Two-dimensional speckle tracking imaging evaluates right ventricular systolic function and synchrony in the early stage of left bundle branch pacing
-
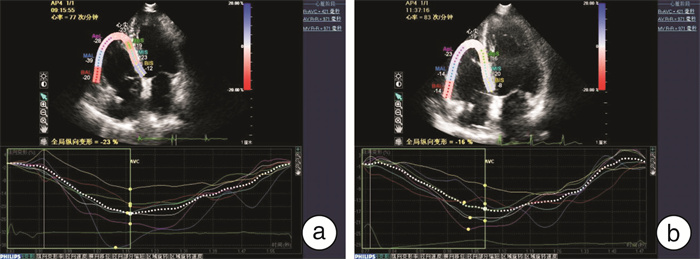
摘要: 目的 运用二维斑点追踪(2D-STI)技术对左束支区域起搏(LBBP)术后早期右心室收缩功能及同步性进行评价。方法 选取2020年8月—2021年1月于成都市第三人民医院心内科成功实施LBBP及右室流出道起搏(RVOP)的患者各23例。所有患者均于术后2周内行超声心动图检查。应用2D-STI技术分析和获取2组患者右心室整体、侧壁及室间隔纵向应变(LS)及相应的纵向应变达峰时间标准差(SD-Ts)。比较2组患者手术前后的常规参数及2D-STI参数。结果 ① RVOP组术后QRS时限明显增宽,且术后QRS时限RVOP组较LBBP组明显增宽(P< 0.001)。其余各常规指标在两组间差异均无统计学意义(P>0.05)。②LBBP组术后,右心室SD-Ts、间隔SD-Ts、侧壁SD-Ts均减小,且术后LBBP组右心室SD-Ts、侧壁SD-Ts较RVOP组亦明显减小,差异均有统计学意义(P< 0.05)。手术前、后右心室各应变指标在两组间差异均无统计学意义(P>0.05)。结论 2D-STI技术可客观、精确地评价不同部位起搏术后右心室收缩功能及同步性。LBBP作为一种全新的生理性起搏方式,能有效地维持右心室收缩同步性。Abstract: Objective To evaluate early right ventricular systolic function and synchronicity of left bundle branch pacing using two-dimensional speckle tracking imaging(2D-STI).Methods Forty six patients who received permanent cardiac implantation were enrolled from August 2020 to January 2021 in The Third People's Hospital of Chengdu. Patients were divided into left bundle branch pacing(LBBP) group(n=23) and right ventricular outflow tract pacing(RVOP) group(n=23). Echocardiography was performed at two weeks after surgery. The global longitudinal strain(GLS) and standard deviation of the time to peak strain(SD-Ts) of RV, the longitudinal strain(LS) and SD-Ts of lateral wall and ventricular septum were analyzed and obtained using 2D-STI. General and 2D STI parameters were compared between the two groups before and after operation.Results (1) The QRS wave duration was significantly longer in RVOP group after operation and was also significantly longer than in LBBP group(P< 0.001). No significant differences were detected in the rest parameters(P>0.05). (2) The SD-Ts of RV, ventricular septum and lateral wall were decreased in LBBP group after operation(P< 0.05). Compared with RVOP group, the SD-Ts of RV and lateral wall were also decreased in LBBP group after operation(P< 0.05). There were no differences of the strain index between two groups before and after operation(P>0.05)Conclusion 2D-STI is an objective and accurate method to evaluate RV global systolic function and synchrony.
-

-
表 1 两组一般临床资料比较
Table 1. General data
X±S 项目 LBBP组(23例) RVOP组(23例) 年龄/岁 66.60±11.86 70.60±9.43 心率/(次·min-1) 69.78±6.76 67.47±8.60 男性/例(%) 9(39.1) 13(56.5) 病因/例(%) 高度房室传导阻滞 9(39.1) 11(47.8) 三度房室传导阻滞 14(60.9) 12(52.2) 合并症/例(%) 高血压 15(65.2) 18(78.3) 糖尿病 12(52.2) 10(43.5) 术前QRS波时限/ms 120.39±23.99 121.30±23.19 术后QRS波时限/ms 113.04±11.13 146.04±12.421)2) RVOP组术后与术前比较,1)P < 0.001;LBBP组与RVOP组术后比较,2)P < 0.001。 表 2 两组常规超声心动图参数比较
Table 2. Conventional echocardiographic parameters
X±S 指标 LBBP组 RVOP组 术前 术后 术前 术后 RVD1/mm 53.47±5.89 51.39±7.24 52.38±5.98 54.17±6.65 RVD2/mm 35.68±4.67 37.52±3.99 34.89±5.23 36.69±3.88 RVD3/mm 31.53±3.94 29.95±5.80 30.25±3.38 29.08±4.08 FAC/% 50.05±4.28 51.25±6.08 48.23±5.59 48.15±6.20 S′/(cm·s-1) 12.38±2.61 11.98±1.85 13.02±1.69 11.47±1.13 TAPSE 19.20±3.78 18.71±2.52 21.06±4.23 19.39±3.05 LVEF/% 62.38±3.42 59.74±4.49 61.58±4.67 60.82±4.43 E/A 0.97±0.26 0.81±0.35 0.89±0.43 0.93±0.36 表 3 两组手术前后右心室收缩功能比较
Table 3. Right ventricular systolic function
X±S 指标 LBBP组 RVOP组 术前 术后 术前 术后 GLS/% -20.71±5.41 -21.48±5.46 -20.65±4.62 -19.47±4.39 SLS/% -17.79±4.66 -18.89±5.40 -17.00±4.17 -15.97±4.32 LLS/% -23.20±6.43 -24.60±6.31 -24.15±5.68 -22.98±5.81 表 4 两组手术前后右心室收缩同步性比较
Table 4. Right ventricular systolic synchrony
X±S, M(P25, P75) 指标 LBBP组 RVOP组 术前 术后 术前 术后 RV SD-Ts/ms 53.75±23.75 34.71±24.031)2) 48.83±25.84 56.69±27.88 S SD-Ts/ms 31.37(23.09, 43.46) 20.75(11.95, 36.30)1) 35.43(10.32, 59.39) 40.84(16.39, 74.48) L SD-Ts/ms 34.95(23.48, 73.57) 22.53(7.84, 59.87)1)2) 34.67(20.34, 58.98) 46.58(25.48, 68.39) 与本组术前比较,1)P < 0.05;与RVOP组术后比较,2)P < 0.05。 -
[1] Huang W, Su L, Wu S, et al. A novel pacing strategy with low and stable output: pacing the left bundle branch immediately beyond the conduction block[J]. Can J Cardiol, 2017, 33(12): 1736. e1-1736. e3. doi: 10.1016/j.cjca.2017.09.013
[2] Huang W, Wu S, Vijayaraman P, et al. Cardiac resynchronization therapy in patients with nonischemic cardiomyopathy using left bundle branch pacing[J]. JACC Clinical Electrophysiology, 2020, 6(7): 849-858. doi: 10.1016/j.jacep.2020.04.011
[3] 贾祥贺, 郑晓琳, 卢文杰, 等. 希氏束起搏与右心室间隔部起搏的临床对比研究[J]. 临床心血管病杂志, 2021, 37(4): 375-378. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202104017.htm
[4] Wu S, Su L, Vijayaraman P, et al. Left bundle branch pacing for cardiac resynchronization therapy: nonrandomized on-treatment comparison with his bundle pacing and biventricular pacing[J]. Canadian J Cardiol, 2020, 20: 111.
[5] Apostolakis S, Konstantinides S. The right ventricle in health and disease: Insights into physiology, pathophysiology and diagnostic management[J]. Cardiologym, 2012, 121: 263-273. doi: 10.1159/000338705
[6] Muraru D, Onciul S, Peluso D, et al. Sex-and method-specific reference values for right ventricular strain by 2-Dimensional speckle-tracking echocardiography[J]. Circ Cardiovasc Imaging, 2016, 9: e003866.
[7] Cameli M, Righini FM, Lisi M, et al. Right ventricular strain as a novel approach to analyze right ventricular performance in patients with heart failure[J]. Heart Failure Reviews, 2014, 19(5): 603-610. doi: 10.1007/s10741-013-9414-7
[8] Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay[J]. J Am Coll Cardiol, 2019, 74(7): e51-e156. doi: 10.1016/j.jacc.2018.10.044
[9] Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging[J]. J Am Soc Echocardiogr, 2015, 28(1): 1-39. doi: 10.1016/j.echo.2014.10.003
[10] Haddad F, Hunt SA, Rosenthal DN, et al. Right ventricular function in cardiovascular disease, part i: anatomy, physiology, aging, and functional assessment of the right ventricle[J]. Circulation, 2008, 117(11): 1436-1448. doi: 10.1161/CIRCULATIONAHA.107.653576
[11] 苏蓝, 黄伟剑. 永久性希浦系起搏——同步化治疗的新方向[J]. 南京医科大学学报, 2019, 39(6): 802-805. https://www.cnki.com.cn/Article/CJFDTOTAL-NJYK201906003.htm
[12] Siu CW, Wang M, Zhang XH, et al. Analysis of ventricular performance as a function of pacing site and mode[J]. Prog Cardiovasc Dis, 2008, 51(2): 171-182. doi: 10.1016/j.pcad.2008.01.001
[13] 张洁, 吴冬燕, 何乐, 等. 不同起搏部位的心室电机械同步性分析[J]. 临床心血管病杂志, 2021, 37(5): 440-446. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202105010.htm
[14] 庞博, 李光源, 王永槐, 等. 二维斑点追踪成像技术评价完全性左束支传导阻滞患者的左心室功能及同步性[J]. 中华医学超声杂志(电子版), 2019, 16(11): 841-847. doi: 10.3877/cma.j.issn.1672-6448.2019.11.009
[15] Sharma PS, Dandamudi G, Herweg B, et al. Permanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: A multicenter experience[J]. Heart rhythm, 2017, 15(3): 413.
[16] Rudski LG, Lai WW, Afifilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography[J]. J Am Soc Echocardiogr, 2010, 23: 685-713. doi: 10.1016/j.echo.2010.05.010
[17] Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging[J]. European Heart Journal-Cardiovascular Imaging, 2018, 20: 111.
[18] 高海叶, 邓爱云, 王小娟, 等. 速度向量成像技术对肺动脉高压患者右心室收缩功能及同步性的评估[J]. 中国循环杂志, 2019, 34(5): 75-80. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH201905014.htm
[19] 李慧, 胡奕然, 顾敏, 等. 实时三维超声心动图联合斑点追踪技术评价不同部位起搏对右室功能的影响[J]. 中国分子心脏病学杂志, 2020, 113(4): 26-30. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGFB202004005.htm
-




 下载:
下载: