Expression and clinical significance of serum NLRC4/ Caspase-1 in patients with atrial fibrillation
-
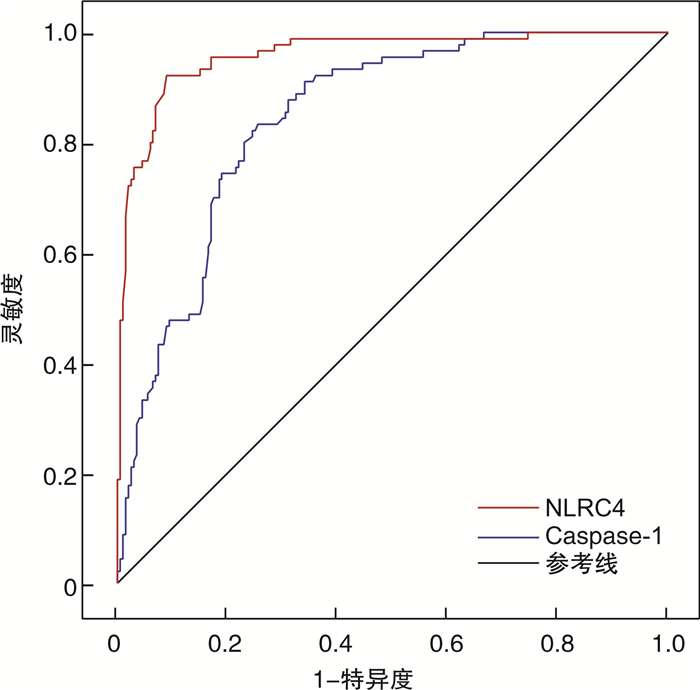
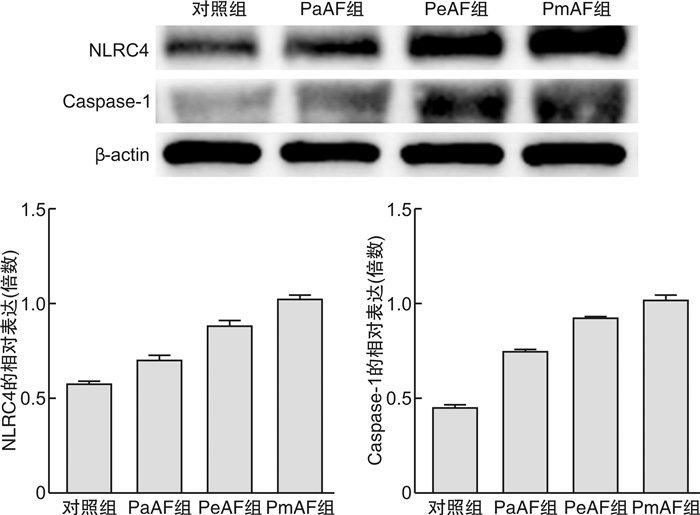
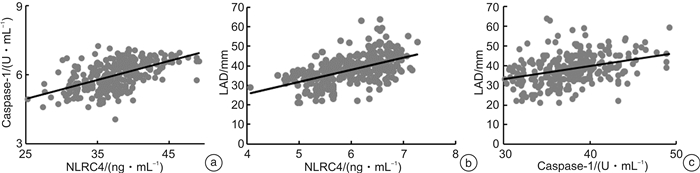
摘要: 目的 通过检测心房颤动(房颤)患者血清中NLR家族含CARD结构蛋白4(NLRC4)和半胱氨酸天冬氨酸特异蛋白酶1(Caspase-1)的表达水平变化,探讨二者在房颤发展中的规律及临床意义。方法 采用横断面研究方法,选取2020年12月—2021年12月在我院接受治疗的房颤患者200例,其中阵发性房颤(paroxysmal atrial fibrillation,PaAF)组61例,持续性房颤(persistent atrial fibrillation,PeAF)组71例,永久性房颤(permanent atrial fibrillation,PmAF)组68例。并选取90例同时期体检窦性心律(sinus rhythm,SR)者为对照组。ELISA和Western blot法分别测定血清中NLRC4、半胱氨酸天冬氨酸特异性蛋白酶1(Caspase-1)水平及通路蛋白表达情况,并分别与已测得的左心房内径(left atrial diameter,LAD)进行相关性分析。结果 与对照组比较,PaAF组、PeAF组和PmAF组NLRC4、Caspase-1表达水平升高(P < 0.01)。与PeAF组比较,PmAF组NLRC4、Caspase-1表达水平升高(P < 0.01)。与PaAF组比较,PeAF组和PmAF组NLRC4、Caspase-1表达水平升高(P < 0.01)。Western blot检测NLRC4/Caspase-1通路中各蛋白表达量,均存在上调趋势。Pearson法对NLRC4、Caspase-1与LAD进行相关性分析,结果显示在所有试验组中NLRC4浓度与Caspase-1、LAD呈正相关(r=0.540、0.516,P < 0.001);Caspase-1与LAD呈正相关(r=0.363,P < 0.001)。结论 NLRC4与Caspase-1在房颤患者血清表达水平明显升高,且与LAD有一定的相关性,NLRC4/Caspase-1的激活与表达可能与房颤的发生有关。
-
关键词:
- 心房颤动 /
- NLRC4 /
- 半胱氨酸天冬氨酸特异性蛋白酶1 /
- 左心房内径
Abstract: Objective To investigate the regulation and clinical significance of NLRC4 and Caspase-1 in the development of atrial fibrillation by detecting the expression levels of NLRC4 and Caspase-1 in the serum of atrial fibrillation patients.Methods A cross-sectional study was conducted to select 200 ATRIAL FIBRILLATION patients treated in our hospital from December 2020 to December 2021, including 61 patients in the paroxysmal atrial fibrillation (PaAF) group. There were 71 patients in the persistent atrial fibrillation (PeAF) group and 68 patients in the permanent atrial fibrillation (PmAF) group. A total of 90 patients with sinus rhythm (SR) were selected as the control group. The levels of NLRC4 and caspase-1 and the expression of pathway proteins in serum were measured by ELISA and Western blot, and the correlation between NLRC4 and LAD was analyzed.Results Compared with the control group, the expression levels of NLRC4 and Caspase-1 in PaAF, PeAF, and PmAF groups were significantly increased (P < 0.01). Compared with the PeAF group, the expression levels of NLRC4 and Caspase-1 in the PmAF group were significantly increased (P < 0.01). Compared with the PaAF group, the expression levels of NLRC4 and caspase-1 in PeAF and PmAF groups were significantly increased (P < 0.01). The expression levels of NLRC4/Caspase-1 proteins were up-regulated by Western blot. The Pearson method was used to analyze the correlation between NLRC4, Caspase-1, and LAD. The results showed that the concentration of NLRC4 was positively correlated with Caspase-1 and LAD in all experimental groups (r=0.540, 0.516, P < 0.001), Caspase-1 was positively correlated with LAD (r=0.363, P < 0.001).Conclusion The expression levels of NLRC4 and Caspase-1 in the serum of atrial fibrillation patients are significantly increased, and there is a certain correlation with LAD. The activation and expression of NLRC4/ Caspase-1 may be related to the occurrence of atrial fibrillation.-
Key words:
- atrial fibrillation /
- NLRC4 /
- Caspase-1 /
- left atrial diameter
-

-
表 1 临床基线资料比较
Table 1. Comparison of clinical baseline data
例(%), X±S 指标 对照组(90例) PaAF组(61例) PeAF组(71例) PmAF组(68例) F/χ2 P值 男性 46(51.11) 33(54.09) 38(53.52) 35(51.47) 2.579 0.461 HBP 42(46.67) 33(54.09) 35(49.29) 37(54.41) 3.806 0.283 SH 20(22.22) 14(22.95) 18(25.35) 10(14.71) 1.218 0.749 DM 9(10.00) 8(13.11) 11(15.49) 9(13.24) 4.270 0.118 CI 17(18.89) 13(21.31) 15(21.13) 13(19.12) 3.552 0.169 年龄/岁 65.81±10.79 69.70±9.24 70.23±10.66 66.44±9.46 3.625 0.014 WBC/(×109/L) 6.10±1.61 6.04±1.56 5.99±1.58 6.31±1.93 0.512 0.674 SBP/mmHg 139.98±16.97 136.95±21.73 134.87±19.16 136.99±18.90 0.988 0.399 DBP/mmHg 87.98±12.8 85.98±14.04 86.66±13.66 86.65±13.61 0.301 0.824 TG/(mmol·L-1) 1.44±0.88 1.54±0.87 1.44±0.99 1.41±0.79 0.252 0.861 Glu/(mmol·L-1) 5.59±1.33 5.96±1.61 5.87±1.73 5.68±1.39 1.185 0.316 Scr/(μmol·L-1) 67.6±11.86 68.33±14.76 70.86±16.39 67.74±18.25 0.725 0.538 ALT/(U·L-1) 21.67±10.33 24.49±12.25 24.21±12.31 23.68±11.09 1.006 0.390 AST/(U·L-1) 24.47±5.81 27.13±9.99 26.42±8.08 26.06±11.72 1.249 0.292 LVEF/% 59.22±5.40 57.03±4.34 53.46±6.03 50.13±7.67 36.628 < 0.001 LVEDD/mm 46.29±4.06 48.53±4.78 50.87±5.28 54.37±6.25 34.866 < 0.001 FS/% 32.90±3.16 31.02±4.46 28.63±7.64 24.60±6.15 31.398 < 0.001 AD 0(0) 57(93.44) 63(88.73) 61(89.70) 0.309 0.857 ACD 0(0) 57(93.44) 68(95.77) 65(95.59) 1.021 0.600 注:HBP:高血压;SH:吸烟史;DM:糖尿病;CI:脑梗死;WBC:白细胞;SBP:收缩压;DBP:舒张压;TG:甘油三酯;Glu:血糖;Scr:肌酐;ALT:谷丙转氨酶;AST:谷草转氨酶;LVEF:左室射血分数;LVEDD:左室舒张末期内径;FS:左心室缩短分数;AD:胺碘酮;ACD:抗凝药物。 表 2 不同分组房颤患者NLRC4、Caspase-1、CRP及LAD比较
Table 2. Comparison of NLRC4, Caspase-1, CRP and LAD in patients with atrial fibrillation in different groups
X±S 指标 对照组(90例) PaAF组(61例) PeAF组(71例) PmAF组(68例) F值 P值 NLRC4/(ng·mL-1) 5.31±0.37 5.98±0.441) 6.32±0.351)3) 6.61±0.241)3)4) 199.806 < 0.001 Caspase-1/(U·mL-1) 34.26±2.92 37.04±3.061) 38.31±3.651)4) 41.10±3.091)3)4) 66.643 < 0.001 CRP/(μg·L-1) 2.80±2.67 5.29±1.592) 8.47±5.692)4) 13.47±12.931)3)4) 31.721 < 0.001 LAD/mm 31.72±4.99 37.68±4.832) 41.16±6.701)4) 43.55±7.161)3)4) 59.418 < 0.001 与对照组比较,1)P < 0.01,2)P < 0.05;与PaAF组比较,3)P < 0.01,4)P < 0.05;与PeAF组比较,4)P < 0.05。 -
[1] 马长生. 房颤的流行病学进展[J]. 医学与哲学(B), 2016, 37(11): 8-9, 26. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZL201611004.htm
[2] 黎凯锋, 田灿辉, 潘俊安. 他汀类药物对房颤相关性急性缺血性脑卒中患者血浆Ox-LDL水平的影响及预后研究[J]. 临床急诊杂志, 2020, 21(12): 982-986. doi: 10.13201/j.issn.1009-5918.2020.12.010
[3] Jones DG, Haldar SK, Donovan J, et al. Biomarkers in Persistent AF and Heart Failure: Impact of Catheter Ablation Compared with Rate Control[J]. Pacing Clin Electrophysiol, 2016, 39(9): 926-934. doi: 10.1111/pace.12919
[4] Zhou X, Dudley SC Jr. Evidence for Inflammation as a Driver of Atrial Fibrillation[J]. Front Cardiovasc Med, 2020, 7: 62. doi: 10.3389/fcvm.2020.00062
[5] Sborgi L, Rühl S, Mulvihill E, et al. GSDMD membrane pore formation constitutes the mechanism of pyroptotic cell death[J]. Embo J, 2016, 35(16): 1766-1778. doi: 10.15252/embj.201694696
[6] Jorgensen I, Zhang Y, Krantz BA, et al. Pyroptosis triggers pore-induced intracellular traps(PITs)that capture bacteria and lead to their clearance by efferocytosis[J]. J Exp Med, 2016, 213(10): 2113-2128. doi: 10.1084/jem.20151613
[7] 夏熠, 李道博, 王运松, 等. 中性粒细胞与淋巴细胞比值对非瓣膜病心房颤动患者射频消融围术期抗凝出血风险的预测价值[J]. 临床心血管病杂志, 2020, 36(1): 55-59. doi: 10.13201/j.issn.1001-1439.2020.01.012
[8] Hu YF, Chen YJ, Lin YJ, et al. Inflammation and the pathogenesis of atrial fibrillation[J]. Nat Rev Cardiol, 2015, 12(4): 230-243. doi: 10.1038/nrcardio.2015.2
[9] Vyas V, Hunter RJ, Longhi MP, et al. Inflammation and adiposity: new frontiers in atrial fibrillation[J]. Europace, 2020, 22(11): 1609-1618. doi: 10.1093/europace/euaa214
[10] 吴俊杰, 蔡志雄. 心房颤动与心房纤维化的相关机制研究进展[J]. 现代医药卫生, 2017, 33(9): 1343-1347. doi: 10.3969/j.issn.1009-5519.2017.09.020
[11] Ding B, Liu P, Zhang FF, et al. Predicting Values of Neutrophil-to-Lymphocyte Ratio(NLR), High-Sensitivity C-Reactive Protein(hs-CRP), and Left Atrial Diameter(LAD)in Patients with Nonvalvular Atrial Fibrillation Recurrence After Radiofrequency Ablation[J]. Med Sci Monit, 2022, 28: e934569.
[12] Yao MH, Ren CL, Zhang L, et al. Short-term and mid-term effects of radiofrequency ablation in mitral valve surgery in patients with different left atrial sizes[J]. J Thorac Dis, 2020, 12(10): 6030-6038. doi: 10.21037/jtd-20-2953
[13] 王喆, 陈英伟, 董建增. 左心房结构相关指标对心房颤动导管消融术后复发的影响[J]. 临床心血管病杂志, 2020, 36(9): 786-789. doi: 10.13201/j.issn.1001-1439.2020.09.002
[14] van de Vegte YJ, Siland JE, Rienstra M, et al. Atrial fibrillation and left atrial size and function: a Mendelian randomization study[J]. Sci Rep, 2021, 11(1): 8431. doi: 10.1038/s41598-021-87859-8
[15] Onódi Z, Ruppert M, Kucsera D, et al. AIM2-driven inflammasome activation in heart failure[J]. Cardiovasc Res, 2021, 117(13): 2639-2651.
[16] Morin DP, Bernard ML, Madias C, et al. The State of the Art: Atrial Fibrillation Epidemiology, Prevention, and Treatment[J]. Mayo Clin Proc, 2016, 91(12): 1778-1810. doi: 10.1016/j.mayocp.2016.08.022
[17] Koniari I, Artopoulou E, Velissaris D, et al. Biomarkers in the clinical management of patients with atrial fibrillation and heart failure[J]. J Geriatr Cardiol, 2021, 18(11): 908-951.
[18] Bohne LJ, Jansen HJ, Daniel I, et al. Electrical and structural remodeling contribute to atrial fibrillation in type 2 diabetic db/db mice[J]. Heart Rhythm, 2021, 18(1): 118-129. doi: 10.1016/j.hrthm.2020.08.019
[19] Ma N, Lu R, Zhao DF, et al. Left Atrial Appendage Fibrosis and 3-Year Clinical Outcomes in Atrial Fibrillation After Endoscopic Ablation: A Histologic Analysis[J]. Ann Thorac Surg, 2020, 109(1): 69-76. doi: 10.1016/j.athoracsur.2019.05.055
[20] Mao Q, Liang XL, Zhang CL, et al. LncRNA KLF3-AS1 in human mesenchymal stem cell-derived exosomes ameliorates pyroptosis of cardiomyocytes and myocardial infarction through miR-138-5p/Sirt1 axis[J]. Stem Cell Res Ther, 2019, 10(1): 393. doi: 10.1186/s13287-019-1522-4
[21] Zhang L, Liu HY, Jia LL, et al. Exosomes Mediate Hippocampal and Cortical Neuronal Injury Induced by Hepatic Ischemia-Reperfusion Injury through Activating Pyroptosis in Rats[J]. Oxid Med Cell Longev, 2019, 2019: 3753485.
[22] Yang J, Hwang I, Lee E, et al. Bacterial Outer Membrane Vesicle-Mediated Cytosolic Delivery of Flagellin Triggers Host NLRC4 Canonical Inflammasome Signaling[J]. Front Immunol, 2020, 11: 581165. doi: 10.3389/fimmu.2020.581165
[23] Sundaram B, Kanneganti TD. Advances in Understanding Activation and Function of the NLRC4 Inflammasome[J]. Int J Mol Sci, 2021, 22(3): 1048. doi: 10.3390/ijms22031048
[24] Sanchez-Rodriguez E, Egea-Zorrilla A, Plaza-Díaz J, et al. The Gut Microbiota and Its Implication in the Development of Atherosclerosis and Related Cardiovascular Diseases[J]. Nutrients, 2020, 12(3): 605. doi: 10.3390/nu12030605
[25] Zuo K, Li J, Li KB, et al. Disordered gut microbiota and alterations in metabolic patterns are associated with atrial fibrillation[J]. Gigascience, 2019, 8(6): giz058. doi: 10.1093/gigascience/giz058
[26] Zhang Y, Zhang S, Li BL, et al. Gut microbiota dysbiosis promotes age-related atrial fibrillation by lipopolysaccharide and glucose-induced activation of NLRP3-inflammasome[J]. Cardiovasc Res, 2022, 118(3): 785-797. doi: 10.1093/cvr/cvab114
[27] Vecchié A, Bonaventura A, Toldo S, et al. IL-18 and infections: Is there a role for targeted therapies?[J]. J Cell Physiol, 2021, 236(3): 1638-1657. doi: 10.1002/jcp.30008
[28] Luan Y, Guo YY, Li SF, et al. Interleukin-18 among atrial fibrillation patients in the absence of structural heart disease[J]. Europace, 2010, 12(12): 1713-1718. doi: 10.1093/europace/euq321
[29] Gungor B, Ekmekci A, Arman A, et al. Assessment of interleukin-1 gene cluster polymorphisms in lone atrial fibrillation: new insight into the role of inflammation in atrial fibrillation[J]. Pacing Clin Electrophysiol, 2013, 36(10): 1220-1227. http://www.tandfonline.com/servlet/linkout?suffix=CIT0011&dbid=8&doi=10.1080%2F14728214.2018.1446941&key=23713812
[30] Fink SL, Bergsbaken T, Cookson BT. Anthrax lethal toxin and Salmonella elicit the common cell death pathway of caspase-1-dependent pyroptosis via distinct mechanisms[J]. Proc Natl Acad Sci U S A, 2008, 105(11): 4312-4317. doi: 10.1073/pnas.0707370105
[31] Mauro AG, Bonaventura A, Mezzaroma E, et al. NLRP3 Inflammasome in Acute Myocardial Infarction[J]. J Cardiovasc Pharmacol, 2019, 74(3): 175-187. doi: 10.1097/FJC.0000000000000717
[32] Yan B, Liu T, Yao C, et al. LncRNA XIST shuttled by adipose tissue-derived mesenchymal stem cell-derived extracellular vesicles suppresses myocardial pyroptosis in atrial fibrillation by disrupting miR-214-3p-mediated Arl2 inhibition[J]. Lab Invest, 2021, 101(11): 1427-1438. doi: 10.1038/s41374-021-00635-0
[33] Xie JY, Noeman M, Pimenta D, et al. C-reactive protein as a predictor for developing post-operative atrial fibrillation[J]. Europace, 2021, 23(1): 159. doi: 10.1093/europace/euaa303
-




 下载:
下载: