An attempt to applicate parallel side to side anastomosis in LAD by minimally invasive coronary artery bypass grafting via left lateral chest wall
-
摘要: 目的初步探讨左胸前外侧小切口微创冠状动脉(冠脉)旁路移植(CABG)手术在前降支(LAD)靶血管上实施平行侧侧吻合的可行性和近期安全性。方法选取2019年11月—2022年2月于我院心外科经左胸前外侧小切口微创CABG手术LAD实施侧侧吻合患者共计29例,其中男21例,女8例。平均移植(2.07±0.26)支。全部患者均采用原位左侧乳内动脉(LIMA)与桡动脉(RA)或大隐静脉(SVG)构成复合桥,并依次完成至前降支靶血管的侧侧吻合以及其他靶血管序贯吻合。通过对术中瞬时血流参数、围术期心肌酶水平以及术后1周冠脉CTA结果观察LAD侧侧吻合的围术期临床表现。结果所有29例患者均按照原定计划顺利完成手术。术中对28例LIMA-LAD桥血管进行了瞬时流量仪测量,桥流量为(26.29±14.60) mL/min[对照组(29.72±20.93) mL/min,P=0.431]、搏动指数为2.93±1.02(对照组2.64±1.01,P=0.166)以及舒张期血供比例为71.21±10.09(对照组74.04±7.09,P=0.190),与对照组端侧吻合基线数据比较差异无统计学意义。术中1例患者未实施术中瞬时血流参数测定,但术后1周冠脉CTA显示复合桥血管通畅。本次研究中3例(10.3%)患者(6支桥)因各种原因未行术后1周冠脉CTA检查。其余26例冠脉CTA共发现桥血管闭塞2支,分别是1例为乳内动脉桥和SVG组成的复合桥第2站钝缘支吻合口闭塞,另1例为乳内动脉与RA组成的复合桥第2站后降支吻合口闭塞,桥血管闭塞率为3.77%;2例患者复合桥中第2站桥血管(RA-PDA)和第2、3站桥血管(RA-PL-PDA)显影略浅淡,但吻合口显示通畅,考虑存在“线样征”可能;1例患者复合桥第1站与第2站吻合口间桥血管显影浅淡,但与第1站和第2站吻合口位置显影良好,且断层观察显影良好,考虑与冠脉CTA成像相关。围术期心肌酶高于正常肌酸激酶同工酶界值10倍以上2例,即为上述出现桥血管闭塞人群(与对照组比较无统计学差异;P=0.110)。29例患者均存活并顺利出院,无伤口并发症。所有患者围术期无神经系统并发症。结论经左胸前外侧小切口微创CABG手术LAD侧侧吻合是一种可行的备选方案。
-
关键词:
- 非体外循环冠状动脉旁路移植术 /
- 侧侧吻合 /
- 微创 /
- 左胸前外侧小切口
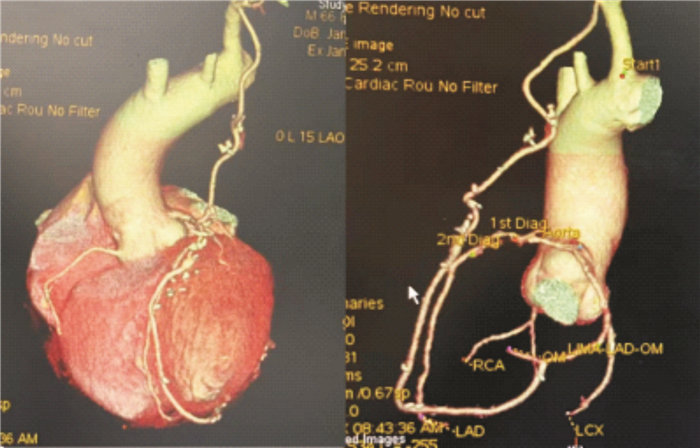
Abstract: ObjectiveTo investigate the feasibility and short-term safety of LIMA bypassing to LAD using parallel side to side anastomosis by left lateral thoracic small incision for minimally invasive coronary artery bypass grafting.MethodsA total of 29 patients, including 21 males and 8 females, were selected from November 2019 to February 2022 in the department of Cardiology of PKUPH. In all patients, the composite grafts were formed by in situ left internal mammary artery(LIMA) and radial artery(RA) or great saphenous vein(SVG), and anastomotic method is parallel side to side anastomosis in LAD and sequential anastomosis of other target vessels were successively completed. The perioperative clinical manifestations of parallel side to side anastomosis in LAD were observed by measuring intraoperative transient parameters of graft blood flow, perioperative myocardial enzyme levels and CCTA results one week after operation.ResultsAll 29 patients underwent surgery as scheduled. Intraoperative flow parameters of graft of LIMA-LAD were measured by TTFM in 28 patients. TTFM parameters included MGF(26.29±14.60 mL /min vs 29.72±20.93 mL /min in the control group, P=0.431), pulse index(PI)(2.93±1.02 vs 2.64±1.01 in the control group, P=0.166) and DF(71.21±10.09 vs 74.04±7.09 in the control group, P=0.190), which showed no statistical difference from the baseline data of end-to-end anastomosis in the control group. Intraoperative TTFM was not performed in one patient, but CCTA showed that the composite graft was unobstructed one week after surgery. In this study, 3 patients(10.3%)(6 Bridges) did not undergo coronary CCTA examination 1 week after surgery due to various reasons. In the other 26 cases of CCTA, two grafts occlusion were found, namely, occlusion of graft to OM in the second station of composite graft composed of LIMA and SVG in one case, occlusion of graft to PDA in the second station of composite graft composed of LIMA and RA in the other case, and the graft occlusion rate was 3.77%. The results of CCTA in two composite grafts showed the second section graft(RA-PDA) and the second and third sections graft(RA-PL-PDA) were slightly shallow, but the anastomosis showed unobstructed, suggesting the possibility of "string sign". The result of CCTA in one composite graft showed between the anastomotic sites at the first and second stations of the graft was shallow, but imaging was good in two anastomotic sites, and the CT section image was good, which was considered to be related to CCTA imaging. Two patients with perioperative myocardial enzymes more than 10 times higher than the normal CK-MB threshold were also patients with graft's occlusion. No statistical difference compared with the control group; P=0.110. All 29 patients survived and were discharged without wound complications. There were no perioperative neurological complications in all patients.ConclusionThe application of parallel side to side anastomosis in LAD by minimally invasive coronary artery bypass grafting via left lateral chest wall is a viable alternative. -

-
表 1 29例患者基线资料
Table 1. General data
X±S 项目 参数 年龄/岁 61.9±10.18 男性/例(%) 21(72.4) 移植支数/支 2.07±0.26 BMI/(kg·m-2) 25.8±3.38 术前射血分数/% 63.56±8.55 左室舒张末内径/cm 4.96±0.61 糖尿病/例(%) 8(27.6) 高血压/例(%) 20(69.0) 高脂血症/例(%) 13(44.8) 外周血管疾病/例(%) 1(3.4) 既往脑血管意外/例(%) 6(20.7) NYHA分级/级 2.31±0.47 既往陈旧性心肌梗死/例(%) 8(27.6) 既往PCI/例(%) 8(27.6) 慢性肾功能不全/例(%) 4(13.8) 围术期神经系统并发症/例(%) 0(0) 术后1周CTA桥血管失败率*/例(%) 2**/53#(3.8) 围术期CK-MB高于上限10倍/例(%) 2/29(6.9) *共计3例患者(共计6支桥)未行术后1周冠脉CTA检查,包括1例术后出现过敏事件;2例拒绝造影检查;**2支桥分别为LIMA-SVG-LAD-OM2中的OM2和LIMA-RA-LAD-PDA中的PDA;#排除1例AO-SVG-LCX桥血管。 表 2 实施CABG手术的方案和复合桥构成
Table 2. CABG operation and composite bridge structure
例(%) 复合桥构成 比例 LIMA-SVG-LAD-PL 2(6.9) LIMA-SVG-LAD-OM2 1(3.4) LIMA-SVG-LAD-LCX 1(3.4) LIMA-SVG-LAD-Dx 1(3.4) LIMA-RA-LAD-RCA 2(6.9) LIMA-RA-LAD-PL 2(6.9) LIMA-RA-LAD-PL-PDA 1(3.4) LIMA-RA-LAD-PDA 10(34.5) LIMA-RA-LAD-OM 2(6.9) LIMA-RA-LAD-LCX 7(24.1) 总和* 29(100) LCX:回旋支;RCA:右冠脉,PDA:后降支;PL:左室后支;OM:钝缘支;Dx:对角支。*总和中不包括微创侧切口下实施的1支AO-SVG-LCX移植。 -
[1] Ahn JM. Comparison of stenting versus bypass surgery according to the completeness of revascularization in severe coronary artery disease: patient-level pooled analysis of the SYNTAX, PRECOMBAT, and BEST Trials[J]. JACC Cardiovasc Interv, 2017, 10(14): 1415-1424. doi: 10.1016/j.jcin.2017.04.037
[2] Head SJ. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data[J]. Lancet, 2018, 391(10124): 939-948. doi: 10.1016/S0140-6736(18)30423-9
[3] 赵舟, 张显贵, 张国栋, 等. 非常规情况下使用大隐静脉替代左侧乳内动脉实施前降支再血管化治疗的围术期表现[J]. 临床心血管病杂志, 2020, 36(12): 1125-130. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202012012.htm
[4] 杨威, 陈彧, 陈生龙, 等. 微创单支冠状动脉旁路移植术单中心505例经验[J]. 中华胸心血管外科杂志, 2021, 37(7): 4.
[5] Kawajir I, Hidetak E. Bilateral internal thoracic artery grafting: in situ or composite?[J]. Ann Cardiothoracic Surg, 2018, 7(5): 673-680. doi: 10.21037/acs.2018.05.16
[6] 张国栋, 秦俊超, 张显贵, 等. 原位左侧乳内动脉重建前降支血管术中瞬时血流参数对围术期不良事件的预测价值[J]. 临床心血管病杂志, 2020, 36(9): 863-867. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202009018.htm
[7] 韩增强, 张国栋, 刘刚, 等. 原位或游离右侧乳内动脉用于双侧乳内动脉冠状动脉旁路移植术[J]. 临床心血管病杂志, 2020, 36(7): 640-643. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202007013.htm
[8] Staalsen NH. The anastomosis angle does change the flow fields at vascular end-to-side anastomoses in vivo[J]. J Vascular Surg, 1995, 21(3): 460-471. doi: 10.1016/S0741-5214(95)70288-1
[9] Tsuku I, Hiroyuk I. Longer coronary anastomosis provides lower energy loss in coronary artery bypass grafting[J]. Heart and Vessels, 2017, 32(1): 83-89. doi: 10.1007/s00380-016-0880-4
[10] LaDis A, John F Jr. Computational simulations demonstrate altered wall shear stress in aortic coarctation patients treated by resection with end-to-end anastomosis[J]. Congenital Heart Disease, 2011, 6(5): 432-443. doi: 10.1111/j.1747-0803.2011.00553.x
[11] Wei ZH. Distal end side-to-side anastomosis of sequential coronary bypass for size mismatched saphenous vein grafts and coronary arteries[J]. Perfusion, 24 May. 2022, doi: 10.1177/02676591221100738.
[12] Boner T, Michae L. A numerical study of blood flow in coronary artery bypass graft side-to-side anastomoses[J]. Ann Biomedical Enginee, 2002, 30(5): 599-611. doi: 10.1114/1.1481052
[13] Tinic A, Grigor E. Long-term graft patency after coronary artery bypass grafting: Effects of surgical technique[J]. Experimental and Therapeutic Medicine, 2019, 17(1): 359-367.
[14] Shimahar A, Yusuk E. Optimal target vessel selection for composite and sequential radial artery grafting with an in situ internal thoracic artery[J]. J Cardiac Surg, 2017, 32(10): 613-620.
[15] Akasaka T. Flow dynamics of angiographically no-flow patent internal mammary artery grafts[J]. JACC, 1998, 31(5): 1049-1056.
[16] Kho T, Umesh N. Radial artery bypass grafts have an increased occurrence of angiographically severe stenosis and occlusion compared with left internal mammary arteries and saphenous vein grafts[J]. Circulation, 2004, 109(17): 2086-2091.
[17] He GW. Arterial grafts for coronary artery bypass grafting: biological characteristics, functional classification, and clinical choice[J]. Annals Thoracic Surgery, 1999, 67(1): 277-284.
[18] Walpot H, Beat H. Vascular adaptation of the internal thoracic artery graft early and late after bypass surgery[J]. J Thoracic Cardiovasc Surg, 2008, 136(4): 876-883.
-




 下载:
下载: