Effect of Dulaglutide on the number of endothelial progenitor cells in peripheral blood of patients with type 2 diabetes mellitus
-
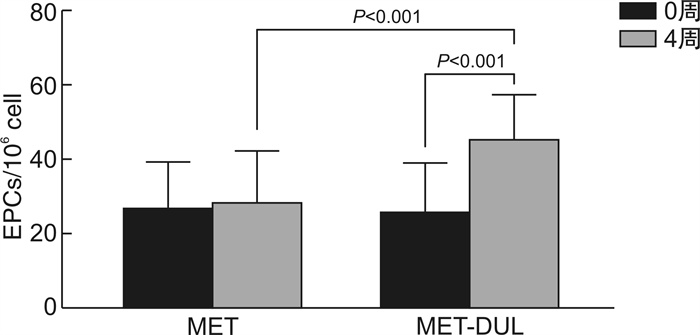
摘要: 目的 了解度拉糖肽对2型糖尿病(T2DM)患者外周血内皮祖细胞(EPCs)数量的影响及其相关因素。方法 选取60例口服二甲双胍1000 mg/d治疗的T2DM患者,随机分为二甲双胍增量组(MET组,30例,口服二甲双胍2000 mg/d)和二甲双胍联合度拉糖肽治疗组(MET-DUL组,30例,二甲双胍1000 mg/d联合度拉糖肽1.5 mg/周皮下注射),持续治疗4周。采用流式细胞术检测治疗前后CD34、CD133、KDR均为阳性的EPCs数量。结果 经4周治疗后,MET组外周血EPCs数量改变无统计学意义(P>0.05),而MET-DUL组中外周血EPCs数量[(45.8±11.6)/106cell∶(26.1±13.4)/106cell],一氧化氮(NO)[(118.9±18.6)μmol/L∶(71.6±13.9)μmol/L]均高于治疗前(P< 0.05),BMI[(26.3±2.6) kg/m2:(27.1±2.5) kg/m2]低于治疗前(P< 0.05)。MET-DUL组中ΔEPCs与ΔBMI、ΔFPG相关系数(r)为-0.296、-0.218(P< 0.05),与ΔNO的r为0.389(P< 0.05)。结论 度拉糖肽可提高T2DM患者外周血EPCs数量。Abstract: Objective To understand the effect of dulaglutide on the number of endothelial progenitor cells(EPCs) in peripheral blood of patients with type 2 diabetes mellitus(T2DM) and its related factors.Methods A total of 60 T2DM patients treated with oral metformin 1000 mg/day were selected and randomly divided into metformin incremental group(MET group, 30 cases, oral metformin 2000 mg/day) and metformin combined with dulaglutide treatment group(MET-DUL Group, 30 cases, metformin 1000 mg/day combined with subcutaneous injection of dulaglutide 1.5 mg/week) for 4 weeks. Flow cytometry was used to detect the number of EPCs positive for CD34, CD133 and KDR before and after treatment.Results After 4 weeks of treatment, the number of peripheral blood EPCs in the MET group did not change significantly(P>0.05), while the number of peripheral blood EPCs in the MET-DUL group[(45.8±11.6)/106 cell vs (26.1±13.4)/106 cell], nitric oxide(NO) [(118.9±18.6) μmol/L vs (71.6±13.9) μmol/L]were higher than those before treatment(P< 0.05), BMI[(26.3±2.6) kg/m2: (27.1±2.5) kg/m2]was lower than that before treatment(P< 0.05). In the MET-DUL group, the correlation coefficients(r) of ΔEPCs with ΔBMI and ΔFPG were-0.296, -0.218, and therwith ΔNO was 0.389(P< 0.05).Conclusion Dulaglutide can increase the number of blood EPCs in T2DM patients.
-
Key words:
- Dulaglutide /
- diabetes mellitus, type 2 /
- endothelial progenitor cell /
- nitric oxide
-

-
表 1 两组间治疗前后一般资料及临床特征比较
Table 1. Comparision of general data and clinical characteristics between pre-treatment and post-treatment in two groups
例(%), X±S 变量 MET组 t/χ2 P MET-DUL组 t/χ2 P 0周(30例) 4周(30例) 0周(30例) 4周(30例) 男性 17(56.7) 17(56.7) 0.000 1.000 18(60.0) 17(58.6) 0.012 0.914 年龄/岁 43.5±4.4 43.5±4.4 0.000 1.000 42.9±5.3 42.8±5.4 0.015 0.893 病程/月 9.3±1.4 9.3±1.4 0.000 1.000 8.8±1.3 8.7±1.2 0.016 0.882 BMI/(kg·m-2) 26.8±2.7 26.7±2.9 0.083 0.935 27.1±2.5 26.3±2.6 2.563 0.028 SBP/mmHg 141±14 140±15 0.096 0.924 139±12 136±13 -0.167 0.238 DBP/mmHg 94±11 94±12 0.077 0.967 93±12 93±12 0.019 0842 FPG/(mmol·L-1) 7.4±1.1 7.0±1.2 2.400 0.030 7.5±0.9 6.9±1.0 2.773 0.022 HbA1c/% 7.2±0.2 - - - 7.1±0.3 - - - TG/(mmol·L-1) 2.2±0.8 2.0±0.9 0.993 0.347 2.3±0.9 1.9±1.0 1.104 0.215 TC/(mmol·L-1) 5.7±1.3 5.6±1.2 0.205 0.842 5.6±1.2 5.5±1.1 0.198 0.796 HDL-C/(mmol·L-1) 1.4±0.3 1.4±0.4 0.106 0.918 1.3±0.2 1.4±0.3 -0.153 0.278 LDL-C/(mmol·L-1) 3.5±0.5 3.5±0.4 0.113 0.853 3.4±0.3 3.2±0.4 0.764 0.426 NO/(μmol·L-1) 68.9±14.7 73.6±13.9 -0.154 0.265 71.6±13.9 118.9±18.6 -10.537 < 0.001 VEGF/(pmol·mL-1) 211.7±25.8 219.5±22.7 -0.113 0.312 208.3±26.7 222.7±27.1 -0.242 0.136 SDF-1α/(pmol·mL-1) 2056.1±512.3 2069.4±496.5 -0.203 0.194 1989.6±531.7 2067.5±515.3 -0.198 0.176 EPCs/106cell 27.2±12.3 28.9±13.4 -0.189 0.236 26.1±13.4 45.8±11.6 -8.563 < 0.001 表 2 两组治疗前后临床指标Δ值的比较
Table 2. Comparision of Δ value of clinical indices before and after treatment between two groups
X±S 变量 MET组(30例) MET-DUL组(29例) t P ΔBMI/(kg·m-2) -0.11±0.08 -0.82±0.13 10.346 < 0.001 ΔSBP/mmHg -1.08±0.11 -2.45±0.27 0.895 0.504 ΔDBP/mmHg 0.02±0.04 0.03±0.02 -0.107 0.343 ΔFPG/(mmol·L-1) -0.41±0.04 -0.52±0.09 1.276 0.152 ΔTG/(mmol·L-1) -0.22±0.07 -0.25±0.10 0.374 0.723 ΔTCH/(mmol·L-1) 0.09±0.05 0.08±0.04 0.186 0.836 ΔHDL-C/(mmol·L-1) 0.01±0.01 0.01±0.01 0.068 0.971 ΔLDL-C/(mmol·L-1) 0.01±0.01 0.09±0.05 -0.074 0.462 ΔNO/(μmol·L-1) 6.14±1.08 38.9±9.83 -13.875 < 0.001 ΔVEGF/(pmol·ml-1) 9.18±0.85 13.71±6.63 -1.187 0.185 ΔSDF-1α/(pmol·ml-1) 13.95±5.37 49.26±25.32 -1.837 0.092 ΔEPCs/ 10-6cell 2.12±0.97 19.97±5.86 -10.479 < 0.001 表 3 MET组ΔEPCs与其他临床指标Δ值间的Pearson相关分析
Table 3. Pearson correlation analysis of ΔEPCs with Δ value of other clinical indices in MET group
变量 ΔEPCs r P ΔBMI -0.104 0.298 ΔSBP 0.061 0.657 ΔDBP 0.045 0.701 ΔFPG -0.165 0.102 ΔTG -0.098 0.321 ΔTCH 0.013 0.828 ΔHDL-C 0.084 0.593 ΔLDL-C 0.057 0.687 ΔNO 0.182 0.114 ΔVEGF 0.102 0.301 ΔSDF-1α 0.062 0.654 表 4 MET-DUL组ΔEPCs与其他临床指标Δ值间的Pearson相关分析
Table 4. Pearson correlation analysis of ΔEPCs with Δ value of other clinical indices in MET-DUL group
变量 ΔEPCs r P ΔBMI -0.296 0.013 ΔSBP 0.054 0.703 ΔDBP 0.048 0.784 ΔFPG -0.218 0.042 ΔTG -0.189 0.088 ΔTCH 0.018 0.801 ΔHDL-C 0.075 0.605 ΔLDL-C -0.101 0.287 ΔNO 0.389 0.001 ΔVEGF 0.161 0.159 ΔSDF-1α 0.138 0.285 表 5 MET-DUL组中ΔEPCs与其他临床指标Δ值的多元线性回归分析
Table 5. Multiple linear regressions analysis of ΔEPCs with Δ value of other clinical indices in MET-DUL group
变量 β SE t P 95%CI ΔBMI -0.217 0.097 -3.328 0.019 0.351~0.892 ΔNO 0.396 0.127 7.591 0.000 0.195~0.767 -
[1] Htike ZZ, Zaccardi F, Papamargaritis D, et al. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: a systematic review and mixed-treatment comparison analysis[J]. Diabetes Obes Metab, 2017, 19(4): 524-536. doi: 10.1111/dom.12849
[2] 周子华. 新型降糖药物的降压作用[J]. 临床心血管病杂志, 2021, 37(8): 692-694. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202108002.htm
[3] Scott LJ. Dulaglutide: a review in type 2 diabetes[J]. Drugs, 2020, 80(2): 197-208. doi: 10.1007/s40265-020-01260-9
[4] Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes(REWIND): a doubleblind, randomised placebocontrolled trial[J]. Lancet, 2019, 394(10193): 121130.
[5] 王威, 张颖倩, 李中轩, 等. 内皮祖细胞促进损伤血管再内皮化的机制[J]. 临床心血管病杂志, 2019, 35(8): 763-767. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201908019.htm
[6] Odent Grigorescu G, Rosca AM, Preda MB, et al. Synergic effects of VEGF-A and SDF-1 on the angiogenic properties of endothelial progenitor cells[J]. J Tissue Eng Regen Med, 2017, 11(11): 3241-3252. doi: 10.1002/term.2233
[7] Hu Z, Wang H, Fan G, et al. Danhong injection mobilizes endothelial progenitor cells to repair vascular endothelium injury via upregulating the expression of Akt, eNOS and MMP-9[J]. Phytomedicine, 2019, 61: 152850. doi: 10.1016/j.phymed.2019.152850
[8] Mudyanadzo TA. Endothelial progenitor cells and cardiovascular correlates[J]. Cureus, 2018, 10(9): e3342.
[9] Rigato M, Fadini GP. Circulating stem/progenitor cells as prognostic biomarkers in macro-and microvascular disease: a narrative review of prospective observational studies[J]. Curr Med Chem, 2018, 25(35): 4507-4517. doi: 10.2174/0929867324666170920154020
[10] 沐世昌, 荚杨洋, 陈明卫, 等. 封闭式负压引流对轻中度缺血糖尿病足溃疡患者外周血内皮祖细胞数量的影响[J]. 中华内分泌代谢杂志, 2017, 33(10): 816-821. doi: 10.3760/cma.j.issn.1000-6699.2017.10.002
[11] Mudyanadzo TA. Endothelial progenitor cells and cardiovascular correlates[J]. Cureus, 2018, 10(9): e3342.
[12] Kristensen SL, Rørth R, Jhund PS, et al. Cardiovascular, mortality, and kidney outcomes with GLP1 receptor agonists in patients with type 2 diabetes: a systematic review and metaanalysis of cardiovascular outcome trials[J]. Lancet Diabetes Endocrinol, 2019, 7(10): 776785.
[13] Xu M, Zhao X, Zheng M, et al. Acute effects of sitagliptin on progenitor cells and soluble mediators in newly diagnosed type 2 diabetes[J]. Int J Clin Pharmacol Ther, 2020, 58(9): 491-503. doi: 10.5414/CP203665
[14] Fadini GP, Mehta A, Dhindsa DS, et al. Circulating stem cells and cardiovascular outcomes: from basic science to the clinic[J]. Eur Heart J, 2020, 41(44): 4271-4282. doi: 10.1093/eurheartj/ehz923
[15] Richards WO, Prutzman KB, O'Hea MF, et al. Bariatric surgery improves the circulating numbers and biological activity of late outgrowth endothelial progenitor cells[J]. Surg Obes Relat Dis, 2014, 10(5): 906-913. doi: 10.1016/j.soard.2014.04.025
[16] Iorga RA, Bacalbasa N, Carsote M, et al. Metabolic and cardiovascular benefits of GLP-1 agonists, besides the hypoglycemic effect(Review)[J]. Exp Ther Med. 2020, 20(3): 2396-2400.
[17] De Ciuceis C, Agabiti-Rosei C, Rossini C, et al. Microvascular density and circulating endothelial progenitor cells before and after treatment with incretin mimetics in diabetic patients[J]. High Blood Press Cardiovasc Prev, 2018, 25(4): 369-378. doi: 10.1007/s40292-018-0279-7
[18] Luo X, Hu Y, He S, et al. Dulaglutide inhibits high glucose-induced endothelial dysfunction and NLRP3 inflammasome activation[J]. Arch Biochem Biophys, 2019, 671: 203-209. doi: 10.1016/j.abb.2019.07.008
[19] Wang R, Wang N, Han Y, et al. Dulaglutide alleviates LPS-induced injury in cardiomyocytes[J]. ACS Omega, 2021, 6(12): 8271-8278. doi: 10.1021/acsomega.0c06326
-




 下载:
下载: