The association of vitamin D levels and sleep status with cardiovascular disease among the elderly: a cohort study
-
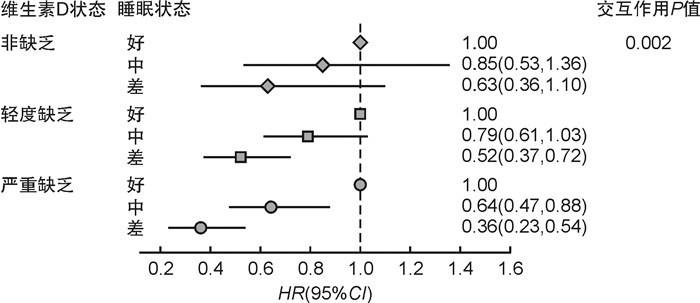
摘要: 目的 探讨老年人群的维生素D水平及睡眠状态与心血管疾病的关联。方法 基于前瞻性队列研究,于2016年8月—2020年7月招募年龄大于60岁的体检老人7837人,每年随访1次,平均随访3年。基线时志愿者做一份结构化问卷,并采集静脉血检测维生素D水平。睡眠状态由5个睡眠问题组成,包括持续时间、睡眠类型、失眠、打鼾和白天过度嗜睡,分为好、中、差3组。结局指标为脑卒中、心肌梗死、冠心病等心血管疾病。结果 本研究人群,平均年龄为(68.86±14.16)岁,心血管疾病发生率为12.0%。睡眠状态好、中、差的比例分别为23.1%、63.6%和13.3%。与维生素D严重缺乏组比较,维生素D轻度缺乏组(HR=0.56,95%CI:0.48,0.66)及非缺乏组(HR=0.41,95%CI:0.34,0.51)心血管疾病发生风险较低。睡眠状态差可增加心血管疾病发生风险。维生素D水平与睡眠状态存在交互作用(P=0.002),在维生素D严重缺乏人群中,与睡眠状态差组比较,睡眠状态中等组(HR=0.64,95%CI:0.47,0.88)及睡眠状态好组(HR=0.36,95%CI:0.23,0.54)心血管疾病发生风险较低,而在维生素D非缺乏人群中未发现这种关联。结论 高维生素D水平及健康的睡眠可降低老年人群的心血管疾病发生风险,较高的维生素D水平可减弱不健康睡眠所带来的危害。Abstract: Objective To investigate the association of vitamin D levels and sleep status with cardiovascular disease in an elderly population.Methods Based on a prospective cohort study, 7837 seniors attending medical examinations aged>60 years were recruited from August 2016 to July 2020 and followed up once a year for a mean follow-up period of 3 years. Volunteers were given a structured questionnaire at baseline and venous blood was collected for vitamin D levels. Sleep status consisted of five sleep problems, including sleep duration, chronotype, insomnia, snoring, and daytime sleepiness, divided into three groups: healthy, moderate, and poor. The outcomes were stroke, myocardial infarction, and coronary artery disease.Results In this study population, the mean age was(68.86±14.16) years and the incidence of cardiovascular disease was 12.0%. The percentage of healthy, moderate, and poor sleep status was 23.1%, 63.6%, and 13.3%, respectively. The risk of cardiovascular disease was lower in the mild vitamin D deficient group(HR=0.56, 95%CI: 0.48, 0.66) and the non-deficient group(HR=0.41, 95%CI: 0.34, 0.51) compared with the severe vitamin D deficient group. The risk of cardiovascular disease was higher in the poor sleep status group. There was an interaction between vitamin D levels and sleep status(P=0.002), with a lower risk of cardiovascular disease in the moderate sleep status group(HR=0.64, 95%CI: 0.47, 0.88) and the healthy sleep status group(HR=0.36, 95%CI: 0.23, 0.54) compared with the poor sleep status group in the severe vitamin D deficient population, and in the no such association was found in the vitamin D non-deficient group.Conclusion High vitamin D levels and healthy sleep reduce the risk of cardiovascular disease in the elderly population, and higher levels of vitamin D attenuate the adverse effects of unhealthy sleep.
-
Key words:
- sleep /
- vitamin D /
- aged /
- cardiovascular disease
-

-
表 1 不同维生素D状态的老年人群基线特征分析
Table 1. Characteristics of the elder population in different vitamin D status
例(%), X±S 项目 维生素D F/χ2值 P值 严重缺乏组(1636例) 轻度缺乏组(4106例) 非缺乏组(2095例) 一般人口学特征 年龄/岁 68.93±14.15 68.91±14.23 68.72±14.02 1.663 0.190 男性 732(44.7) 1868(45.5) 894(42.7) 1.491 0.106 小学及以下 1009(61.7) 2526(61.5) 1346(64.2) 1.720 0.094 月收入 < 3000元 1186(72.5) 2880(70.1) 1482(70.7) 3.135 0.209 健康状况 BMI/(kg·m-2) 21.71±3.061) 21.38±2.802) 20.94±2.653) 36.106 < 0.001 总胆固醇/(mmol·L-1) 6.05±0.951) 5.94±0.952) 5.81±0.923) 12.921 < 0.001 高密度脂蛋白胆固醇/(mmol·L-1) 1.99±0.39 2.01±0.36 2.00±0.36 0.208 0.812 空腹血糖/(mmol·L-1) 4.55±0.441) 4.50±0.402) 4.46±0.393) 18.562 < 0.001 收缩压/mmHg 141.62±15.551) 140.28±14.622) 138.34±14.143) 55.187 < 0.001 慢性病史(高血压、冠心病等) 728(44.5) 1740(42.4)2) 797(38.0)3) 17.570 < 0.001 慢性病用药 409(25.0) 1019(24.8) 486(23.2) 2.344 0.310 生活方式 吸烟 684(41.8) 1673(40.7) 846(40.4) 0.830 0.660 饮酒 576(35.2) 1526(37.2) 800(38.2) 3.562 0.168 体力活动 < 5次/周a) 730(44.6) 1814(44.2) 955(45.6) 1.109 0.574 晒太阳 < 5次/周b) 179(10.9) 478(11.6)2) 320(15.3)3) 21.186 < 0.001 与维生素D轻度缺乏组比较,1)P < 0.05;与维生素D非缺乏组比较,2)P < 0.05;与维生素D严重缺乏组比较,1)P < 0.05。a)体力活动定义为每天30 min以上的中等程度活动;b)晒太阳定义为每天不少于30 min的阳光接触。 表 2 老年人群维生素D状态与CVD的关联
Table 2. The association between vitamin D status and CVD among elder people
例(%) 维生素D状态 CVD P值 单因素模型 多因素模型 严重缺乏 306(18.7) 1.00 1.00 轻度缺乏 463(11.3) < 0.001 0.55(0.47,0.64) 0.56(0.48,0.66) 非缺乏 171(8.2) 0.39(0.62,0.47) 0.41(0.34,0.51) 注:多因素模型调整睡眠、年龄、性别、教育程度、收入、BMI、空腹血糖、高密度脂蛋白胆固醇、总胆固醇、收缩压、吸烟、饮酒、体力活动及晒太阳频率。 表 3 老年人群睡眠状态与CVD的关联
Table 3. The association between sleep status and CVD among elder people
睡眠状态 维生素D/(nmol·L-1)1) CVD 例(%)1) 单因素模型 多因素模型 差 38.47±17.93 172(16.5) 1.00 1.00 中 40.88±18.65 618(12.4) 0.71(0.59,0.86) 0.73(0.61,0.88) 好 40.99±17.69 150(8.3) 0.46(0.36,0.57) 0.44(0.35,0.56) 注:多因素模型调整维生素D状态、年龄、性别、教育程度、收入、BMI、空腹血糖、高密度脂蛋白胆固醇、总胆固醇、收缩压、吸烟、饮酒、体力活动及晒太阳频率。1)P < 0.05。 -
[1] Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2019, 394(10204): 1145-1158. doi: 10.1016/S0140-6736(19)30427-1
[2] Jani R, Mhaskar K, Tsiampalis T, et al. Circulating 25-hydroxy-vitamin D and the risk of cardiovascular diseases. Systematic review and meta-analysis of prospective cohort studies[J]. Nutr Metab Cardiovasc Dis, 2021, 31(12): 3282-3304. doi: 10.1016/j.numecd.2021.09.003
[3] 罗梦莹, 邹德玲. 维生素D对冠心病的发生及病变程度的影响[J]. 临床心血管病杂志, 2021, 37(6): 537-541. doi: 10.13201/j.issn.1001-1439.2021.06.009
[4] 史天珍, 王琴. 维生素D与血压控制的相关性[J]. 临床心血管病杂志, 2021, 37(11): 1047-1050. doi: 10.13201/j.issn.1001-1439.2021.11.016
[5] Manson JE, Cook NR, Lee IM, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease[J]. N Engl J Med, 2019, 380(1): 33-44. doi: 10.1056/NEJMoa1809944
[6] Asemi Z, Hashemi T, Karamali M, et al. An Expression of Concern from the AJCN Editorial Office about: Effects of vitamin D supplementation on glucose metabolism, lipid concentrations, inflammation, and oxidative stress in gestational diabetes: a double-blind randomized controlled clinical trial[J]. Am J Clin Nutr, 2020, 112(5): 1406. doi: 10.1093/ajcn/nqaa319
[7] 龚和杨子, 邢丽菲, 康毅敏, 等. 血清维生素D代谢物与成年女性睡眠时间的相关性分析[J]. 实用临床医药杂志, 2022, 26(14): 26-30. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202214006.htm
[8] Hejazian SM, Ahmadian E, Zununi Vahed S, et al. The Association of Sleep Quality and Vitamin D Levels in Hemodialysis Patients[J]. Biomed Res Int, 2021, 2021: 4612091.
[9] Yan S, Tian Z, Zhao H, et al. A meta-analysis: Does vitamin D play a promising role in sleep disorders?[J]. Food Sci Nutr, 2020, 8(10): 5696-5709. doi: 10.1002/fsn3.1867
[10] Fan M, Sun D, Zhou T, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants[J]. Eur Heart J, 2020, 41(11): 1182-1189. doi: 10.1093/eurheartj/ehz849
[11] Wang M, Zhou T, Li X, et al. Baseline Vitamin D Status, Sleep Patterns, and the Risk of Incident Type 2 Diabetes in Data From the UK Biobank Study[J]. Diabetes Care, 2020, 43(11): 2776-2784. doi: 10.2337/dc20-1109
[12] 彭斌, 吴波. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51(9): 666-682. https://www.cnki.com.cn/Article/CJFDTOTAL-XDJB201911024.htm
[13] 中国医师协会心血管内科医师分会. 2020心肌梗死后心力衰竭防治专家共识[J]. 中国循环杂志, 2020, 35(12): 1166-1180. doi: 10.3969/j.issn.1000-3614.2020.12.002
[14] Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association[J]. Circulation, 2021, 143(21): e984-e1010.
[15] Gholami F, Moradi G, Zareei B, et al. The association between circulating 25-hydroxyvitamin D and cardiovascular diseases: a meta-analysis of prospective cohort studies[J]. BMC Cardiovasc Disord, 2019, 19(1): 248. doi: 10.1186/s12872-019-1236-7
[16] Al-Ishaq RK, Kubatka P, Brozmanova M, et al. Health implication of vitamin D on the cardiovascular and the renal system[J]. Arch Physiol Biochem, 2021, 127(3): 195-209.
[17] Sinha SK, Sun L, Didero M, et al. Vitamin D3 Repletion Improves Vascular Function, as Measured by Cardiorenal Biomarkers in a High-Risk African American Cohort[J]. Nutrients, 2022, 14(16): 3331.
[18] Izzo M, Carrizzo A, Izzo C, et al. Vitamin D: Not Just Bone Metabolism but a Key Player in Cardiovascular Diseases[J]. Life(Basel), 2021, 11(5): 452.
[19] Rai V, Agrawal DK. Role of Vitamin D in Cardiovascular Diseases[J]. Endocrinol Metab Clin North Am, 2017, 46(4): 1039-1059.
[20] Chen S, Swier VJ, Boosani CS, et al. Vitamin D Deficiency Accelerates Coronary Artery Disease Progression in Swine[J]. Arterioscler Thromb Vasc Biol, 2016, 36(8): 1651-1659.
[21] Mosavat M, Smyth A, Arabiat D, et al. Vitamin D and sleep duration: Is there a bidirectional relationship?[J]. Horm Mol Biol Clin Investig, 2020, 41(4).
[22] Ai M, Li SS, Chen H, et al. 1, 25(OH)2 D3 attenuates sleep disturbance in mouse models of Lewis lung cancer, in silico and in vivo[J]. J Cell Physiol, 2021, 236(11): 7473-7490.
[23] Huang G, Chen J, Zhan L, et al. Reduced serum vitamin D levels are associated with poor sleep quality in early stroke patients[J]. Front Nutr, 2022, 9: 937867.
[24] McCarthy MS, Elshaw EB, Szekely BM, et al. A Prospective Cohort Study of Vitamin D Supplementation in AD Soldiers: Preliminary Findings[J]. Mil Med, 2019, 184(Suppl 1): 498-505.
-




 下载:
下载: