Risk factors of new left bundle branch block after transcatheter aortic valve implantation and its influence on left ventricular function
-
摘要: 目的 探讨经导管主动脉瓣置入术(TAVI)患者新发左束支传导阻滞(new-LBBB)的危险因素及其对左心室功能的影响。方法 回顾性分析郑州大学第一附属医院2019年8月-2020年8月行TAVI的58例重度主动脉瓣狭窄患者资料。根据术后有无持续性new-LBBB,分为new-LBBB组(15例)和对照组(43例)。分析2组患者术前、术中临床资料及术前、术后超声心动图结果的差异。结果 new-LBBB组术前基础QRS波时限、术中置入人工瓣膜尺寸大于对照组,差异均有统计学意义(P < 0.05);术后1年new-LBBB组左心室射血分数(LVEF)低于对照组,左心室舒张末期直径(LVEDD)高于对照组,差异均有统计学意义(P < 0.05)。结论 基础QRS波时限、人工瓣膜尺寸是TAVI后new-LBBB的独立危险因素;TAVI后new-LBBB可能影响患者的LVEF和左心室结构。
-
关键词:
- 经导管主动脉瓣置入术 /
- 新发左束支传导阻滞 /
- 左心室功能 /
- 危险因素
Abstract: Objective To investigate the risk factors of new-LBBB in patients undergoing transcatheter aortic valve implantation (TAVI) and its effect on left ventricular function.Methods The data of 58 patients with severe aortic stenosis who underwent TAVI from August 2019 to August 2020 in the First Affiliated Hospital of Zhengzhou University were analyzed retrospectively. According to postoperative persistence of new-LBBB, they were divided into new-LBBB group (n= 15) and control group (n= 43). Preoperative and intraoperative clinical data and preoperative and postoperative echocardiography results were analyzed.Results The preoperative basic QRS duration and intraoperative prosthetic valve size of the new-LBBB group were larger than those of the control group (P < 0.05).One year after the operation, the left ventricular ejection fraction (LVEF) in the new LBBB group was lower than that in the control group, and the left ventricular end diastolic diameter (LVEDD) was higher than that in the control group (P < 0.05).Conclusion Basic QRS duration and artificial valve size were independent risk factors for new-LBBB after TAVI; New-LBBB after TAVI may affect LVEF and left ventricular structure in patients. -

-
表 1 2组患者临床资料比较
Table 1. Comparison of clinical data
例(%), M(P25, P75), X±S 项目 new-LBBB组(15例) 对照组(43例) χ2/t/Z P 男/女/例 9/6 30/13 0.482 0.533 年龄/岁 77.87(74.18,80.84) 76.33(72.27,79.67) 1.648 0.225 BMI/(kg·m-2) 23.139±3.287 22.979±3.654 0.526 0.695 高血压病 5(33.33) 22(51.16) 1.421 0.233 糖尿病 1(6.67) 11(25.58) 2.425 0.156 冠心病 11(73.33) 25(58.14) 1.090 0.296 AF 4(26.67) 2(4.65) 5.812 0.034 COPD 1(6.67) 3(6.98) 0.002 1.000 脑卒中 3(20.00) 10(23.26) 0.068 1.000 室性心律失常 1(6.67) 3(6.98) 0.002 1.000 基础QRS时限/ms 115.07±12.04 102.88±12.99 0.489 0.004 心率/(次·min-1) 77.53±17.09 73.49±12.88 0.960 0.341 一度AVB 2(13.33) 3(6.98) 0.570 0.596 二叶瓣畸形 1(6.67) 5(11.63) 0.295 1.000 NYHA心功能分级 Ⅱ级 4(26.67) 4(9.30) 2.820 0.185 Ⅲ级 5(33.33) 24(55.81) 2.248 0.230 Ⅳ级 6(40.00) 15(34.89) 0.126 0.723 LVEF/% 54.07±8.44 54.53±10.06 -0.161 0.872 LVEDD/mm 51.67±8.81 51.51±6.86 0.070 0.945 AV Vmax/(m·s-1) 4.52(4.13,4.81) 4.69(4.26,5.11) -2.235 0.066 AVPG-Mean/mmHg 58.32±15.34 69.17±20.63 -2.536 0.023 Edwards/Venus-A/例 1/14 2/41 0.092 1.000 中度及以上瓣周漏 1(6.67) 1(2.33) 0.629 0.454 瓣中瓣 2(13.33) 8(18.60) 0.898 0.327 瓣膜尺寸/mm 28.88±2.53 26.10±2.65 1.852 0.004 Scr/(μmol·L-1) 99.52±66.85 84.34±43.34 1.007 0.318 NT-proBNP/(pg·mL-1) 5071.1(2362.1,9239.8) 4219.6(1562.1,7134.5) 5.548 0.457 表 2 术后1年2组患者超声心动图比较
Table 2. Comparison of echocardiography one year after operation
M(P25, P75), X±S 项目 new-LBBB组(11例) 对照组(40例) t/Z P LVEF/% 56.27±4.15 60.03±4.20 -2.629 0.011 LVEDD/mm 50.55±4.53 46.90±4.01 2.589 0.012 AV Vmax/(m·s-1) 2.23(1.98,2.45) 2.32(2.05,2.67) -0.691 0.492 AVPG-Mean/mmHg 4.13±1.89 3.70±1.77 0.912 0.372 表 3 单因素logistic回归分析
Table 3. Univariate logistic regression analysis
变量 β SE Wald P OR 95%CI AF 2.009 0.93 4.664 0.031 7.455 1.204-46.155 基础QRS波时限 0.073 0.028 6.631 0.010 1.076 1.018-1.138 人工瓣膜尺寸 0.351 0.128 7.562 0.006 1.421 1.106-1.826 表 4 多因素logistic回归分析
Table 4. Multivariate logistic regression analysis
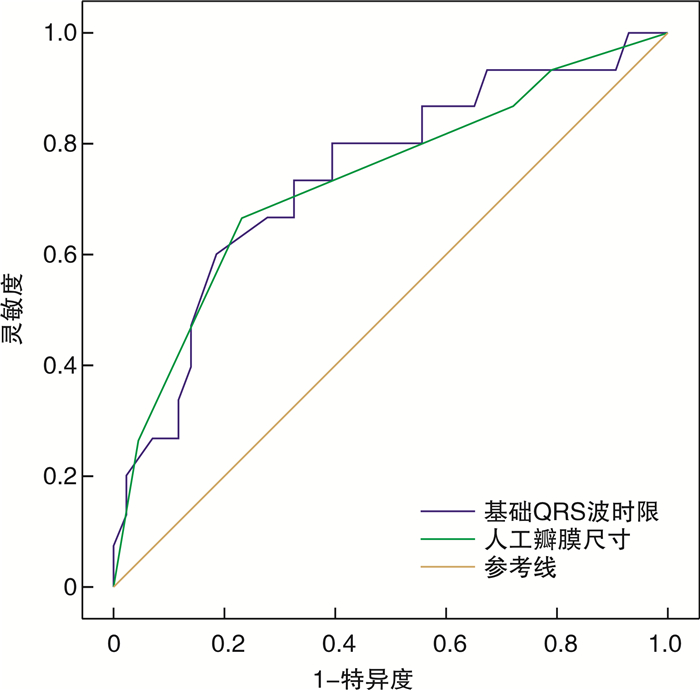
变量 β SE Wald P OR 95%CI 基础QRS波时限 0.072 0.035 4.191 0.041 1.075 1.003-1.151 人工瓣膜尺寸 0.339 0.141 5.771 0.016 1.404 1.064-1.852 表 5 不同预测模型的AUC
Table 5. AUC of different prediction models
变量 AUC(95%CI) 最佳临界值 约登指数 灵敏度 特异度 P 基础QRS时限 0.741(0.590~0.892) 114 ms 0.414 60.00% 81.40% 0.004 人工瓣膜尺寸 0.733(0.575~0.890) 26 mm 0.434 66.67% 76.74% 0.008 -
[1] Chamandi C, Barbanti M, Munoz-Garcia A, et al. Long-Term Outcomes in Patients With New-Onset Persistent Left Bundle Branch Block Following TAVR[J]. JACC Cardiovasc Interv, 2019, 12(12): 1175-1184. doi: 10.1016/j.jcin.2019.03.025
[2] Fadahunsi OO, Olowoyeye A, Ukaigwe A, et al. Incidence, Predictors, and Outcomes of Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement: Analysis From the U.S. Society of Thoracic Surgeons/American College of Cardiology TVT Registry[J]. JACC Cardiovasc Interv, 2016, 9(21): 2189-2199. doi: 10.1016/j.jcin.2016.07.026
[3] Chamandi C, Barbanti M, Munoz-Garcia A, et al. Long-Term Outcomes in Patients With New Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement[J]. JACC Cardiovasc Interv, 2018, 11(3): 301-310. doi: 10.1016/j.jcin.2017.10.032
[4] López-Aguilera J, Segura Saint-Gerons JM, Sánchez Fernández J, et al. Long-term clinical impact of permanent cardiac pacing after transcatheter aortic valve implantation with the CoreValve prosthesis: a single center experience[J]. Europace, 2018, 20(6): 993-1000. doi: 10.1093/europace/eux046
[5] Eschalier R, Massoullié G, Nahli Y, et al. New-Onset Left Bundle Branch Block After TAVI has a Deleterious Impact on Left Ventricular Systolic Function[J]. Can J Cardiol, 2019, 35(10): 1386-1393. doi: 10.1016/j.cjca.2019.05.012
[6] Houthuizen P, Van Garsse LA, Poels TT, et al. Left bundle-branch block induced by transcatheter aortic valve implantation increases risk of death[J]. Circulation, 2012, 126(6): 720-728. doi: 10.1161/CIRCULATIONAHA.112.101055
[7] 王圣, 任培军, 陈现杰, 等. 不同治疗方式对高龄钙化性主动脉瓣重度狭窄患者预后的影响[J]. 临床心血管病杂志, 2019, 35(6): 540-543. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201906012.htm
[8] Panchal HB, Barry N, Bhatheja S, et al. Mortality and major adverse cardiovascular events after transcatheter aortic valve replacement using Edwards valve versus CoreValve: A meta-analysis[J]. Cardiovasc Revasc Med, 2016, 17(1): 24-33. doi: 10.1016/j.carrev.2015.11.005
[9] Zaman S, McCormick L, Gooley R, et al. Incidence and predictors of permanent pacemaker implantation following treatment with the repositionable LotusTM transcatheter aortic valve[J]. Catheter Cardiovasc Interv, 2017, 90(1): 147-154. doi: 10.1002/ccd.26857
[10] 戴晗怡, 朱齐丰, 刘先宝. 经导管主动脉瓣置换术后传导阻滞的研究现状[J]. 华西医学, 2021, 36(09): 1167-1171. https://www.cnki.com.cn/Article/CJFDTOTAL-HXYX202109023.htm
[11] Sammour Y, Krishnaswamy A, Kumar A, et al. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement[J]. JACC Cardiovasc Interv, 2021, 14(2): 115-134. doi: 10.1016/j.jcin.2020.09.063
[12] Auffret V, Puri R, Urena M, et al. Conduction Disturbances After Transcatheter Aortic Valve Replacement: Current Status and Future Perspectives[J]. Circulation, 2017, 136(11): 1049-1069. doi: 10.1161/CIRCULATIONAHA.117.028352
[13] Toutouzas K, Synetos A, Tousoulis D, et al. Predictors for permanent pacemaker implantation after core valve implantation in patients without preexisting ECG conduction disturbances: the role of a new echocardiographic index[J]. Int J Cardiol, 2014, 172(3): 601-603. doi: 10.1016/j.ijcard.2014.01.091
[14] Nazif TM, Williams MR, Hahn RT, et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: analysis of the PARTNER experience[J]. Eur Heart J, 2014, 35(24): 1599-1607. doi: 10.1093/eurheartj/eht376
[15] 焦晓芳, 周微微, 张婷婷, 等. 应用超声新技术评价射血分数保留完全性左束支传导阻滞患者心室功能及同步性[J]. 临床军医杂志, 2021, 49(10): 1141-1143. https://www.cnki.com.cn/Article/CJFDTOTAL-JYGZ202110021.htm
[16] Poulin F, Généreux P, Woo A. Late Cardiac Death in Patients Undergoing Transcatheter Aortic Valve Replacement[J]. J Am Coll Cardiol, 2015, 66(2): 207. doi: 10.1016/j.jacc.2015.03.600
[17] Rodés-Cabau J, Urena M, Nombela-Franco L, et al. Arrhythmic Burden as Determined by Ambulatory Continuous Cardiac Monitoring in Patients With New-Onset Persistent Left Bundle Branch Block Following Transcatheter Aortic Valve Replacement: The MARE Study[J]. JACC Cardiovasc Interv, 2018, 11(15): 1495-1505. doi: 10.1016/j.jcin.2018.04.016
[18] Mathias A, Moss AJ, McNitt S, et al. Clinical Implications of Complete Left-Sided Reverse Remodeling With Cardiac Resynchronization Therapy: A MADIT-CRT Substudy[J]. J Am Coll Cardiol, 2016, 68(12): 1268-1276. doi: 10.1016/j.jacc.2016.06.051
[19] Teng AE, Lustgarten DL, Vijayaraman P, et al. Usefulness of His Bundle Pacing to Achieve Electrical Resynchronization in Patients With Complete Left Bundle Branch Block and the Relation Between Native QRS Axis, Duration, and Normalization[J]. Am J Cardiol, 2016, 118(4): 527-534. doi: 10.1016/j.amjcard.2016.05.049
[20] Jilaihawi H, Zhao Z, Du R, et al. Minimizing permanent pacemakerfollowing repositionable self-expanding transcatheter aortic valvereplacement[J]. JACC Cardiovasc Interv., 2019, 12(18): 1796-1807. doi: 10.1016/j.jcin.2019.05.056
[21] 李光照, 王明蛟, 胡彩娜, 等. 经导管主动脉瓣置换术治疗重度主动脉瓣狭窄的早期临床疗效分析[J]. 临床心血管病杂志, 2020, 36(3): 280-283. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202003019.htm
-




 下载:
下载: