Correlation between clot lysis time based on thromboelastogram and recurrent myocardial infarction in patients with acute coronary syndrome and hyperlipidemia
-
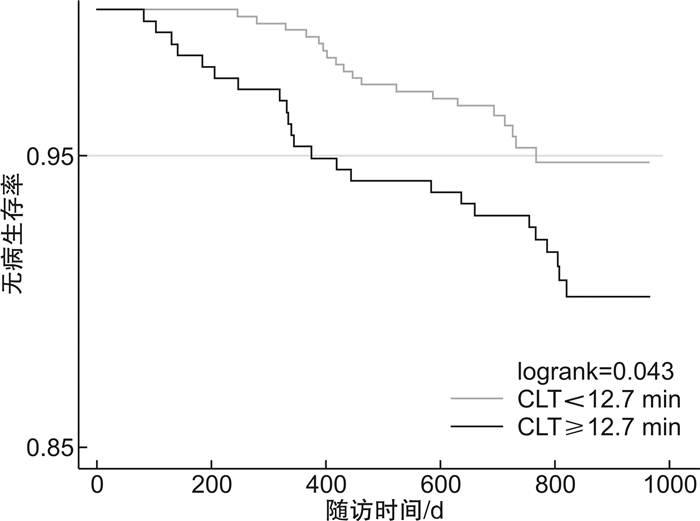
摘要: 目的 探讨凝块溶解时间(CLT)与急性冠状动脉综合征(ACS)合并高脂血症患者再发心肌梗死(心梗)事件风险的关系。方法 纳入2019年1月—2020年2月于北京安贞医院住院确诊为ACS且出院前行血栓弹力图检测的患者,共计909例。收集研究对象的人口学特征、临床检测结果并对其进行电话随访,中位随访时间为2年。根据患者出院诊断及既往病史将其分为ACS高脂血症组(685例)和ACS非高脂血症组(224例)。通过多因素logistic回归模型分析CLT与ACS合并高脂血症患者再发心梗事件的关系,并利用受试者工作特征(ROC)曲线评价CLT对患者再发心梗事件的评估效能。使用Kaplan-Meier方法计算生存曲线。结果 ACS高脂血症组患者出院前CLT值高(P=0.007)。多因素logistic回归模型显示,调整病史、合并症及临床检验指标等后,CLT与ACS高脂血症患者再发心梗事件发生风险独立相关(OR=1.45,95%CI:1.06-2.00,P=0.020)。ROC曲线分析得到CLT评估ACS高脂血症患者再发心梗事件风险的最佳截止点为12.7 min,Kaplan-Meier生存曲线分析结果表明CLT≥12.7 min组再发心梗发生率显著高于CLT < 12.7 min组(Log rank:P=0.043)。结论 CLT可评估ACS合并高脂血症患者出院后发生再发心梗事件风险。Abstract: Objective To investigate the relationship between clot lysis time(CLT) and the risk of recurrence of myocardial infarction events in patients with acute coronary syndrome and hyperlipidemia.Methods A total of 909 patients who were hospitalized with acute coronary syndrome were included in Beijing Anzhen Hospital from January 2019 to February 2020. And these patients also underwent thromboelastography(TEG) testing before discharge. Their clinical characteristics and serum markers were collected. Patients were followed up by telephone and the median duration of follow-up was 2 years. The patients were divided into ACS hyperlipidemia group(n=685) and ACS non-hyperlipidemia group(n=224) according to their diagnosis at discharge and past medical history. The relationship between CLT and recurrent myocardial infarction event in ACS patients with hyperlipidemia was analyzed by multivariate logistic regression model, and the receiver operating characteristic(ROC) curve was used to evaluate the efficacy of CLT in evaluation of recurrent myocardial infarction. Survival analysis was performed using Kaplan-Meier survival curve.Results The CLT value before discharge was higher in the ACS hyperlipidemia group(P=0.007). Multivariate logistic regression model showed that after adjusting medical history, comorbidities and clinical test indicators, CLT was independently associated with the risk of recurrent myocardial infarction in patients with ACS hyperlipidemia(OR=1.45, 95%CI: 1.06-2.00, P=0.020). The ROC curve analysis showed that the optimal cutoff point for CLT to assess the risk of recurrent myocardial infarction in patients with ACS hyperlipidemia was 12.7 min. The Kaplan-Meier survival curve analysis showed that the incidence of recurrent myocardial infarction in the CLT ≥ 12.7 min group was significantly higher than that in the CLT group < 12.7 min group(Log rank: P=0.043).Conclusion CLT can assess the risk of recurrent myocardial infarction in patients with ACS complicated with hyperlipidemia after discharge.
-
Key words:
- acute coronary syndrome /
- hyperlipidemia /
- thromboelastogram /
- prognosis research
-

-
表 1 ACS高脂血症组与非高脂血症组基线临床特征比较
Table 1. Baseline clinical characteristics in Hyperlipidemia Group and Non-Hyperlipidemia Group
X±S 项目 ACS非高脂血症组(224例) ACS高脂血症组(685例) P值 男性/例(%) 177(79.02) 518(75.62) 0.298 年龄/岁 62.51±10.26 60.69±10.14 0.020 BMI/(kg·m-2) 25.73±9.74 24.38±6.90 0.023 病史或合并症 吸烟/例(%) 80(35.71) 245(35.77) 0.989 高血压/例(%) 135(60.27) 451(65.84) 0.130 糖尿病/例(%) 88(39.29) 232(33.87) 0.141 ST段改变/例(%) 8(3.57) 106(15.47) <0.001 既往心梗/例(%) 31(13.84) 111(16.20) 0.397 既往卒中/例(%) 42(18.75) 76(11.09) 0.003 外周血管病/例(%) 16(7.14) 26(3.80) 0.038 肾功能不全/例(%) 5(2.23) 14(2.04) 0.864 实验室检查 白细胞计数/(×109·L-1) 7.46±1.82 7.78±2.50 0.241 血红蛋白/(ng·L-1) 141.38±17.26 143.85±17.29 0.160 BNP/(pg·mL-1) 111.80±237.06 93.41±146.10 0.489 CRP/(mg·L-1) 3.47±5.32 4.22±7.77 0.072 肌酐/(μmol·L-1) 81.70±55.97 78.93±42.52 0.235 血糖/(mmol·L-1) 7.52±3.43 7.44±3.14 0.940 糖化血红蛋白/% 6.67±1.28 6.69±2.95 0.601 甘油三酯/(mmol·L-1) 1.54±1.03 1.71±1.27 0.038 总胆固醇/(mmol·L-1) 3.79±0.98 4.12±1.04 <0.001 高密度脂蛋白/(mmol·L-1) 1.00±0.24 1.05±0.25 0.008 低密度脂蛋白/(mmol·L-1) 2.25±0.85 2.46±0.88 0.001 CLT/min 12.93±16.76 16.61±17.90 0.007 结局事件发生率 再发心梗/例(%) 5(2.23) 43(6.28) 0.019 表 2 按CLT截断值分组一般临床资料比较
Table 2. General clinical data across groups CLT cutoff value
X±S 项目 CLT<12.7 min组(429例) CLT≥12.7 min组(256例) P值 男性/例(%) 318(74.13) 200(78.13) 0.238 年龄/岁 60.89±9.74 60.35±10.80 0.500 BMI/(kg·m-2) 25.54±4.63 22.44±9.27 <0.001 病史或合并症 吸烟/例(%) 145(33.80) 100(39.06) 0.164 高血压/例(%) 285(66.43) 166(64.84) 0.671 糖尿病/例(%) 153(35.66) 79(30.86) 0.199 ST段改变/例(%) 18(4.20) 88(34.38) <0.001 既往心梗/例(%) 64(14.92) 47(18.36) 0.237 既往卒中/例(%) 51(11.89) 25(9.77) 0.392 外周血管病/例(%) 17(3.96) 9(3.52) 0.767 肾功能不全/例(%) 4(0.93) 10(3.91) 0.008 实验室检查 白细胞计数/(×109·L-1) 7.32±2.01 8.54±3.00 <0.001 血红蛋白/(ng·L-1) 143.07±16.10 145.17±19.07 0.505 BNP/(pg·mL-1) 67.62±95.20 137.50±198.43 <0.001 CRP/(mg·L-1) 3.11±4.47 6.20±11.24 <0.001 肌酐/(μmol·L-1) 76.61±29.26 82.82±58.27 0.049 血糖/(mmol·L-1) 7.12±2.96 7.97±3.36 0.001 糖化血红蛋白/% 6.72±3.53 6.65±1.49 0.737 甘油三酯/(mmol·L-1) 1.66±1.15 1.79±1.44 0.246 总胆固醇/(mmol·L-1) 3.97±0.97 4.38±1.12 <0.001 高密度脂蛋白/(mmol·L-1) 1.05±0.24 1.06±0.27 0.584 低密度脂蛋白/(mmol·L-1) 2.36±0.83 2.65±0.94 0.001 结局事件发生率 再发心梗/例(%) 19(4.43) 24(9.38) 0.010 表 3 CLT与血脂指标的Pearson相关性分析
Table 3. Pearson correlation analysis of CLT and lipid indexes
项目 r P值 甘油三酯 0.052 0.120 总胆固醇 0.200 <0.001 高密度脂蛋白 0.067 0.045 低密度脂蛋白 0.163 <0.001 表 4 CLT与结局事件的logistic回归分析
Table 4. logistic regression analysis of CLT and endpoint
项目 单因素分析 多因素分析 模型1 模型2 OR(95%CI) P值 OR(95%CI) P值 OR(95%CI) P值 log CLT 1.35(1.05~1.74) 0.019 1.35(1.04~1.75) 0.022 1.45(1.06~2.00) 0.020 模型1包括变量:性别、年龄、BMI、吸烟史、高血压、糖尿病、既往卒中、肾功能不全;模型2包括变量:性别、年龄、BMI、吸烟史、高血压、糖尿病、既往卒中、肾功能不全、白细胞计数、血红蛋白、B型钠尿肽、C反应蛋白、肌酐、血糖、糖化血红蛋白、甘油三酯、总胆固醇、高密度脂蛋白、低密度脂蛋白。 -
[1] 中国医师协会急诊医师分会, 国家卫健委能力建设与继续教育中心急诊学专家委员会, 中国医疗保健国际交流促进会急诊急救分会. 急性冠脉综合征急诊快速诊治指南(2019)[J]. 中华急诊医学杂志, 2019, 28(4): 421-428. doi: 10.3760/cma.j.issn.1671-0282.2019.04.003
[2] Schüpke S, Neumann FJ, Menichelli M, et al. Ticagrelor or prasugrel in patients with acute coronary syndromes[J]. N Engl J Med, 2019, 381: 1524-1534. doi: 10.1056/NEJMoa1908973
[3] 宋峥, 苏文, 崔天盆, 等. 基于脂质代谢的体质特征与冠心病发生的关系研究[J]. 临床急诊杂志, 2020, 21(8): 659-662. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202008013.htm
[4] Zhu YH, Xian XM, Wang ZZ, et al. Research progress on the relationship between atherosclerosis and inflammation[J]. Biomolecules, 2018, 8: 111. doi: 10.3390/biom8040111
[5] Shapiro MD, Fazio S. From lipids to inflammation: new approaches to reducing atherosclerotic risk[J]. Circ Res, 2016, 118: 732-749. doi: 10.1161/CIRCRESAHA.115.306471
[6] Basurto L, Sánchez L, Díaz A, et al. Differences between metabolically healthy and unhealthy obesity in PAI-1 level: Fibrinolysis, body size phenotypes and metabolism[J]. Thromb Res, 2019, 180: 110-114. doi: 10.1016/j.thromres.2019.06.013
[7] Gorog DA, Prognostic value of plasma fibrinolysis activation markers in cardiovascular disease[J]. J Am Coll Cardiol, 2010, 55: 2701-2709. doi: 10.1016/j.jacc.2009.11.095
[8] Mackman N, Bergmeier W, Stouffer GA, et al. Therapeutic strategies for thrombosis: new targets and approaches[J]. Nat Rev Drug Discov, 2020, 19: 333-352. doi: 10.1038/s41573-020-0061-0
[9] Burton AG, Jandrey KE, Use of thromboelastography in clinical practice[J]. Vet Clin North Am Small Anim Pract, 2020, 50: 1397-1409. doi: 10.1016/j.cvsm.2020.08.001
[10] Santos GCG, Picatoste B, Badimón JJ, Pathophysiology of acute coronary syndrome. [J]. Curr Atheroscler Rep, 2014, 16: 401. doi: 10.1007/s11883-014-0401-9
[11] Zhong SS, Li LX, Shen X, et al. An update on lipid oxidation and inflammation in cardiovascular diseases[J]. Free Radic Biol Med, 2019, 144: 266-278. doi: 10.1016/j.freeradbiomed.2019.03.036
[12] Andreotti F, Navarese P, Crea F, et al. Prolonged endogenous fibrinolysis predicts reduced survival after acute coronary syndromes[J]. Eur Heart J, 2018, 39: 1086-1088. doi: 10.1093/eurheartj/ehy118
[13] Wohner N, Sótonyi P, Machovich R, et al. Lytic resistance of fibrin containing red blood cells[J]. Arterioscler Thromb Vasc Biol, 2011, 31: 2306-2313. doi: 10.1161/ATVBAHA.111.229088
[14] Carrieri C, Galasso R, Semeraro F, et al. The role of thrombin activatable fibrinolysis inhibitor and factor XI in platelet-mediated fibrinolysis resistance: a thromboelastographic study in whole blood[J]. J Thromb Haemost, 2011, 9: 154-162. doi: 10.1111/j.1538-7836.2010.04120.x
[15] Konings J, Hoving LR, Ariёns RS, et al. The role of activated coagulation factor XⅡ in overall clot stability and fibrinolysis[J]. Thromb Res, 2015, 136: 474-480. doi: 10.1016/j.thromres.2015.06.028
[16] 张本蓉, 谢成兵. 血栓弹力图联合D-二聚体/纤维蛋白(原)降解产物比值检测在脓毒症并发弥散性血管内凝血患者中的应用价值研究[J]. 临床急诊杂志, 2021, 22(1): 31-35. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202101007.htm
[17] Kott Katharine A, Morel-Kopp MC, Vernon ST, et al. Association of global coagulation profiles with cardiovascular risk factors and atherosclerosis: a sex disaggregated analysis from the BioHEART-CT Study[J]. J Am Heart Assoc, 2021, 90: e020604.
[18] Leibundgut G, Arai K, Orsoni A, et al. Oxidized phospholipids are present on plasminogen, affect fibrinolysis, and increase following acute myocardial infarction[J]. J Am Coll Cardiol, 2012, 59: 1426-1437. doi: 10.1016/j.jacc.2011.12.033
-




 下载:
下载: