013 15.532 1.053 1.027~1.081 < 0.001 RCA -0.973 0.477 4.153 0.378 0.148~0.963 0.042 -
[1] Kim LK, Yoon JW, Lee DH, et al. Impact of metabolic syndrome on the progression of coronary calcium and of coronary artery disease assessed by repeated cardiac computed tomography scans[J]. Cardiovasc Diabetol, 2016, 15: 92. doi: 10.1186/s12933-016-0404-7
[2] 李云龙, 岳佳, 唐刚, 等. 代谢综合征与老年急性心肌梗死严重程度的相关性分析[J]. 中华老年心脑血管病杂志, 2020, 22(9): 920-923. doi: 10.3969/j.issn.1009-0126.2020.09.007
[3] Lovic MB, Savic L, Matic D, et al. Predictive value of metabolic syndrome definitions in patients with myocardial infarction with ST segment elevation-are they all the same?[J]. Acta Cardiol, 2018, 73(6): 574-582. doi: 10.1080/00015385.2018.1424599
[4] Pantea-Roşan LR, Pantea VA, Bungau S, et al. No-Reflow after PPCI-A Predictor of Short-Term Outcomes in STEMI Patients[J]. J Clin Med, 2020, 9(9).
[5] Zhou FZ, Song W, Yin LH, et al. Effects of remote ischemic preconditioning on myocardial injury and endothelial function and prognosis after percutaneous coronary intervention in patients with acute coronary syndrome[J]. Eur Rev Med Pharmacol Sci, 2017, 21(20): 4642-4648.
[6] 樊丹丹, 姚芳兰, 屈慧, 等. 同型半胱氨酸预测急性心肌梗死冠脉病变的研究[J]. 临床急诊杂志, 2021, 22(4): 265-270. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202104009.htm
[7] Karabaǧ Y, Çaǧdaş M, Rencuzogullari I, et al. Usefulness of The C-Reactive Protein/Albumin Ratio for Predicting No-Reflow in ST-elevation myocardial infarction treated with primary percutaneous coronary intervention[J]. Eur J Clin Invest, 2018, 48(6): e12928. doi: 10.1111/eci.12928
[8] Plakht Y, Gilutz H, Shiyovich A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction Ⅱ(SAMI-Ⅱ)project[J]. Int J Cardiol, 2016, 219: 20-24. doi: 10.1016/j.ijcard.2016.05.067
[9] Söǧüt Ö, Akdemir T, Can MM. Prognostic value of the C-reactive protein to albumin ratio in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction[J]. Turk J Med Sci, 2021, 51(3): 1281-1288. doi: 10.3906/sag-2003-188
[10] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 国际内分泌代谢杂志, 2021, 41(5): 482-548. doi: 10.3760/cma.j.cn121383-20210825-08063
[11] Tasar O, Karabay AK, Oduncu V, et al. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Coron Artery Dis, 2019, 30(4): 270-276. doi: 10.1097/MCA.0000000000000726
[12] 张若青. 血脂代谢特征与冠心病合并代谢综合征患者冠脉狭窄程度的关系[J]. 中国老年学杂志, 2014, 34(21): 6055-6057. doi: 10.3969/j.issn.1005-9202.2014.21.55
[13] 谢瑾, 李红, 罗浩. 合并MS冠心病患者细胞因子表达及临床意义[J]. 分子诊断与治疗杂志, 2020, 12(2): 221-224. doi: 10.3969/j.issn.1674-6929.2020.02.023
[14] Tartan Z, Ozer N, Uyarel H, et al. Metabolic syndrome is a predictor for an ECG sign of no-reflow after primary PCI in patients with acute ST-elevation myocardial infarction[J]. Nutr Metab Cardiovasc Dis, 2008, 18(6): 441-447. doi: 10.1016/j.numecd.2007.02.015
[15] Miñana G, Gil-Cayuela C, Fácila L, et al. Homocysteine and long-term recurrent infarction following an acute coronary syndrome[J]. Cardiol J, 2021, 28(4): 598-606. doi: 10.5603/CJ.a2020.0170
[16] Marcucci R, Betti I, Cecchi E, et al. Hyperhomocysteinemia and vitamin B6 deficiency: new risk markers for nonvalvular atrial fibrillation?[J]. Am Heart J, 2004, 148(3): 456-461. doi: 10.1016/j.ahj.2004.03.017
[17] Li L, Hasegawa H, Inaba N, et al. Diet-induced hyperhomocysteinemia impairs vasodilation in 5/6-nephrectomized rats[J]. Amino Acids, 2018, 50(10): 1485-1494. doi: 10.1007/s00726-018-2626-3
[18] Szabo C. Hydrogen sulfide, an enhancer of vascular nitric oxide signaling: mechanisms and implications[J]. Am J Physiol Cell Physiol, 2017, 2017, 312(1) C3-C15.
[19] Balint B, Jepchumba VK, Guéant JL, et al. Mechanisms of homocysteine-induced damage to the endothelial, medial and adventitial layers of the arterial wall[J]. Biochimie, 2020, 173: 100-106. doi: 10.1016/j.biochi.2020.02.012
[20] 任宇波, 李小明. 同型半胱氨酸与冠状动脉病变的相关性研究进展[J]. 岭南心血管病杂志, 2020, 26(4): 485-488. doi: 10.3969/j.issn.1007-9688.2020.04.25
[21] Quispe R, Michos ED, Martin SS, et al. High-Sensitivity C-Reactive Protein Discordance With Atherogenic Lipid Measures and Incidence of Atherosclerotic Cardiovascular Disease in Primary Prevention: The ARIC Study[J]. J Am Heart Assoc, 2020, 9(3): e013600. doi: 10.1161/JAHA.119.013600
[22] 王宗方, 柏战, 阮爱兵, 等. 纤维蛋白原与白蛋白比值和D-二聚体对冠状动脉慢血流现象的预测价值[J]. 临床心血管病杂志, 2021, 37(10): 901-904. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202110006.htm
[23] 高秀鑫, 刘逸翔, 丁振江, 等. 纤维蛋白原与白蛋白比值对PCI术后的急性冠脉综合征患者预后的影响[J]. 临床心血管病杂志, 2021, 37(8): 763-768. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202108018.htm
[24] 曾令泽, 陈媛, 吴胤松, 等. 急性冠状动脉综合征患者PCI术后冠脉无复流机制及治疗进展[J]. 中国循证心血管医学杂志, 2021, 13(9): 1148-1149, 1152. doi: 10.3969/j.issn.1674-4055.2021.09.35
[25] Hibi K, Kozuma K, Sonoda S, et al. A Randomized Study of Distal Filter Protection Versus Conventional Treatment During Percutaneous Coronary Intervention in Patients With Attenuated Plaque Identified by Intravascular Ultrasound[J]. JACC Cardiovasc Interv, 2018, 11(16): 1545-1555. doi: 10.1016/j.jcin.2018.03.021
[26] 张希, 王一涵, 鲁思彤. 替格瑞洛与氯吡格雷对老年冠心病患者HCY、hs-CRP、IL-6水平的影响[J]. 当代医学, 2021, 27(28): 4-6. doi: 10.3969/j.issn.1009-4393.2021.28.002
[27] Verdoia M, Rolla R, Negro F, et al. Homocysteine levels and platelet reactivity in coronary artery disease patients treated with ticagrelor[J]. Nutr Metab Cardiovasc Dis, 2020, 30(2): 292-299. doi: 10.1016/j.numecd.2019.09.018
[28] 白洁, 杨帮国, 韩谨阳. 替罗非班对冠心病经皮冠状动脉介入术后患者的临床研究[J]. 中国临床药理学杂志, 2019, 35(23): 2967-2970. https://www.cnki.com.cn/Article/CJFDTOTAL-GLYZ201923004.htm
[29] 宋琼, 毕丽丽, 张金杰, 等. 阿托伐他汀对冠状动脉无复流作用机制的研究进展[J]. 医药导报, 2021, 40(5): 641-644. https://www.cnki.com.cn/Article/CJFDTOTAL-YYDB202105018.htm
[30] Polimeni A, De Rosa S, Sabatino J, et al. Impact of intracoronary adenosine administration during primary PCI: A meta-analysis[J]. Int J Cardiol, 2016, 203: 1032-1041. doi: 10.1016/j.ijcard.2015.11.086
[31] The REFLO-STEMI(REperfusion Facilitated by LOcal adjunctive therapy in ST-Elevation Myocardial Infarction)trial: a randomised controlled trial comparing intracoronary administration of adenosine or sodium nitroprusside with control for attenuation of microvascular obstruction during primary percutaneous coronary intervention[M]. Southampton(UK): NIHR Journals Library, 2016.
-




 下载:
下载: