Predictive value of FIB-4 Index in stent restenosis after PCI in patients with acute myocardial infarction
-
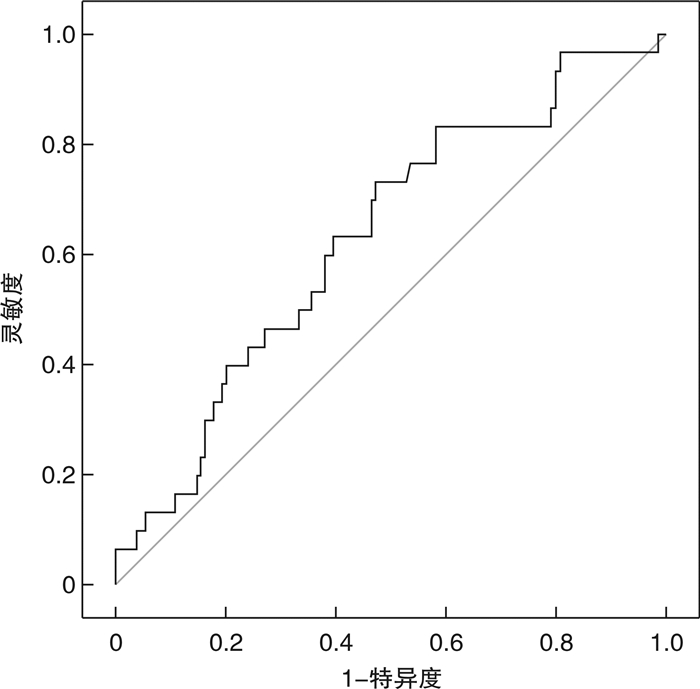
摘要: 目的 探讨FIB-4指数预测急性心肌梗死(AMI)患者冠状动脉介入(PCI)术后支架内再狭窄(ISR)的价值。方法 选取我院心内科确诊为AMI并行PCI术的患者159例,根据随访冠状动脉造影结果分为无支架内再狭窄(NISR)组及ISR组。比较两组基本临床资料、手术资料、PCI术后服药情况、PCI前及随访时实验室结果等。采用多因素logistic回归分析发生ISR的相关因素,ROC曲线评价FIB-4预测ISR临床价值。结果 两组年龄、性别、高血压、糖尿病、术后服用药物及PCI前实验室结果等比较均无统计学差异(P>0.05)。与NISR组相比,ISR组行急诊PCI比例低(P<0.05)。ISR组随访时HDL-C水平及FIB-4指数显著高于NISR组(P<0.05)。多因素logistic回归分析显示,随访时FIB-4指数(OR=3.022,P=0.032)是ISR发生的独立危险因素。随访时FIB-4指数ROC曲线下面积为0.632(95%CI:0.524~0.740,P=0.024),诊断临界值为0.474,灵敏度为73.3%,特异度为52.7%。结论 PCI术后随访时FIB-4指数是发生ISR的危险因素。Abstract: Objective To explore the predictive value of FIB-4 index in stent restenosis after percutaneous transluminal coronary intervention(PCI) in patients with acute myocardial infarction(AMI).Methods A total of 159 patients with AMI received PCI in our hospital from June 2018 to October 2020. According to the results of re-examined for coronary angiography, they were divided into non-stent restenosis group(NISR group) and in-stent restenosis group(ISR group). The basic clinical data, surgical data, medications after PCI, laboratory results before the PCI and follow-up were compared. The multivariate logistic regression was used to analyze the related factors of ISR, and the ROC curve was used to evaluate FIB-4 to the clinical value of ISR.Results There were no significant differences in age, gender, hypertension, diabetes, postoperative drug use and laboratory results before PCI between the two groups(P> 0.05). Compared with the NISR group, the rate of emergency PCI in the ISR group was lower(P< 0.05). The HDL-C level and FIB-4 index in the ISR group were significantly higher than those in the NISR group at follow-up(P< 0.05). Multivariate logistic regression analysis showed that FIB-4 index at follow-up(OR=3.022,P=0.032) was an independent risk factor for ISR. At follow-up, the area under the FIB-4 index ROC curve was 0.632(95%CI: 0.524-0.740,P=0.024), the diagnostic critical value was 0.474, the sensitivity was 73.3%, and the specificity was 52.7%.Conclusion FIB-4 index is a risk factor for ISR at follow-up after PCI.
-

-
表 1 两组基本资料及术后服用药物比较
Table 1. Comparison of basic data and medications
X±S, M(P25, P75) 项目 NISR组(129例) ISR组(30例) χ2/t/Z P值 年龄/岁 55.86±10.34 59.97±10.98 1.937 0.055 男性/例(%) 105(81.4) 20(66.7) 3.141 0.076 急诊PCI/例(%) 50(38.8) 5(16.7) 5.251 0.022 分次PCI/例(%) 47(36.4) 9(30.0) 0.442 0.506 高血压/例(%) 60(46.5) 17(56.7) 1.005 0.316 糖尿病/例(%) 35(27.1) 11(36.7) 1.076 0.300 术前脑梗死病史/例(%) 7(5.4) 0(0) 1.703 0.192 术后服用药物/例(%) CCB 14(10.9) 5(16.7) 0.782 0.377 ACEI/ARB 66(51.2) 19(63.3) 1.449 0.229 β受体阻滞剂 101(78.3) 24(80.0) 0.042 0.837 随访周期/月 12.53(9.3,13.2) 11.95(6.91,13.01) -1.547 0.122 CCB:钙通道拮抗剂;ACEI/ARB:血管紧张素转换酶抑制剂/血管紧张素受体拮抗剂。 表 2 两组PCI前及随访时检验资料比较
Table 2. Comparison of laboratory data before PCI and follow-up
X±S, M(P25, P75) 项目 NISR组(129例) ISR组(30例) /t/Z P值 PCI前 WBC/(×109·L-1) 9.00±2.93 8.49±2.66 0.874 0.384 PLT/(×109·L-1) 233.67±68.01 230.70±55.10 0.223 0.824 MPV/fL 8.59±1.34 8.64±1.08 -0.215 0.830 eGFR/[mL·min-1·(1.73m2)-1] 94.48±14.58 90.09±20.78 1.362 0.175 ALT/(U·L-1) 31.0(19.0,47.0) 22.5(17.0,43.0) -1.207 0.228 AST/(U·L-1) 41.0(26.0,107.5) 47.0(21.0,96.3) -0.229 0.819 TC/(mmol·L-1) 4.02(3.54,4.91) 3.90(3.38,4.64) -0.720 0.472 TG/(mmol·L-1) 1.60(1.08,2.35) 1.58(1.16,2.21) -0.117 0.907 HDL-C/(mmol·L-1) 0.96±0.22 0.98±0.24 -0.414 0.680 LDL-C/(mmol·L-1) 2.69±0.95 2.72±1.24 -0.154 0.878 FIB-4 0.85(0.40,1.66) 0.88(0.51,1.84) -0.713 0.476 随访时 WBC/(×109·L-1) 6.28±1.71 6.72±2.23 -1.204 0.230 PLT/(×109·L-1) 207.00±49.36 213.30±54.01 -0.611 0.542 MPV/fL 9.20±1.28 9.49±1.96 -1.003 0.317 eGFR/[mL·min-1·(1.73m2)-1] 92.93±14.77 87.78±17.96 1.650 0.101 ALT /(U·L-1) 23.0(17.0,31.5) 19.5(15.0,24.3) 0.114 0.114 AST /(U·L-1) 20.0(17.0.25.0) 16.75(14.0,19.0) 0.628 0.628 TC/(mmol·L-1) 2.92(2.53,3.35) 2.99(2.67,3.65) 0.327 0.327 TG/(mmol·L-1) 1.23(0.95,1.82) 1.36(0.92,1.93) 0.884 0.884 HDL-C/(mmol·L-1) 0.96±0.20 1.05±0.21 -2.583 0.012 LDL-C/(mmol·L-1) 1.57±0.53 1.69±0.67 -1.055 0.293 FIB-4 0.47(0.34,0.70) 0.62(0.45,0.87) -2.252 0.024 表 3 多因素logistic回归分析
Table 3. Multivariate logistic regression analysis
自变量 BE Wald OR 95%CI P值 急诊PCI -1.108 3.732 0.330 1.053~7.173 0.053 随访时HDL-C 1.736 2.920 5.677 0.784~41.698 0.087 随访时FIB-4指数 1.106 4.586 3.022 1.053~7.173 0.032 -
[1] 胡盛寿, 高润霖, 刘力生, 等. 《中国心血管病报告2018》概要[J]. 中国循环杂志, 2019, 34(3): 209-220. doi: 10.3969/j.issn.1000-3614.2019.03.001
[2] Fernando Alfonso, Robert A. Byrne, Fernando Rivero, et al. Current treatment of in-stent restenosis[J]. J Am Coll Cardiol, 2014, 63(24): 2659-2673.
[3] Daichi M, Kazushi S, Takahide I, et al. Fibrosis-4 index reflects right-sided filling pressure in patients with heart failure[J]. Heart Vessels, 2020, 35(3): 376-383. doi: 10.1007/s00380-019-01505-y
[4] Uchenna Agbim, Sumeet K. Asrani. Non-invasive assessment of liver fibrosis and prognosis: an update on serum and elastography markers[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(4): 361-374. doi: 10.1080/17474124.2019.1579641
[5] Qian Chen, Qing Li, Dan Li, et al. Association between liver fibrosis scores and the risk of mortality among patients with coronary artery disease[J]. Atherosclerosis, 2020, 299: 45-52. doi: 10.1016/j.atherosclerosis.2020.03.010
[6] Cao YX, Zhang M, Zhang HW, et al. Impact of liver fibrosis score on prognosis in patients with previous myocardial infarction: A prospective cohort study[J]. Liver Int, 2021, 41(6): 1294-1304. doi: 10.1111/liv.14780
[7] Stefano B, Alessandro M, Enrica B, et al. Liver fibrosis biomarkers accurately exclude advanced fibrosis and are associated with higher cardiovascular risk scores in patients with NAFLD or viral chronic liver disease[J]. Diagnostics(Basel), 2021, 11(1): 111.
[8] Jin JJ, Hui-Wen Zhang, Cao YX, et al. Liver fibrosis scores and coronary atherosclerosis: novel findings in patients with stable coronary artery disease[J]. Hepatol Int, 2021, 15(2): 413-423. doi: 10.1007/s12072-021-10167-w
[9] Liu HH, Cao YX, Jin JL, et al. Liver fibrosis scoring systems as novel tools for predicting cardiovascular outcomes in patients following elective percutaneous coronary intervention[J]. J Am Heart Assoc, 2021, 10(3): e018869. doi: 10.1161/JAHA.120.018869
[10] Kristian T, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. Glob Heart, 2018, 13(4): 305-338. doi: 10.1016/j.gheart.2018.08.004
[11] 韩雅玲. 中国经皮冠状动脉介入治疗指南(2016)[J]. 中华心血管病杂志, 2016, 44(5): 382-400. doi: 10.3760/cma.j.issn.0253-3758.2016.05.006
[12] Davide P, Giuliana C, Dario B, et al. Recurrent in-stent restenosis, certainty of its origin, uncertainty about treatment[J]. Int J Cardiol, 2017, 230: 91-96. doi: 10.1016/j.ijcard.2016.12.073
[13] 吴迪, 张庆军. 中国冠心病诊疗现状和进展[J]. 中国研究型医院, 2020, 7(1): 71-75+192-197. https://www.cnki.com.cn/Article/CJFDTOTAL-YJXU202001020.htm
[14] Helen U, Maximilian O, Thomas M, et al. Coronary in-stent restenosis-predictors and treatment[J]. Dtsch Arztebl Int, 2021, 20: 111.
[15] Jiro A, Kengo T. Mechanisms of drug-eluting stent restenosis[J]. Cardiovasc Interv Ther, 2021, 36(1): 23-29. doi: 10.1007/s12928-020-00734-7
[16] Kenichi F, Satoru O, Wataru Y, et al. Impact of optical coherence tomography-derived neointimal tissue morphology on development of very late in-stent restenosis[J]. Catheter Cardiovasc Interv, 2020, 96(4): E398-E405.
[17] Kazuyuki Y, Frank DK, Fumiyuki O, et al. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis[J]. Nat Rev Cardiol, 2016, 13(2): 79-98. doi: 10.1038/nrcardio.2015.164
[18] Gjin N, Stefan H, Roisin C, et al. Inverse association of alanine aminotransferase within normal range with prognosis in patients with coronary artery disease[J]. Clin Chim Acta, 2019, 496: 55-61. doi: 10.1016/j.cca.2019.06.021
[19] Mitsutaka N, Satoru S, Toru M, et al. Fibrosis-4 index reflects right ventricular function and prognosis in heart failure with preserved ejection fraction[J]. ESC Heart Fail, 2021, 8(3): 2240-2247. doi: 10.1002/ehf2.13317
[20] Qin Z, Zhou K, Li YP, et al. Remnant lipoproteins play an important role of in-stent restenosis in type 2 diabetes undergoing percutaneous coronary intervention: a single-centre observational cohort study[J]. Cardiovasc Diabetol, 2019, 18(1): 11. doi: 10.1186/s12933-019-0819-z
[21] Gupta PK, Jayaram B. Predictor of in-stent restenosis in patients with drug-eluting stent(PRIDE)-a retrospective cohort study[J]. Clin Investig Arterioscler, 2021, 33(4): 184-194.
[22] Kristian T, Joseph SA, Allan S, et al. Third universal definition of myocardial infarction[J]. J Am Coll Cardiol, 2012, 60(16): 1581-1598. doi: 10.1016/j.jacc.2012.08.001
[23] 杨骁翰, 王东兴, 赵慧强, 等. 急性心肌梗死发病昼夜节律及院内结局的探讨[J]. 临床心血管病杂志, 2021, 37(11): 1008-1013. http://lcxb.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=0c7929a2-ccad-4fca-bc50-c222643b1151
[24] Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction[J]. Lancet, 2017, 389(10065): 197-210. doi: 10.1016/S0140-6736(16)30677-8
[25] 徐慧, 刘芳. 单核细胞计数/高密度脂蛋白胆固醇比值与早发冠心病的相关性分析[J]. 临床心血管病杂志, 2020, 36(8): 709-713. http://lcxb.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=0334b654-9fe6-42fc-9d5e-87e4dc3d5643
[26] Karjalainen MK, Holmes MV, Wang Q, et al. Apolipoprotein A-I concentrations and risk of coronary artery disease: A Mendelian randomization study[J]. Atherosclerosis, 2020, 299: 56-63. doi: 10.1016/j.atherosclerosis.2020.02.002
[27] Kjeldsen EW, Nordestgaard LT, Ruth FS. HDL cholesterol and non-cardiovascular disease: a narrative review[J]. Int J Mol Sci, 2021, 22(9): 111.
-




 下载:
下载: