Construction and validation of a nomogram prediction model for the risk of coronary heart disease in elderly postmenopausal women
-
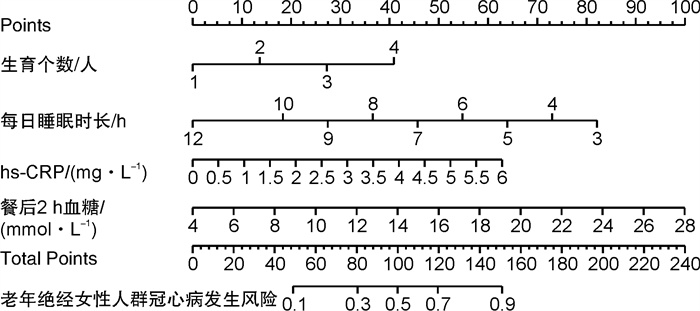
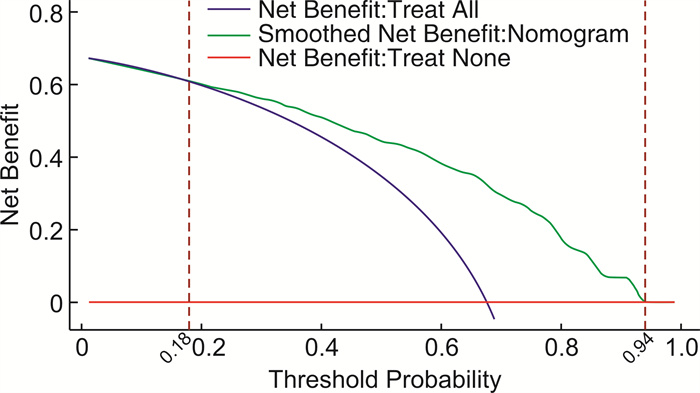
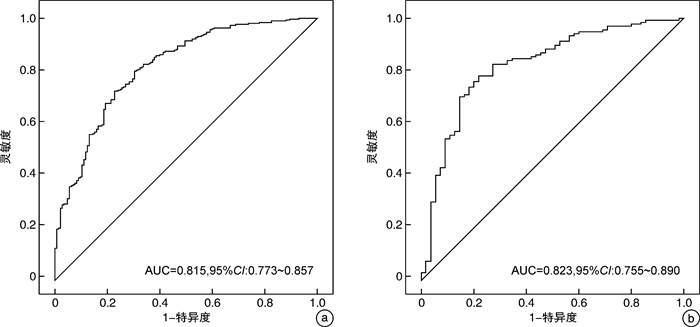
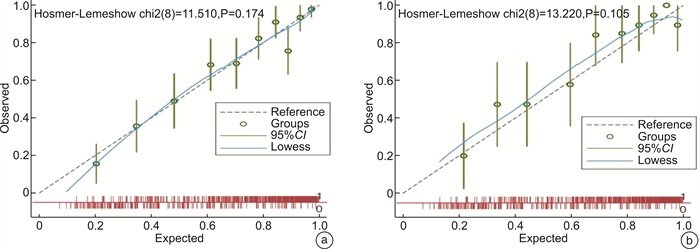
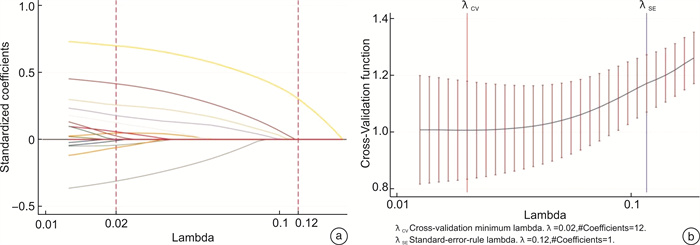
摘要: 目的 构建老年绝经女性人群发生冠心病(CHD)的预测模型,并对列线图的预测效率进行验证。方法 回顾性分析2018年3月—2019年2月在安徽省某三级甲等医院心内科就诊并接受冠状动脉(冠脉)造影的639例老年绝经女性的临床资料,根据冠脉造影结果将其分为CHD组(439例)和对照组(200例),同时将研究对象依据7∶3的比例随机分为建模组(447例)和验证组(192例)。在建模组人群中采用多因素回归分析筛选出老年绝经女性人群发生CHD的独立影响因素、构建个性化的列线图模型,并在验证组人群中对模型的预测效率和适用性进行外部验证。结果 建模组人群的多因素logistic回归分析结果表明,每日睡眠时长(OR=0.674,95%CI:0.546~0.833)是老年绝经女性人群发生CHD的独立保护因素(P< 0.05),而生育个数(OR=1.798,95%CI:1.391~2.325)、超敏C反应蛋白水平(OR=1.572,95%CI:1.381~1.789)及餐后2 h血糖(OR=1.197,95%CI:1.097~1.305)为老年绝经女性人群发生CHD的独立危险因素(P< 0.05)。利用上述指标构建列线图预测模型,列线图模型的ROC曲线下面积在建模组及验证中分别为0.815(95%CI:0.773~0.857)、0.823(95%CI:0.755~0.890),建模组及验证组人群中的校准曲线均提示列线图的预测概率与实际发生频率之间具有较好的一致性。临床决策分析曲线提示,当老年绝经女性人群发生CHD的阈值概率处于0.18~0.94时,采用列线图的临床净获益水平最高。结论 老年绝经女性人群发生CHD的列线图预测模型预测能力和适用能力较好,可用于筛查此类人群的CHD发生风险。Abstract: Objective To construct a prediction model for coronary heart disease(CHD) in elderly postmenopausal women, and to verify the prediction efficiency of nomogram.Methods There were 639 elderly postmenopausal women who received coronary angiography retrospectively in this study. According to the results of coronary angiography, they were divided into CHD group(439 cases) and control group(200 cases), and the subjects were randomly divided into modeling group(447 cases) and validation group(192 cases) according to the split ratio of 7∶3. Multivariate regression analysis was used in the modeling group to screen out the independent influencing factors of CHD, and a personalized nomogram model was constructed, and the prediction efficiency and applicability of the model were externally verified in the validation group.Results The multivariate logistic regression analysis of the modeling group showed that daily sleep duration(OR=0.674, 95%CI: 0.546-0.833) was an independent protective factor for the occurrence of CHD in elderly menopausal women(P< 0.05), while Number of children born(OR=1.798, 95%CI: 1.391-2.325), level of high-sensitivity C-reactive protein(OR=1.572, 95%CI: 1.381-1.789) and 2-h postprandial blood glucose(OR=1.197, 95%CI: 1.097-1.305) were independent risk factors for CHD in elderly postmenopausal women(P< 0.05). Using the above indicators to build a nomogram prediction model, the area under the ROC curve of the nomogram model was 0.815(95%CI: 0.773-0.857) and 0.823(95%CI: 0.755-0.890) in the modeling group and the validation group, respectively. The calibration curves in both the modeling group and the validation group indicated that the predicted probability of the nomogram was in good agreement with the actual frequency of occurrence. The clinical decision analysis curve suggests that when the threshold probability of coronary heart disease in elderly postmenopausal women is between 0.18 and 0.94, the level of net clinical benefit of using nomogram is the highest.Conclusion The nomogram prediction model of CHD in elderly postmenopausal women has good predictive ability and applicability, and can be used to screen the risk of CHD in this population.
-
Key words:
- elderly menopausal women /
- coronary heart disease /
- risk factors /
- prediction model
-

-
表 1 建模组及验证组临床资料比较
Table 1. General data
例(%), M(P25, P75), X±S 项目 总计(639例) 建模组(447例) 验证组(192例) 统计量 P 冠心病 439(68.70) 302(67.56) 137(71.35) 0.898 0.343 文化程度 1.522 0.467 初中及以下 556(87.01) 393(87.92) 163(84.90) 高中及中专 58(9.08) 39(8.72) 19(9.90) 大专及以上 25(3.91) 15(3.36) 10(5.21) 生育个数 0.915 0.822 1人 112(17.53) 78(17.45) 34(17.71) 2人 294(46.01) 205(45.86) 89(46.35) 3人 109(17.06) 80(17.90) 29(15.10) 4人 124(19.41) 84(18.79) 40(20.83) 吸烟 2(0.31) 0(0) 2(1.04) - 0.090 饮酒 1(0.16) 1(0.22) 0(0) - 1.000 家族史 4(0.63) 3(0.67) 1(0.52) 0.049 0.825 脑血管病史 136(21.28) 95(21.25) 41(21.35) 0.001 0.977 高血压 447(69.95) 308(68.90) 139(72.40) 0.779 0.377 糖尿病 193(30.20) 136(30.43) 57(29.69) 0.035 0.852 高脂血症 197(30.83) 138(30.87) 59(30.73) 0.001 0.971 TSH/(μIU·mL-1) 2.42(1.54,3.83) 2.47(1.58,3.83) 2.29(1.50,3.84) 0.755 0.450 FT4/(ng·dL-1) 12.67(11.50,13.91) 12.78(11.51,13.98) 12.51(11.50,13.81) 0.810 0.418 FT3/(pg·mL-1) 4.50(4.00,4.97) 4.50(4.01,4.97) 4.50(3.96,5.01) -0.364 0.716 VLDL-C/(mmol·L-1) 1.06(0.87,1.31) 1.06(0.88,1.32) 1.05(0.85,1.29) 0.638 0.524 LDL-C/(mmol·L-1) 2.21(1.72,2.70) 2.20(1.70,2.64) 2.23(1.75,2.85) -1.037 0.300 HDL-C/(mmol·L-1) 1.01(0.87,1.19) 1.03(0.89,1.19) 0.98(0.83,1.19) 1.928 0.054 TG/(mmol·L-1) 1.50(1.14,2.02) 1.48(1.15,1.99) 1.54(1.14,2.02) -0.751 0.453 TC/(mmol·L-1) 4.31(3.67,5.02) 4.31(3.66,4.99) 4.34(3.69,5.06) -0.686 0.493 HbA1c/% 6.00(5.70,6.80) 6.00(5.70,6.73) 6.00(5.60,7.10) -0.203 0.839 餐后2h血糖/(mmol·L-1) 7.90(7.00,10.84) 7.90(7.07,10.59) 7.80(6.88,11.49) 0.350 0.726 空腹血糖/(mmol·L-1) 5.21(4.67,6.12) 5.19(4.67,6.09) 5.22(4.66,6.34) -0.024 0.981 随机血糖/(mmol·L-1) 6.73(5.46,9.04) 6.78(5.44,9.00) 6.59(5.50,9.40) -0.026 0.979 血钙/(mmol·L-1) 2.20(2.11,2.31) 2.20(2.11,2.30) 2.20(2.12,2.32) -0.066 0.948 血氯/(mmol·L-1) 106.00(104.00,108.00) 106.00(104.00,108.00) 106.00(104.00,108.00) -0.846 0.395 血钠/(mmol·L-1) 141.00(139.00,142.00) 141.00(139.00,142.00) 141.00(139.00,142.00) -0.907 0.361 血钾/(mmol·L-1) 3.83(3.60,4.08) 3.83(3.61,4.07) 3.81(3.59,4.08) 0.452 0.651 血CO2/mmHg 24.49±3.04 24.48±3.11 24.52±2.87 -0.166 0.868 胱抑素/(mg·L-1) 0.91(0.80,1.09) 0.92(0.81,1.09) 0.90(0.78,1.08) 1.457 0.145 尿酸/(μmol·L-1) 305.00(250.00,367.00) 302.00(252.00,368.00) 312.00(246.00,364.00) 0.291 0.771 肌酐/(μmol·L-1) 62.00(53.00,76.00) 61.50(52.00,76.00) 62.00(54.00,75.00) -0.393 0.695 尿素氮/(mmol·L-1) 6.32(5.14,8.00) 6.34(5.11,8.01) 6.29(5.20,7.90) 0.528 0.598 GLO/(g·L-1) 25.40(22.80,28.90) 25.40(22.90,28.70) 25.50(22.70,29.00) -0.142 0.888 ALB/(g·L-1) 43.60(40.60,45.90) 43.70(40.60,46.20) 43.20(40.30,45.50) 1.496 0.135 TP/(g·L-1) 69.00(65.00,72.90) 69.00(65.00,73.00) 69.00(65.00,72.60) 0.799 0.425 间接胆红素/(μmol·L-1) 6.30(4.60,8.70) 6.20(4.60,8.50) 6.40(4.90,8.90) -0.872 0.383 直接胆红素/(μmol·L-1) 2.90(2.10,4.00) 2.80(2.10,3.80) 3.00(2.20,4.30) -1.248 0.212 TBIL/(μmol·L-1) 9.30(7.00,12.60) 9.10(6.90,12.50) 9.50(7.30,13.10) -1.002 0.316 AST/(U·L-1) 20.00(16.00,27.00) 20.00(16.00,27.00) 20.00(17.00,25.00) 0.616 0.538 ALT/(U·L-1) 17.00(13.00,24.00) 17.00(13.00,25.00) 18.00(14.00,23.00) -0.303 0.762 hs-CRP/(mg·L-1) 2.80(1.03,5.00) 2.86(0.98,5.00) 2.70(1.10,5.00) 0.519 0.597 PLT/(×109·L-1) 193.00(156.00,227.00) 191.00(155.00,227.00) 197.00(162.00,227.00) -0.829 0.407 Hb/(g·L-1) 120.00(111.00,127.00) 120.00(111.00,128.00) 120.00(111.00,126.00) 0.311 0.756 RBC/(×1012·L-1) 3.90(3.65,4.19) 3.92(3.66,4.19) 3.87(3.65,4.18) 0.550 0.583 NLR 2.20(1.64,2.95) 2.23(1.64,3.00) 2.10(1.65,2.74) 1.205 0.228 白细胞/(×109·L-1) 6.13(5.21,7.53) 6.07(5.21,7.37) 6.24(5.25,7.74) -1.188 0.235 脉压差/mmHg 58.00(48.00,68.00) 58.00(49.00,69.00) 55.00(47.00,66.00) 1.831 0.067 舒张压/mmHg 76.00(70.00,84.00) 76.00(69.00,83.00) 76.00(70.00,85.00) -1.291 0.196 收缩压/mmHg 135.00(124.00,146.00) 136.00(125.00,145.00) 134.00(123.00,146.00) 0.434 0.664 心率/(次·min-1) 72.00(67.00,80.00) 72.00(68.00,79.00) 74.00(66.00,80.00) -0.612 0.540 每日睡眠时长/h 6.00(6.00,7.00) 6.00(6.00,7.00) 6.00(6.00,7.00) 0.991 0.297 BMI/(kg·m-2) 24.49(22.67,26.67) 24.61(22.89,26.67) 24.34(22.60,26.64) 1.061 0.289 年龄/岁 68.00(65.00,74.00) 69.00(65.00,74.00) 68.00(64.00,74.00) 0.806 0.420 表 2 建模组人群CHD发生的单因素分析结果
Table 2. Univariate analysis results of CHD in the modeling group
例(%), M(P25, P75), X±S 项目 总计(447例) 未发生CHD(145例) 发生CHD(302例) 统计量 P 文化程度 8.996 0.011 初中及以下 393(87.92) 119(82.07) 274(90.73) 高中及中专 39(8.72) 21(14.48) 18(5.96) 大专及以上 15(3.36) 5(3.45) 10(3.31) 生育个数 39.360 < 0.001 1人 78(17.45) 37(25.52) 41(13.58) 2人 205(45.86) 84(57.93) 121(40.07) 3人 80(17.90) 9(6.21) 71(23.51) 4人 84(18.79) 15(10.34) 69(22.85) 吸烟 0(0) 0(0) 0(0) - 1.000 饮酒 1(0.22) 0(0) 1(0.33) - 1.000 家族史 3(0.67) 1(0.69) 2(0.66) 0.001 0.973 脑血管病史 95(21.25) 23(15.86) 72(23.84) 3.727 0.054 高血压 308(68.90) 90(62.07) 218(72.19) 4.679a 0.031 糖尿病 136(30.43) 22(15.17) 114(37.75) 23.587 < 0.001 高脂血症 138(30.87) 40(27.59) 98(32.45) 1.086 0.297 TSH/(μIU·mL-1) 2.47(1.58,3.83) 2.53(1.50,4.04) 2.46(1.62,3.65) 0.290 0.772 FT4/(ng·dL-1) 12.78(11.51,13.98) 12.83(11.70,14.04) 12.66(11.41,13.94) 0.522 0.602 FT3/(pg·mL-1) 4.50(4.01,4.97) 4.54(4.09,5.06) 4.48(3.99,4.86) 1.501 0.133 VLDL-C/(mmol·L-1) 1.06(0.88,1.32) 1.05(0.87,1.30) 1.07(0.88,1.33) -1.053 0.292 LDL-C/(mmol·L-1) 2.20(1.70,2.64) 2.24(1.60,2.71) 2.19(1.75,2.62) 0.192 0.848 HDL-C/(mmol·L-1) 1.03(0.89,1.19) 1.07(0.93,1.22) 1.01(0.87,1.17) 2.453 0.014 TG/(mmol·L-1) 1.48(1.15,1.99) 1.35(0.97,1.76) 1.57(1.18,2.11) -3.317 < 0.001 TC/(mmol·L-1) 4.31(3.66,4.99) 4.32(3.54,5.18) 4.30(3.71,4.90) 0.167 0.868 HbA1c/% 6.00(5.70,6.73) 5.80(5.50,6.20) 6.20(5.80,7.10) -6.619 < 0.001 餐后2h血糖/(mmol·L-1) 7.90(7.07,10.59) 7.24(6.80,8.35) 8.60(7.60,12.13) -6.736 < 0.001 空腹血糖/(mmol·L-1) 5.19(4.67,6.09) 5.06(4.60,5.61) 5.31(4.69,6.33) -2.679 0.007 随机血糖/(mmol·L-1) 6.78(5.44,9.00) 6.35(5.33,7.89) 6.97(5.48,9.52) -2.504 0.012 血钙/(mmol·L-1) 2.20(2.11,2.30) 2.21(2.12,2.33) 2.20(2.10,2.30) 1.096 0.273 血氯/(mmol·L-1) 106.00(104.00,108.00) 106.00(104.00,108.00) 106.00(103.00,108.00) 0.797 0.423 血钠/(mmol·L-1) 141.00(139.00,142.00) 141.00(140.00,142.00) 141.00(139.00,142.00) 2.375 0.017 血钾/(mmol·L-1) 3.83(3.61,4.07) 3.80(3.54,4.04) 3.86(3.64,4.10) -1.595 0.111 血CO2/mmHg 24.48±3.11 24.64±3.19 24.40±3.07 0.778 0.437 胱抑素/(mg·L-1) 0.92(0.81,1.09) 0.89(0.79,1.03) 0.94(0.82,1.12) -1.980 0.048 尿酸/(μmol·L-1) 302.00(252.00,368.00) 299.00(243.00,363.00) 310.00(256.00,373.00) -1.125 0.261 肌酐/(μmol·L-1) 61.50(52.00,76.00) 60.00(53.00,74.00) 62.00(52.00,76.00) -0.617 0.537 尿素氮/(mmol·L-1) 6.34(5.11,8.01) 6.39(5.16,7.81) 6.30(5.09,8.15) 0.016 0.988 GLO/(g·L-1) 25.40(22.90,28.70) 25.60(22.20,28.90) 25.30(23.00,28.60) -0.604 0.546 ALB/(g·L-1) 43.70(40.60,46.20) 44.80(41.10,46.50) 43.30(40.50,45.90) 2.013 0.044 TP/(g·L-1) 69.15±6.05 69.39±6.13 69.04±6.00 0.574 0.566 间接胆红素/(μmol·L-1) 6.20(4.60,8.50) 6.40(4.60,9.20) 6.20(4.50,8.30) 1.095 0.274 直接胆红素/(μmol·L-1) 2.80(2.10,3.80) 2.70(2.00,4.00) 2.90(2.10,3.80) -0.132 0.895 TBIL/(μmol·L-1) 9.10(6.90,12.50) 9.10(6.70,14.00) 9.10(6.90,11.90) 0.488 0.626 AST/(U·L-1) 20.00(16.00,27.00) 20.00(16.00,26.00) 20.00(17.00,28.00) -0.840 0.401 ALT/(U·L-1) 17.00(13.00,25.00) 17.00(12.00,22.00) 17.00(13.00,28.00) -1.177 0.239 hs-CRP/(mg·L-1) 2.86(0.98,5.00) 1.03(0.45,3.20) 4.15(1.76,5.00) -8.173 < 0.001 PLT/(×109·L-1) 191.00(155.00,227.00) 176.00(148.00,209.00) 196.00(162.00,237.00) -3.857 < 0.001 Hb/(g·L-1) 120.00(111.00,128.00) 121.00(115.00,129.00) 119.00(110.00,126.00) 2.125 0.034 RBC/(×1012·L-1) 3.92(3.66,4.19) 3.96(3.72,4.20) 3.89(3.61,4.19) 1.490 0.136 NLR 2.23(1.64,3.00) 2.03(1.53,2.75) 2.32(1.72,3.21) -3.096 0.002 白细胞计数/(×109·L-1) 6.07(5.21,7.37) 5.90(4.92,6.85) 6.13(5.35,7.69) -2.809 0.005 脉压差/mmHg 58.84±14.68 58.01±15.08 59.24±14.47 -0.829 0.408 舒张压/mmHg 76.00(69.00,83.00) 78.00(70.00,86.00) 75.00(68.00,82.00) 2.167 0.030 收缩压/mmHg 136.00(125.00,145.00) 135.00(125.00,146.00) 136.00(125.00,145.00) 0.345 0.730 心率/(次·min-1) 72.00(68.00,79.00) 73.00(68.00,80.00) 72.00(67.00,79.00) 0.611 0.541 每日睡眠时长/h 6.00(6.00,7.00) 7.00(6.00,8.00) 6.00(6.00,7.00) 4.430 < 0.001 BMI/(kg·m-2) 24.61(22.89,26.67) 25.00(22.67,26.71) 24.44(22.89,26.67) 0.786 0.432 年龄/岁 69.00(65.00,74.00) 68.00(64.00,73.00) 69.00(65.00,75.00) -1.985 0.047 表 3 Logistic回归分析老年绝经女性发生CHD的影响因素
Table 3. Logistic regression analyzed the influencing factors of CHD in elderly postmenopausal women
变量 偏回归系数 标准误 Z P OR OR的95%CI 常量 -0.885 0.823 -1.080 0.282 0.413 0.082~2.071 生育个数 0.587 0.131 4.470 < 0.001 1.798 1.391~2.325 每日睡眠时长 -0.394 0.108 -3.660 < 0.001 0.674 0.546~0.833 hs-CRP 0.452 0.066 6.850 < 0.001 1.572 1.381~1.789 餐后2 h血糖 0.180 0.044 4.060 < 0.001 1.197 1.097~1.305 -
[1] Zhang Y, Pletcher MJ, Vittinghoff E, et al. Association between cumulative low-density lipoprotein cholesterol exposure during young adulthood and middle age and risk of cardiovascular events[J]. JAMA Cardiol, 2021, 6(12): 1406-1413. doi: 10.1001/jamacardio.2021.3508
[2] 刘新防, 苏怀勇. 老年绝经女性冠心病危险因素与预防保健思路研究现状[J]. 双足与保健, 2018, 27(13): 195-196.
[3] Akyea RK, Kontopantelis E, Kai J, et al. Sex disparity in subsequent outcomes in survivors of coronary heart disease[J]. Heart, 2022, 108(1): 37-45. doi: 10.1136/heartjnl-2021-319566
[4] Khamis RY, Ammari T, Mikhail GW. Gender differences in coronary heart disease[J]. Heart, 2016, 102(14): 1142-1149. doi: 10.1136/heartjnl-2014-306463
[5] 郭福佳, 袁正强, 施尚鹏, 等. 早发与晚发冠心病患者临床及冠状动脉病变特点的性别差异分析[J]. 临床心血管病杂志, 2021, 37(1): 28-31. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202101006.htm
[6] 骆燕萍, 俞艳烨, 邹茜. 绝经前后冠心病患者临床特点雌激素及冠状动脉病变特征分析[J]. 中国妇幼保健, 2021, 36(20): 4846-4848. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202120065.htm
[7] 白茹, 戴思燕, 汤彩虹. 围绝经期老年绝经女性冠心病发病率调查和影响因素分析[J]. 中国妇幼保健, 2021, 36(17): 4098-4102. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202117063.htm
[8] 党爱民. 老年绝经女性心血管疾病特征与研究现状[J]. 中华老年心脑血管病杂志, 2021, 23(6): 561-563. doi: 10.3969/j.issn.1009-0126.2021.06.001
[9] 廖丽萍, 周跟东, 张晓红, 等. 淋巴单核细胞比值与老年绝经后女性冠心病的相关性分析[J]. 中华老年心脑血管病杂志, 2021, 23(11): 1158-1161. doi: 10.3969/j.issn.1009-0126.2021.11.010
[10] 吴琪. 建立基于生化指标的冠心病风险预测模型[D]. 杭州师范大学, 2019.
[11] Cho KI, Shin ES, Ann SH, et al. Gender differences in risk factors and clinical outcomes in young patients with acute myocardial infarction[J]. J Epidemiol Community Health, 2016, 70(11): 1057-1064. doi: 10.1136/jech-2015-207023
[12] 雷梅先, 蔡霜婷. 围绝经期女性性激素与血管内皮功能及冠心病的相关性研究[J]. 临床内科杂志, 2021, 38(9): 594-597. doi: 10.3969/j.issn.1001-9057.2021.09.006
[13] 叶青. 老年绝经女性冠心病相关的危险因素及其与冠状动脉病变严重程度的相关性研究[D]. 安徽医科大学, 2020.
[14] 李玲慧, 李娜. 2018~2019年3月天津市部分体检老年人群睡眠时长与冠心病的相关性研究[J]. 预防医学论坛, 2019, 25(9): 678-682. https://www.cnki.com.cn/Article/CJFDTOTAL-YXWX201909010.htm
[15] Weber C, Fangauf SV, Michal M, et al. Cortisol awakening reaction and anxiety in depressed coronary artery disease patients[J]. J Clin Med, 2022, 11(2): 100.
[16] 李菁, 郑金刚. 女性冠心病危险因素分析[J]. 心血管病学进展, 2012, 33(1): 31-35. doi: 10.3969/j.issn.1004-3934.2012.01.010
[17] Kloster S, Tolstrup JS, Nielsen DG, et al. Long-term cardiovascular health after pregnancy in danish women with congenital heart disease. a register-based cohort study between 1993 and 2016[J]. J Am Heart Assoc, 2022, 11(5): e023588. doi: 10.1161/JAHA.121.023588
[18] 陆士娟, 钟江华, 吴淼, 等. 血浆网膜素-1及超敏C反应蛋白水平与冠心病发生与发展的关系[J]. 医疗装备, 2021, 34(15): 3-5. doi: 10.3969/j.issn.1002-2376.2021.15.002
[19] Jiang J, Zhao L, Lin L, et al. Postprandial blood glucose outweighs fasting blood glucose and HbA1c in screening coronary heart disease[J]. Sci Rep, 2017, 7(1): 14212. doi: 10.1038/s41598-017-14152-y
[20] 花宇, 郭潇繁. 血糖控制水平对冠心病合并糖尿病患者经皮冠状动脉介入治疗预后的影响[J]. 中国卫生工程学, 2020, 19(6): 926-927+932. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWX202006046.htm
[21] Dong Y, Que L, Jia Q, et al. Predicting reintervention after thoracic endovascular aortic repair of Stanford type B aortic dissection using machine learning[J]. Eur Radiol, 2022, 32(1): 355-367. doi: 10.1007/s00330-021-07849-2
[22] Kong S, Chen C, Zheng G, et al. A prognostic nomogram for long-term major adverse cardiovascular events in patients with acute coronary syndrome after percutaneous coronary intervention[J]. BMC Cardiovasc Disord, 2021, 21(1): 253. doi: 10.1186/s12872-021-02051-0
[23] Zhang Q, Zhang J, Lei L, et al. Nomogram to predict risk of incident chronic kidney disease in high-risk population of cardiovascular disease in China: community-based cohort study[J]. BMJ Open, 2021, 11(11): e047774. doi: 10.1136/bmjopen-2020-047774
[24] 周晓娟, 马礼坤, 魏艳, 等. 急性心肌梗死患者院内心源性休克风险列线图预测模型的构建[J]. 临床心血管病杂志, 2021, 37(5): 421-427. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202105007.htm
[25] 白扬, 李晓红, 任素剑, 等. 冠心病、抑郁症与慢性应激[J]. 湖北中医药大学学报, 2019, 21(2): 54-57. doi: 10.3969/j.issn.1008-987X.2019.02.013
[26] 霍翾, 吕茂玲, 刘莎莎, 等. 新疆地区LIPG和GUCY1A3基因多态性与冠心病的相关性研究[J]. 临床心血管病杂志, 2021, 37(6): 576-580. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202106017.htm
-




 下载:
下载: