Association of neutrophil to lymphocyte ratio with plaque rupture in acute coronary syndrome patients diagnosed by optical coherence tomography
-
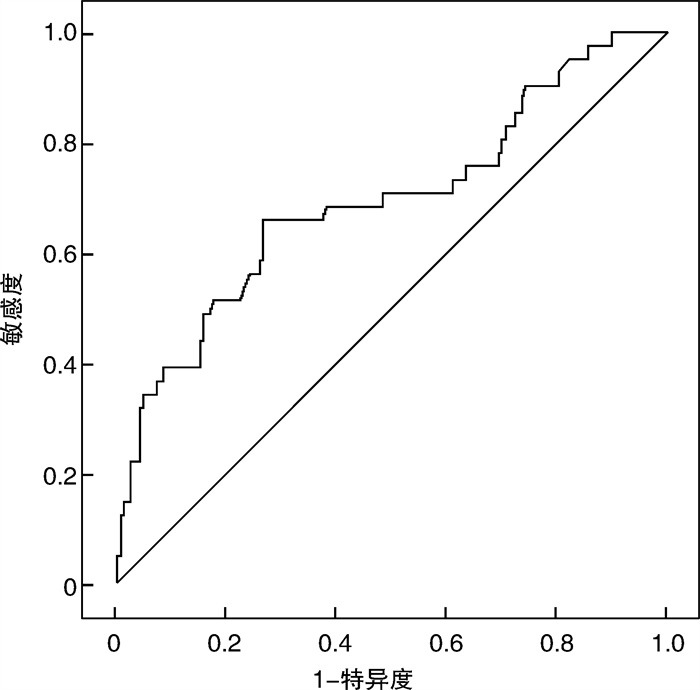
摘要: 目的 分析中性粒细胞与淋巴细胞比值(NLR)与急性冠状动脉综合征(acute coronary syndrome,ACS)患者光学相干断层扫描(optical coherence tomography,OCT)发现的冠状动脉(冠脉)斑块破裂的相关性。方法 入选2016年6月—2021年5月在上海交通大学医学院附属第九人民医院接受冠脉介入治疗并应用OCT进行冠脉病变评估的207例ACS患者为研究对象。根据OCT结果将所有受试者分为斑块破裂组(41例)和非斑块破裂组(166例),分析和比较两组间年龄、性别、心血管危险因素、心血管家族史、血常规、血脂等指标,及其与OCT诊断的冠脉斑块破裂的关系。结果 斑块破裂组年龄>65岁、性别为男性、有吸烟史人群的比例显著高于非破裂组。斑块破裂组患者的炎症指标[白细胞计数、中性粒细胞计数、C反应蛋白(CRP)水平]、肌钙蛋白I、低密度脂蛋白胆固醇(LDL-C)、NLR、血小板/淋巴细胞比值(PLR)均明显高于非斑块破裂组。其中,斑块破裂组的NLR水平显著高于非斑块破裂组,两组比较差异有统计学意义[3.33(1.94,6.34) vs 2.26(1.70,2.92),P < 0.001]。多因素logistic回归分析提示,NLR与ACS患者发生斑块破裂具有一定相关性(OR=1.360,95%CI:1.092~1.695,P=0.006)。ROC曲线分析发现,NLR>2.81是预测ACS患者冠脉斑块破裂的临界点,敏感度为65.9%,特异度为73.5%。结论 NLR与ACS冠脉病变发生斑块破裂密切相关,在预测斑块的不稳定性和ACS危险分层中具有一定临床价值。
-
关键词:
- 急性冠状动脉综合征 /
- 斑块破裂 /
- 中性粒细胞/淋巴细胞比值 /
- 光学相干断层扫描
Abstract: Objective To analyze the correlation between neutrophil to lymphocyte ratio (NLR) and plaque rupture in patients with acute coronary syndrome (ACS).Methods A total of 207 ACS patients who received coronary interventional procedures and optical coherence tomography (OCT) evaluations of coronary lesions at Shanghai Ninth People's Hospital from June 2016 to May 2021 were enrolled in the present study. According to the findings of OCT, all the subjects were divided into a non-plaque rupture group (n=166) and plaque rupture group (n=41). The differences in clinical characteristics such as age, sex, risk factors of cardiovascular diseases and the family history of coronary artery disease and laboratory parameters including blood routine examination and blood lipid levels between the two groups were compared. The correlation between hematological indices and plaque rupture in ACS was also analyzed.Results The proportion of patients aged>65, male and current smoking in plaque rupture group was significantly higher than that in non-rupture group. The inflammatory biomarkers(white blood cell count, neutrophil count, CRP level), troponin I, low density lipoprotein cholesterol(LDL-C), NLR and platelet to lymphocyte ratio(PLR) in plaque rupture group also significantly increased in comparison to non-rupture group. The NLR level in plaque rupture group was significantly higher than that in non-rupture group. The difference between the two groups was statistically significant[3.33(1.94, 6.34) vs 2.26(1.70, 2.92), P < 0.001]. Multivariate Logistic regression analysis showed that NLR was closely correlated with plaque rupture in ACS patients(OR=1.360, 95%CI: 1.092—1.695, P=0.006). ROC curve analysis found a cutoff point of NLR>2.81 for plaque rupture with 65.9% sensitivity and 73.5% specificity.Conclusion NLR is closely related to plaque rupture events in coronary lesions, and is associated with plaque rupture events in patients with acute coronary syndrome and can be used to predict plaque stability, early identification of vulnerable plaques, and risk stratification. -

-
表 1 斑块破裂组和非斑块破裂组患者的基线临床特征
Table 1. Baseline clinical characteristics of patients with or without plaque rupture
X±S, M(P25, P75) 项目 斑块破裂组(41例) 非斑块破裂组(166例) P值 年龄/岁 65.65±9.92 61.02±12.26 0.012 男性/例(%) 35(85.4) 114(68.7) 0.033 吸烟/例(%) 26(63.8) 66(39.8) 0.006 高血压/例(%) 27(65.9) 115(69.3) 0.672 糖尿病/例(%) 6(14.6) 41(24.7) 0.168 心血管疾病家族史/例(%) 12(29.3) 60(36.1) 0.408 抗血小板药物应用/例(%) 12(85.7) 60(88.2) 0.793 β受体阻滞剂应用/例(%) 4(28.6) 16(23.5) 0.689 ACEI/ARB应用/例(%) 6(42.9) 26(38.2) 0.859 他汀类应用/例(%) 8(57.1) 35(51.5) 0.699 BMI /(kg·m-2) 24.86±3.07 25.22±3.78 0.528 TG/(mmol·L-1) 4.02(3.74,4.71) 3.83(3.24,4.62) 0.112 TC/(mmol·L-1) 1.32(1.03,1.88) 1.48(1.02,2.12) 0.293 LDL-C/(mmol·L-1) 2.85(2.36,3.32) 2.52(1.98,3.18) 0.019 HDL-C/(mmol·L-1) 0.99(0.79,1.21) 1.00(0.86,1.18) 0.688 TnI/(ng·mL-1) 0.07(0.00,0.84) 0.01(0.00,0.02) < 0.001 BNP/(pg·mL-1) 43.00(23.50,101.50) 49.50(25.00,100.75) 0.704 CRP/(mg·L-1) 1.29(1.28,2.09) 1.33(1.28,2.17) 0.044 表 2 斑块破裂组和非斑块破裂组患者的血常规指标
Table 2. Hematological indexes of patients with or without plaque rupture
X±S, M(P25, P75) 指标 斑块破裂组(41例) 非斑块破裂组(166例) P值 红细胞计数/(×1012·L-1) 4.54±0.50 4.51±0.55 0.772 Hb/(g·L-1) 140.32±16.85 136.68±17.89 0.240 MCH/pg 30.80(29.70,31.60) 30.40(29.48,31.40) 0.198 MCV/fL 90.20(87.65,93.80) 90.30(87.55,93.55) 0.694 RDW/% 13.30(12.75,13.75) 13.00(12.50,13.50) 0.065 白细胞计数/(×109·L-1) 8.20(6.75,9.55) 6.30(5.20,7.61) < 0.001 中性粒细胞计数/(×109·L-1) 5.90(4.06,8.47) 3.80(3.00,4.93) < 0.001 淋巴细胞/(×109·L-1) 1.50(1.13,1.90) 1.67(1.30,2.10) 0.187 单核细胞/(×109·L-1) 0.49(0.38,0.66) 0.45(0.35,0.57) 0.165 NLR 3.33(1.94,6.34) 2.26(1.70,2.92) < 0.001 血小板计数/(×109·L-1) 227.00(202.00,266.50) 209.50(179.75,243.75) 0.096 MPV/fL 10.20(9.80,10.90) 10.30(9.70,10.90) 0.906 PDW/% 12.20(11.60,14.40) 12.45(11.10,14.23) 0.858 PLR 150.00(111.45,186.91) 128.58(97.88,165.00) 0.035 表 3 斑块破裂影响因素的logistic回归分析
Table 3. Influencing factors of plaque rupture analyzed by logistic regression analysis
指标 单因素 多因素 OR 95%CI P值 OR 95%CI P值 年龄>65岁 0.447 0.220~0.907 0.026 0.503 0.219~1.155 0.105 男性 2.661 1.054~6.717 0.038 1.711 0.532~5.503 0.368 吸烟史 2.626 1.295~5.328 0.007 1.813 0.737~4.463 0.195 LDL-C 1.438 1.013~2.042 0.042 1.105 0.714~1.708 0.655 TnI 1.168 1.041~1.311 0.008 1.130 1.010~1.265 0.033 CRP 0.949 0.832~1.082 0.433 NLR 1.348 1.170~1.553 < 0.001 1.360 1.092~1.695 0.006 PLR 1.006 1.001~1.011 0.013 0.996 0.987~1.006 0.430 -
[1] Zhang S, Diao J, Qi C, et al. Predictive value of neutrophil to lymphocyte ratio in patients with acute ST segment elevation myocardial infarction after percutaneous coronary intervention: a meta-analysis[J]. BMC Cardiovasc Disord, 2018, 18(1): 75. doi: 10.1186/s12872-018-0812-6
[2] Sugiyama T, Yamamoto E, Bryniarski K, et al. Nonculprit Plaque Characteristics in Patients With Acute Coronary Syndrome Caused by Plaque Erosion vs Plaque Rupture: A 3-Vessel Optical Coherence Tomography Study[J]. JAMA Cardiol, 2018, 3(3): 207-214. doi: 10.1001/jamacardio.2017.5234
[3] 罗莉曼, 付梦璐, 徐西振, 等. 腔内影像学指导下急性冠脉综合征发病机制及干预策略进展[J]. 内科急危重症杂志, 2019, 25(6): 508-511. https://www.cnki.com.cn/Article/CJFDTOTAL-NKJW201906024.htm
[4] 何路平, 于波. 冠状动脉腔内影像技术在高危斑块识别领域的研究现状及展望[J]. 中国循证心血管医学杂志, 2021, 13(11): 1396-1397, 1403. https://www.cnki.com.cn/Article/CJFDTOTAL-PZXX202111032.htm
[5] Fujii K, Kubo T, Otake H, et al. Expert consensus statement for quantitative measurement and morphological assessment of optical coherence tomography[J]. Cardiovasc Interv Ther, 2020, 35(1): 13-18. doi: 10.1007/s12928-019-00626-5
[6] Terada K, Kubo T, Kameyama T, et al. NIRS-IVUS for Differentiating Coronary Plaque Rupture, Erosion, and Calcified Nodule in Acute Myocardial Infarction[J]. JACC Cardiovasc Imaging, 2021, 14(7): 1440-1450. doi: 10.1016/j.jcmg.2020.08.030
[7] 帕孜丽亚·阿地力, 穆叶赛·尼加提. 动脉粥样硬化与炎症[J]. 临床心血管病杂志, 2020, 36(4): 303-306. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202004002.htm
[8] Ma Y, Yabluchanskiy A, Iyer RP, et al. Temporal neutrophil polarization following myocardial infarction[J]. Cardiovasc Res, 2016, 110(1): 51-61. doi: 10.1093/cvr/cvw024
[9] Horckmans M, Ring L, Duchene J, et al. Neutrophils orchestrate post-myocardial infarction healing by polarizing macrophages towards a reparative phenotype[J]. Eur Heart J, 38(3): 187-197.
[10] Mehta J, Dinerman J, Mehta P, et al. Neutrophil function in ischemic heart disease[J]. Circulation, 1989, 79(3): 549-556. doi: 10.1161/01.CIR.79.3.549
[11] Oylumlu M, Oylumlu M, Arslan B, et al. Platelet-to-lymphocyte ratio is a predictor of long-term mortality in patients with acute coronary syndrome[J]. Postepy Kardiol Interwencyjnej, 2020, 16(2): 170-176.
[12] Meeuwsen JAL, Wesseling M, Hoefer IE, et al. Prognostic value of circulating inflammatory cells in patients with stable and acute coronary artery disease[J]. Front Cardiovasc Med, 2017, 4: 44. doi: 10.3389/fcvm.2017.00044
[13] Forget P, Khalifa C, Defour JP, et al. What is the normal value of the neutrophil-to-lymphocyte ratio?[J]. BMC Res Notes, 2017, 10(1): 12. doi: 10.1186/s13104-016-2335-5
[14] 张林, 陈玥, 张宝红. 血小板-淋巴细胞比率、中性粒细胞-淋巴细胞比率及红细胞分布宽度在冠心病严重程度中的诊断价值[J]. 临床心血管病杂志, 2020, 36(9): 824-827. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202009010.htm
[15] 古力斯坦·艾斯卡尔, 布祖克拉·阿布都艾尼, 吐尔孙阿依·依斯米提, 等. 急性冠脉综合征患者微粒中miR-126与NLR间的关系及其临床意义[J]. 临床急诊杂志, 2021, 22(11): 720-726. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202111004.htm
[16] 牛园满, 李振宇, 邱婷婷, 张焕新, 孙海英, 桑威, 程海, 黄一虹, 徐开林, 李德鹏. 外周血中性粒细胞/淋巴细胞比值与真性红细胞增多症血栓事件关系的研究[J]. 临床血液学杂志, 2021, 34(3): 192-197. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202103011.htm
[17] Dong CH, Wang ZM, Chen SY. Neutrophil to lymphocyte ratio predict mortality and major adverse cardiac events in acute coronary syndrome: A systematic review and meta-analysis[J]. Clin Biochem, 2018, 52: 131-136.
[18] Khan S, Razaq HU, Khan A. In-Hospital Mortality Among Patients With Acute Coronary Syndrome With High Neutrophil To Lymphocyte Ratio[J]. J Ayub Med Coll Abbottabad, 2021, 33(Suppl 1)(4): S791-S795.
[19] Horne BD, Anderson JL, John JM, et al. Intermountain Heart Collaborative Study Group. Which white blood cell subtypes predict increased cardiovascular risk?[J]. J Am Coll Cardiol, 2005, 45(10): 1638-1643.
[20] Akyel A, Yaylaç, Erat M, et al. Neutrophil-to-lymphocyte ratio predicts hemodynamic significance of coronary artery stenosis[J]. Anatol J Cardiol, 2015, 15(12): 1002-1007.
[21] Oncel RC, Ucar M, Karakas MS, et al. Relation of neutrophil-to-lymphocyte ratio with GRACE risk score to in-hospital cardiac events in patients with ST-segment elevated myocardial infarction[J]. Clin Appl Thromb Hemost, 2015, 21(4): 383-388.
[22] Bajari R, Tak S. Predictive prognostic value of neutrophil-lymphocytes ratio in acute coronary syndrome[J]. Indian Heart J, 2017, 69 Suppl 1(Suppl 1): S46-S50.
-




 下载:
下载: