The value of combined index prediction model in predicting hospital death in patients with cardiogenic shock after myocardial infarction
-
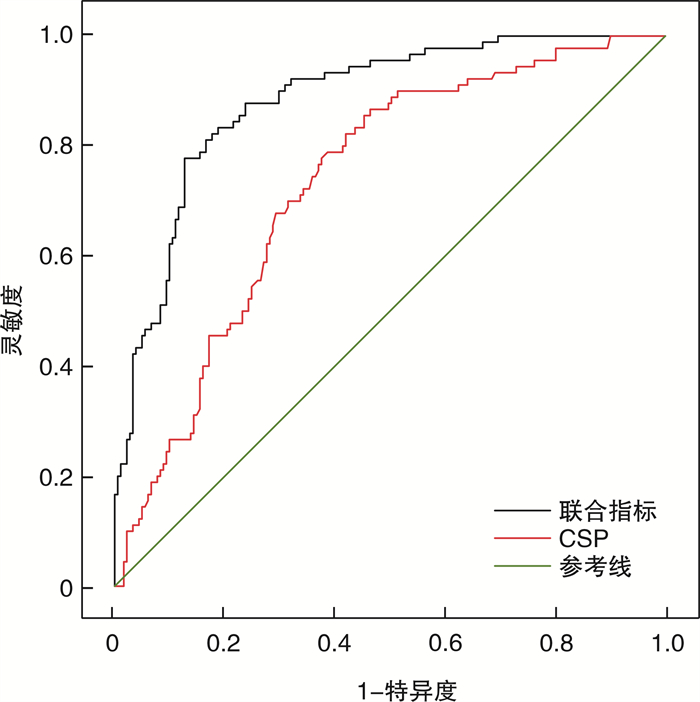
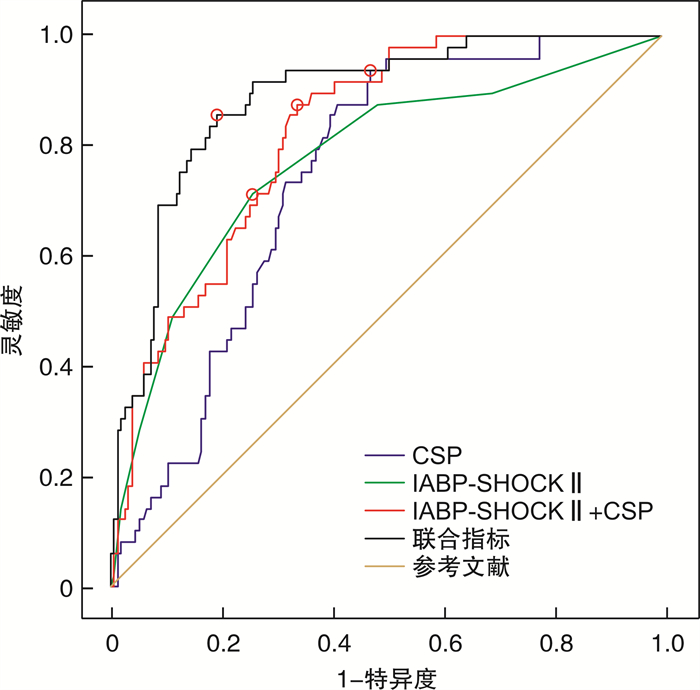
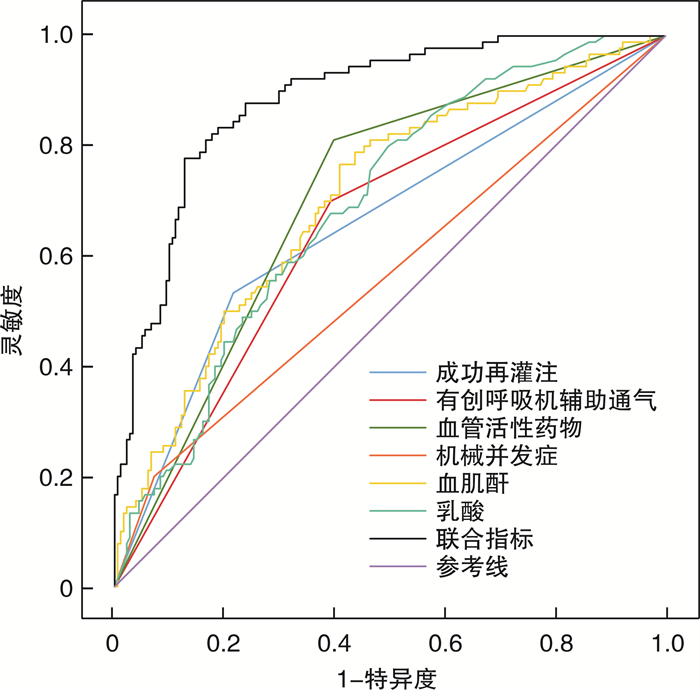
摘要: 目的 探讨急性心肌梗死(AMI)后心源性休克(CS)患者院内死亡的危险因素以及联合指标预测模型对AMI后CS患者院内死亡的预测价值。探讨联合指标预测模型、主动脉内球囊反搏-休克(IABP-SHOCK Ⅱ)评分、心源性休克预后(CSP)评分对行经皮冠状动脉介入术(PCI)的AMI后CS患者院内死亡的预测价值。方法 收集2019年1月—2022年11月于吉林大学第一医院心内科治疗的AMI后CS患者271例,根据院内存活情况将患者分为死亡组(90例)与存活组(181例),分析患者院内死亡的独立影响因素,并构建联合指标预测模型,用受试者工作特性曲线(ROC)和曲线下面积(AUC)评估联合指标预测模型、单个独立因素、CSP评分的预测价值,最后比较不同指标的AUC。从271例AMI后CS患者中筛选出199例接受PCI的患者,分为PCI死亡组(49例)与PCI存活组(150例),用ROC以及AUC评估联合指标预测模型、IABP-SHOCK Ⅱ、CSP、IABP-SHOCK Ⅱ+CSP评分的预测价值,最后再比较不同评分的AUC大小。结果 单因素分析显示,两组在意识不清、左室射血分数(LVEF)、机械并发症、白细胞绝对值(WBC)、中性粒细胞绝对值(NE)、单核细胞绝对值(MO)、酸碱度(pH)、乳酸(LAC)、碱剩余(BE)、门冬氨酸氨基转移酶(AST)、丙氨酸氨基转移酶(ALT)、直接胆红素(DBIL)、白蛋白(ALB)、血尿素氮(BUN)、血肌酐(Scr)、估测肾小球滤过率(eGFR)、B型脑钠肽(BNP)、两种以上血管活性药物、连续性肾脏替代治疗(CRRT)、有创呼吸机辅助通气、成功再灌注、CSP评分上均差异有统计学意义(均P < 0.05)。多因素回归分析显示,机械并发症(OR=6.824,P < 0.001)、LAC(OR=1.125,P=0.006)、Scr(OR=1.005,P=0.013)、两种及以上血管活性药物(OR=5.163,P < 0.001)、有创呼吸机辅助通气(OR=2.823,P=0.004)是AMI后CS患者院内死亡的独立危险因素;成功再灌注(OR=0.190,P < 0.001)是独立保护因素。在AMI后CS的患者中,联合指标预测模型、CSP评分的AUC分别为0.884、0.733。联合指标预测模型的灵敏度和特异度分别为77.8%和87.29%、CSP评分的灵敏度和特异度分别为86.67%和53.59%。在经PCI的AMI合并CS患者中,联合指标预测模型、IABP-SHOCK Ⅱ、CSP以及IABP-SHOCK Ⅱ+CSP评分的AUC分别为0.855、0.775、0.743、0.822。联合指标预测模型、IABP-SHOCK Ⅱ、CSP和IABP-SHOCK Ⅱ+CSP评分的灵敏度分别为85.71%、71.43%、93.88%和87.76%,特异度分别为80.67%、74%、52.67%和66%。结论 机械并发症、LAC、Scr、两种以上血管活性药物、有创呼吸机辅助通气是AMI后CS患者院内死亡的独立危险因素;成功再灌注是独立保护因素。联合指标预测模型对AMI后CS患者死亡预测价值良好,优于单个独立影响因素以及CSP评分。对于行PCI的AMI后CS患者,IABP-SHOCK Ⅱ与CSP评分的预测价值相当;而联合指标预测模型优于IABP-SHOCK Ⅱ、CSP、IABP-SHOCK Ⅱ+CSP评分。
-
关键词:
- 急性心肌梗死 /
- 心源性休克 /
- 主动脉内球囊反搏-休克Ⅱ评分 /
- 心源性休克预后评分
Abstract: Objective To explore the risk factors of hospital death in patients with cardiogenic shock(CS) after acute myocardial infarction(AMI), to determine the value of combined index prediction model in predicting hospital death in patients with CS after AMI. To explore the predictive value of combined index prediction model, intra-aortic balloon counterpulsation-shock Ⅱ(IABP-SHOCK Ⅱ) score, and cardiogenic shock prognosis(CSP) score in hospital death of CS patients with percutaneous coronary intervention(PCI) after AMI.Methods A total of 271 patients with CS after AMI, who were treated in the Department of Cardiology of the First Hospital of Jilin University from January 2019 to November 2022, were collected. All patients were divided into the death group(n=90) and the survival group(n=181) according to their in-hospital survival. The independent influencing factors of in-hospital death were analyzed and a combined index prediction model was established. The predictive value of combined index prediction model, single independent factor, and CSP score was evaluated by the receiver operating characteristic(ROC) curve and area under curve(AUC). Finally, the AUC of different indexes were compared. From 271 patients with CS after AMI, 199 patients with PCI were selected and divided into the PCI death group(n=49) and the PCI survival group(n=150). The predictive value of combined index predictive model, IABP-SHOCK Ⅱ, CSP, and IABP-SHOCK II+CSP score was evaluated by ROC and AUC, and the AUC of different scores were compared.Results Univariate analysis showed that there were significant differences in unconsciousness, left ventricular ejection fraction(LVEF), mechanical complications, white blood cell(WBC), neutrophil absolute value(NE), monocyte absolute value(MO), pH, lactic acid(LAC), base excess(BE), aspartate aminotransferase(AST), alanine aminotransferase(ALT), direct bilirubin(DBIL), albumin(ALB), blood urea nitrogen(BUN), serum creatinine(Scr), estimated glomerular filtration rate(eGFR), B-type brain natriuretic peptide(BNP), more than two vasoactive drugs, continuous renal replacement therapy(CRRT), invasive ventilator-assisted ventilation, successful reperfusion, and CSP score between the two groups(all P < 0.05). Multivariate regression analysis showed that mechanical complications(OR=6.824, P < 0.001), LAC(OR=1.125, P=0.006), Scr(OR=1.005, P=0.013), two or more vasoactive drugs(OR=5.163, P < 0.001), and invasive ventilator-assisted ventilation(OR=2.823, P=0.004) were independent risk factors for in-hospital death in patients with CS after AMI. Successful reperfusion(OR=0.19, P < 0.001) was an independent protective factor. In patients with CS after AMI, the AUC of combined index prediction model and CSP score were 0.884 and 0.733, respectively. The sensitivity and specificity of the combined index prediction model were 77.8% and 87.29%, and CSP score were 86.67% and 53.59%, respectively. The AUC of combined index prediction model, IABP-SHOCKⅡ, CSP, and IABP-SHOCK Ⅱ+CSP scores in CS patients with PCI after AMI were 0.855, 0.775, 0.743 and 0.822, respectively. The sensitivity of the combined index prediction model, IABP-SHOCK Ⅱ, CSP, and IABP-SHOCK Ⅱ+CSP scores were 85.71%, 71.43%, 93.88%, and 87.76%, while specificity were 80.67%, 74%, 52.67%, and 66%, respectively.Conclusion Mechanical complications, LAC, Scr, more than two vasoactive drugs, and invasive ventilator-assisted ventilation are independent risk factors of in-hospital death in patients with CS after AMI. Successful reperfusion is an independent protective factor. The combined index prediction model is of good value in predicting death in patients with CS after AMI, which is better than single independent influencing factor and CSP score. For CS patients with PCI after AMI, the predictive value of IABP-SHOCK Ⅱ and CSP scores is similar, while the combined index prediction model is better than IABP-SHOCK Ⅱ, CSP, and IABP-SHOCK Ⅱ+CSP scores. -

-
表 1 死亡组与存活组的一般临床资料及检验检查
Table 1. Baseline characteristics and examination results between the death and survival group
例(%), M(Q1, Q3) 项目 总体(271例) 死亡组(90例) 存活组(181例) χ2/Z值 P值 男性 163(60.1) 59(65.6) 104(57.5) 1.64 0.200 年龄/岁 66(59,72) 66(59,72) 66(58,72) 0.41 0.679 意识不清 91(33.6) 41(45.6) 50(27.6) 8.67 0.003 既往脑卒中史 52(19.2) 22(24.4) 30(16.6) 2.40 0.121 高血压病史 122(45.0) 35(38.9) 87(48.1) 2.045 0.153 糖尿病史 88(32.5) 33(36.7) 55(30.4) 1.08 0.298 冠心病史 41(15.1) 13(14.4) 28(15.5) 0.05 0.824 吸烟指数 25(0,400) 0(0,400) 80(0,400) 0.47 0.641 LVEF/% 44(37,53) 40(35,50) 44(39,53) 2.36 0.018 LVDD/mm 50(46,54) 51(46,55) 50(46,54) 1.34 0.181 机械并发症 31(11.4) 18(20.0) 13(7.2) 9.75 0.002 室速/室颤 55(20.3) 19(21.1) 36(19.9) 0.06 0.814 血糖/(mmol/L) 9.10(6.54,13.34) 9.55(6.45,14.59) 8.85(6.55,12.54) 0.71 0.479 WBC/(×109/L) 14.90(10.92,18.83) 16.86(12.20,20.52) 14.08(10.61,18.15) 2.80 0.005 NE/(×109/L) 11.78(8.21,16.07) 13.59(9.71,17.06) 11.17(7.71,15.23) 2.62 0.009 LY/(×109/L) 1.48(1.01,2.34) 1.57(0.94,2.43) 1.47(1.07,2.29) 0.27 0.787 MO/(×109/L) 0.79(0.52,1.11) 0.88(0.64,1.21) 0.73(0.46,1.03) 2.82 0.005 PLT/(×109/L) 233(189,281) 233(174,280) 232(193,282) 0.93 0.352 RBC/(×1012/L) 4.43(4.02,4.86) 4.43(3.92,4.98) 4.45(4.04,4.82) 0.45 0.653 HGB/(g/L) 136(122,151) 134(116,149) 137(123,151) 1.11 0.266 NLR 8.01(4.22,12.50) 9.03(5.12,12.76) 7.75(3.79,12.13) 1.546 0.122 pH 7.37(7.29,7.44) 7.34(7.21,7.42) 7.39(7.32,7.44) 2.82 0.005 LAC/(mmol/L) 3.8(2.0,7.3) 5.5(3.2,9.1) 2.9(1.7,5.7) 5.16 < 0.001 BE/(mmol/L) -5.8(-11.1,-2.4) -8.9(-14.3,-4.1) -5.1(-8.9,-1.8) 4.082 < 0.001 AST/(U/L) 272.3(93.6,509.6) 319.9(102.7,781.2) 253.3(92.2,517.1) 2.165 0.03 ALT/(U/L) 76.2(37.7,146.9) 96.5(38.8,305.8) 68.1(36.9,122.7) 2.75 0.006 TBIL/(μmol/L) 13.0(9.7,18.2) 14.1(10.0,20.3) 12.3(9.4,17.3) 1.92 0.055 DBIL/(μmol/L) 3.3(2.1,4.8) 3.8(2.4,6.6) 3.0(2.0,4.2) 3.25 < 0.001 ALB/(g/L) 34.7(32.1,37.7) 34.0(31.2,36.9) 35.1(32.8,37.9) 2.30 0.022 BUN/(mmol/L) 7.51(5.65,10.33) 8.90(6.41,12.49) 6.99(5.33,9.64) 3.76 < 0.001 Scr/(μmol/L) 97.3(77.0,136.6) 123.3(95.4,167.6) 89.4(71.4,118.2) 5.51 < 0.001 eGFR/(mL/min) 65.6(44.1,90.2) 51.0(32.5,73.9) 74.2(50.6,100.3) 5.07 < 0.001 cTnI/(ng/mL) 130.0(36.7,287.0) 167.0(49.9,378.3) 123.0(36.2,237.5) 1.77 0.077 BNP/(ng/mL) 319.0(56.5,1 250.0) 878.0(118.0,1 790.0) 188.0(37.6,823.5) 4.19 < 0.001 表 2 死亡组与存活组的治疗情况及CSP评分
Table 2. Treatments and CSP score between death and survival group
例(%), M(Q1, Q3) 项目 总体(271例) 死亡组(90例) 存活组(181例) 统计值 P值 IABP 82(30.3) 33(36.7) 49(27.1) 2.62 0.105 临时起搏器 19(7.0) 8(8.9) 11(6.1) 0.73 0.393 输注白蛋白 95(35.1) 31(34.4) 64(35.4) 0.02 0.882 两种以上血管活性药物 145(53.5) 73(81.1) 72(39.8) 41.2 < 0.001 CRRT 19(7.0) 14(15.6) 5(2.8) 15.09 < 0.001 成分输血 63(23.2) 27(30.0) 36(19.9) 3.45 0.063 有创呼吸机辅助通气 134(49.4) 63(70.0) 71(39.2) 22.78 < 0.001 成功再灌注 184(67.9) 42(46.7) 142(78.5) 27.86 < 0.001 CSP评分 125.8(68.3,169.9) 156.2(126.3,192.7) 89.6(55.3,153.0) 6.25 < 0.001 表 3 多因素logistic回归分析结果
Table 3. Results of multivariate logistic regression analysis
项目 β SE Wald P OR 95%CI 机械并发症 1.92 0.517 13.796 < 0.001 6.824 2.48~18.80 LAC 0.117 0.042 7.635 0.006 1.125 1.04~1.22 Scr 0.005 0.002 6.172 0.013 1.005 1.00~1.01 两种及以上血管活性药物 1.642 0.388 17.862 < 0.001 5.163 2.41~11.06 有创呼吸机辅助通气 1.038 0.364 8.141 0.004 2.823 1.38~5.76 成功再灌注 -1.659 0.351 22.265 < 0.001 0.190 0.10~0.38 表 4 相关变量的预测价值
Table 4. Predictive value of related variables
项目 灵敏度/% 特异度/% 约登指数 AUC P值 95%CI 机械并发症 20.00 92.82 0.128 0.564 0.005 9 0.503~0.624 LAC 80.00 50.28 0.303 0.693 < 0.000 1 0.634~0.747 Scr 76.67 59.12 0.358 0.706 < 0.000 1 0.647~0.759 两种以上血管活性药物 81.11 60.22 0.413 0.707 < 0.000 1 0.649~0.760 有创呼吸机辅助通气 70.00 60.77 0.308 0.654 < 0.000 1 0.594~0.710 成功再灌注 53.33 78.45 0.318 0.659 < 0.000 1 0.599~0.715 联合指标 77.78 87.29 0.650 0.884 < 0.000 1 0.839~0.919 CSP评分 86.67 53.59 0.403 0.733 < 0.000 1 0.676~0.785 表 5 联合指标与各独立因素以及CSP评分的AUC对比
Table 5. AUC comparison of combined index with independent factors and CSP scores
项目 Z值 P值 机械并发症 11.253 < 0.000 1 LAC 5.535 < 0.000 1 Scr 5.172 < 0.000 1 两种以上血管活性药物 6.995 < 0.000 1 有创呼吸机辅助通气 7.805 < 0.000 1 成功再灌注 7.197 < 0.000 1 CSP评分 5.367 < 0.000 1 表 6 PCI死亡组与PCI存活组的联合指标、IABP-SHOCKⅡ评分及CSP评分比较
Table 6. Combined index, IABP-SHOCK Ⅱ score, and CSP score in the death and survival group in patients with PCI
例(%), M(Q1, Q3) 项目 总体(199例) PCI死亡组(49例) PCI存活组(150例) Z值 P值 CSP评分 126.4(60.6,163.9) 157.4(134.6,181.5) 90.9(50.6,157.0) 5.1 < 0.001 IABP-SHOCK Ⅱ评分 2(0,3) 3(2,4) 1(0,3) 5.76 < 0.001 联合指标评分 0.16(0.02,0.41) 0.56(0.38,0.72) 0.07(0.02,0.26) 8.09 < 0.001 PCI后TIMI分级 3.8 < 0.001 0 14(7.0) 7(14.3) 7(4.7) 1 1(0.5) 0 1(0.7) 2 9(4.5) 4(8.2) 5(3.3) 3 175(87.9) 38(77.6) 137(91.5) 表 7 各预测模型在PCI患者中的预测价值
Table 7. Predictive value of predictive models in patients with PCI
项目 灵敏度/% 特异度/% 约登指数 AUC P值 95%CI IABP-SHOCK Ⅱ评分 71.43 74.00 0.454 0.775 < 0.001 0.710~0.806 CSP评分 93.88 52.67 0.465 0.743 < 0.001 0.676~0.802 IABP-SHOCK Ⅱ评分+CSP评分 87.76 66.00 0.538 0.822 < 0.001 0.761~0.872 联合指标 85.71 80.67 0.664 0.885 < 0.001 0.832~0.926 表 8 各预测模型在PCI患者中的AUC对比
Table 8. AUC comparison of predictive models in patients with PCI
项目 Z值 P值 IABP-SHOCK Ⅱ评分与CSP评分 0.606 0.5444 IABP-SHOCK Ⅱ评分+CSP评分与CSP评分 2.407 0.0161 IABP-SHOCK Ⅱ评分+CSP评分与IABP-SHOCK Ⅱ评分 2.101 0.0356 联合指标与CSP评分 4.44 < 0.0001 联合指标与IABP-SHOCK Ⅱ评分 2.439 0.0147 联合指标与IABP-SHOCK Ⅱ评分+CSP评分 1.967 0.0491 -
[1] Vahdatpour C, Collins D, Goldberg S. Cardiogenic Shock[J]. J Am Heart Assoc, 2019, 8(8): e11991.
[2] 周晓娟, 马礼坤, 魏艳, 等. 急性心肌梗死患者院内心源性休克风险列线图预测模型的构建[J]. 临床心血管病杂志, 2021, 37(5): 421-427. doi: 10.13201/j.issn.1001-1439.2021.05.007
[3] Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic Shock After Acute Myocardial Infarction: A Review[J]. JAMA, 2021, 326(18): 1840-1850. doi: 10.1001/jama.2021.18323
[4] Thiele H, Ohman EM, de Waha-Thiele S, et al. Management of cardiogenic shock complicating myocardial infarction: an update 2019[J]. Eur Heart J, 2019, 40(32): 2671-2683. doi: 10.1093/eurheartj/ehz363
[5] Bertini P, Guarracino F. Pathophysiology of cardiogenic shock[J]. Curr Opin Crit Care, 2021, 27(4): 409-415. doi: 10.1097/MCC.0000000000000853
[6] 魏宇淼. 急性心肌梗死并发心源性休克的当代治疗策略及技术[J]. 临床心血管病杂志, 2021, 37(7): 591-594. doi: 10.13201/j.issn.1001-1439.2021.07.001
[7] Poss J, Koster J, Fuernau G, et al. Risk Stratification for Patients in Cardiogenic Shock After Acute Myocardial Infarction[J]. J Am Coll Cardiol, 2017, 69(15): 1913-1920. doi: 10.1016/j.jacc.2017.02.027
[8] 罗晓亮, 赵彤, 李佳, 等. 主动脉内球囊反搏-休克Ⅱ风险评分对国人急性心肌梗死合并心原性休克患者30天死亡率的预测价值[J]. 中国循环杂志, 2018, 33(6): 535-538. doi: 10.3969/j.issn.1000-3614.2018.06.004
[9] 孙小强, 王保强, 陈建昌. IABP-SHOCKⅡ危险评分在老年急性心肌梗死合并心源性休克患者病情评估及院内死亡评估中的应用价值[J]. 中国老年学杂志, 2022, 42(6): 1288-1291. doi: 10.3969/j.issn.1005-9202.2022.06.003
[10] Tien YT, Chen WJ, Huang CH, et al. The CSP(Cardiogenic Shock Prognosis)Score: A Tool for Risk Stratification of Cardiogenic Shock[J]. Front Cardiovasc Med, 2022, 9: 842056. doi: 10.3389/fcvm.2022.842056
[11] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction(2018)[J]. J Am Coll Cardiol, 2018, 72(18): 2231-2264. doi: 10.1016/j.jacc.2018.08.1038
[12] Fuernau G, Desch S, de Waha-Thiele S, et al. Arterial Lactate in Cardiogenic Shock: Prognostic Value of Clearance Versus Single Values[J]. JACC Cardiovasc Interv, 2020, 13(19): 2208-2216. doi: 10.1016/j.jcin.2020.06.037
[13] Lindholm MG, Hongisto M, Lassus J, et al. Serum Lactate and A Relative Change in Lactate as Predictors of Mortality in Patients With Cardiogenic Shock-Results from the Cardshock Study[J]. Shock, 2020, 53(1): 43-49. doi: 10.1097/SHK.0000000000001353
[14] Muzafarova T, Motovska Z. Laboratory Predictors of Prognosis in Cardiogenic Shock Complicating Acute Myocardial Infarction[J]. Biomedicines, 2022, 10(6): 1328. doi: 10.3390/biomedicines10061328
[15] Ceglarek U, Schellong P, Rosolowski M, et al. The novel cystatin C, lactate, interleukin-6, and N-terminal pro-B-type natriuretic peptide(CLIP)-based mortality risk score in cardiogenic shock after acute myocardial infarction[J]. Eur Heart J, 2021, 42(24): 2344-2352. doi: 10.1093/eurheartj/ehab110
[16] Ghionzoli N, Sciaccaluga C, Mandoli GE, et al. Cardiogenic shock and acute kidney injury: the rule rather than the exception[J]. Heart Fail Rev, 2021, 26(3): 487-496. doi: 10.1007/s10741-020-10034-0
[17] Puerto E, Viana-Tejedor A, Martinez-Selles M, et al. Temporal Trends in Mechanical Complications of Acute Myocardial Infarction in the Elderly[J]. J Am Coll Cardiol, 2018, 72(9): 959-966. doi: 10.1016/j.jacc.2018.06.031
[18] Elbadawi A, Elgendy IY, Mahmoud K, et al. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction[J]. JACC Cardiovasc Interv, 2019, 12(18): 1825-1836. doi: 10.1016/j.jcin.2019.04.039
[19] Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation[J]. Eur Heart J, 2021, 42(14): 1289-1367. doi: 10.1093/eurheartj/ehaa575
[20] Thiele H, de Waha-Thiele S, Freund A, et al. Management of cardiogenic shock[J]. EuroIntervention, 2021, 17(6): 451-465. doi: 10.4244/EIJ-D-20-01296
[21] Uhlig K, Efremov L, Tongers J, et al. Inotropic agents and vasodilator strategies for the treatment of cardiogenic shock or low cardiac output syndrome[J]. Cochrane Database Syst Rev, 2020, 11(11): D9669.
[22] Thiele H, Zeymer U, Neumann FJ, et al. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock(IABP-SHOCK Ⅱ): final 12 month results of a randomised, open-label trial[J]. Lancet, 2013, 382(9905): 1638-1645. doi: 10.1016/S0140-6736(13)61783-3
[23] Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock[J]. N Engl J Med, 2012, 367(14): 1287-1296. doi: 10.1056/NEJMoa1208410
[24] Thiele H, Zeymer U, Thelemann N, et al. Intraaortic Balloon Pump in Cardiogenic Shock Complicating Acute Myocardial Infarction: Long-Term 6-Year Outcome of the Randomized IABP-SHOCK Ⅱ Trial[J]. Circulation, 2019, 139(3): 395-403. doi: 10.1161/CIRCULATIONAHA.118.038201
[25] Rossini R, Valente S, Colivicchi F, et al. ANMCO POSITION PAPER: Role of intra-aortic balloon pump in patients with acute advanced heart failure and cardiogenic shock[J]. Eur Heart J Suppl, 2021, 23(Suppl C): C204-C220.
[26] Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2018, 39(2): 119-177. doi: 10.1093/eurheartj/ehx393
[27] Yang JH, Choi KH, Ko YG, et al. Clinical Characteristics and Predictors of In-Hospital Mortality in Patients With Cardiogenic Shock: Results From the RESCUE Registry[J]. Circ Heart Fail, 2021, 14(6): e8141.
[28] 周生辉, 柳子静, 李紫旋, 等. 急性心肌梗死合并心源性休克患者行急诊经皮冠状动脉介入治疗院内死亡危险因素[J]. 中国心血管病研究, 2022, 20(7): 602-607. https://www.cnki.com.cn/Article/CJFDTOTAL-XXGZ202207003.htm
[29] Hongisto M, Lassus J, Tarvasmaki T, et al. Use of noninvasive and invasive mechanical ventilation in cardiogenic shock: A prospective multicenter study[J]. Int J Cardiol, 2017, 230: 191-197. doi: 10.1016/j.ijcard.2016.12.175
-




 下载:
下载: