Correlation between red blood cell distribution and layered plaques in patients with acute coronary syndrome
-
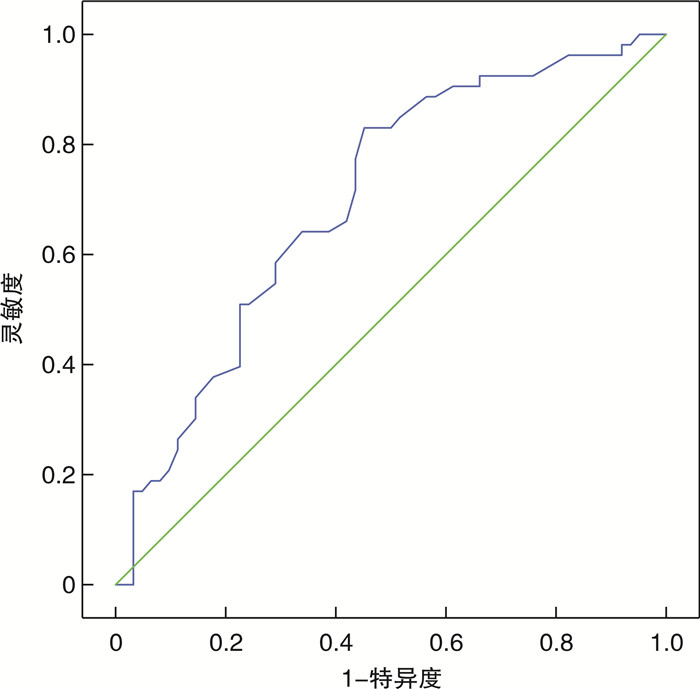
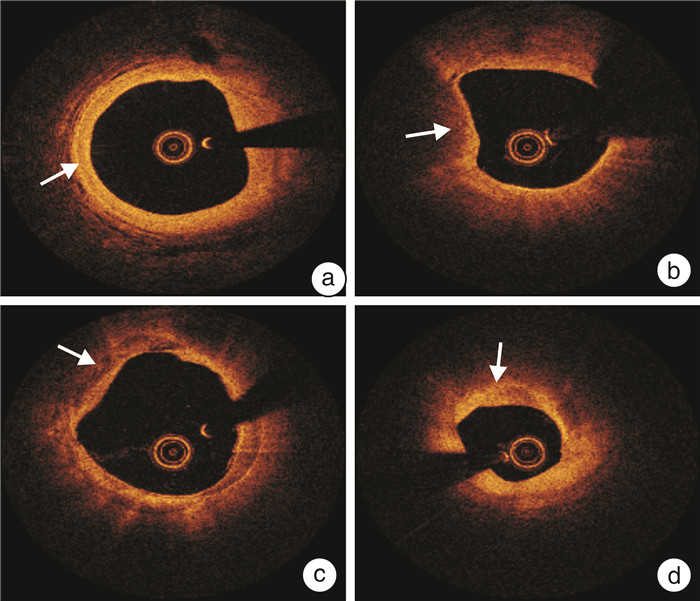
摘要: 目的 基于光学相干断层成像技术(OCT)探讨红细胞分布宽度(RDW)与急性冠状动脉综合征(ACS)患者冠状动脉(冠脉)分层斑块的相关性。方法 选取2020年1月—2023年1月于新疆医科大学第一附属医院行冠脉造影(CAG)和造影后即刻对罪犯血管行OCT检查并确诊为ACS的患者140例为研究对象。根据OCT图像结果,将患者分为分层斑块组66例和非分层斑块组74例。比较两组基线资料、实验室数据以及OCT图像。采用Spearman检验分析RDW水平与斑块破裂、薄纤维帽粥样硬化斑块(TCFA)的相关性。采用单因素及多因素logistic回归分析筛选分层斑块的危险因素。采用受试者工作特征(ROC)曲线评估RDW对冠脉分层斑块的诊断效能。结果 与非分层斑块组比较,分层斑块组高密度脂蛋白胆固醇(HDL-C)水平显著降低[(1.01±0.21) mmol/L vs (0.89±0.25) mmol/L,P=0.006],RDW水平显著升高[(12.52±0.55)% vs (13.30±1.04),P < 0.001]。OCT检查结果显示,分层斑块组巨噬细胞分级、钙化小结检出率(13.6% vs 4.1%)、血栓率(19.7% vs 5.4%)、狭窄率(80% vs 75%)均显著高于非分层斑块组(均P < 0.05)。相关性分析显示,RDW与TCFA、斑块破裂均呈正相关(r=0.565、0.430,均P < 0.001)。多因素logistic回归分析显示,男性(OR=5.000,95%CI:1.557~16.052,P=0.007)、RDW(OR=5.601,95%CI:2.738~11.458,P=0.001)、HDL-C(OR=27.565,95%CI:3.800~199.941,P=0.001)是ACS患者罪犯血管存在分层斑块的独立危险因素。ROC曲线分析发现,RDW 13.05%是预测罪犯血管分层斑块的临界值,灵敏度和特异度分别为49.1%和83.9%。结论 分层斑块与斑块易损特征相关。RDW与斑块破裂、TCFA存在相关性,是ACS患者罪犯血管分层斑块的独立危险因素。Abstract: Objective To analyze the correlation between red blood cell distribution width (RDW) levels and coronary layered plaques in patients with acute coronary syndrome (ACS) utilizing optical coherence tomography (OCT).Methods A total of 140 patients who underwent coronary angiography (CAG) and immediate OCT assessment of culprit vessels following CAG, and were subsequently diagnosed with ACS at the First Affiliated Hospital of Xinjiang Medical University between January 2020 and January 2023, were included. Based on OCT image findings, the patients were categorized into a layered plaque group (66 cases) and a non-layered plaque group (74 cases). Comparative analysis encompassed baseline characteristics, laboratory data, and OCT images. Spearman analysis was performed to explore the correlation between RDW and plaque rupture as well as thin-cap fibroatheroma (TCFA). Univariate and multivariate logistic regression analysis were conducted to identify risk factors associated with layered plaque. Receiver operating characteristic (ROC) curves were generated to evaluate the diagnostic utility of RDW in identifying layered plaques.Results In comparation with the non-layered plaque group, the layered plaque group exhibited a significantly reduction in high-density lipoprotein cholesterol (HDL-C) levels [(1.01 ± 0.21) mmol/L vs (0.89 ± 0.25) mmol/L, P=0.006], accompanied by a noteworthy elevation in RDW levels [(12.52 ± 0.55)% vs (13.30 ± 1.04), P < 0.001]. OCT findings demonstrated heightened macrophage grading, elevated rates of calcified nodule detection (13.6% vs 4.1%), thrombus formation(19.7% vs 5.4%), and increased stenosis frequency (80% vs 75%) in the layered plaque group compared to the non-layered plaque group (P < 0.05). Correlation analysis showed that RDW was positively associated with TCFA (r=0.565, P < 0.001), and plaque rupture (r=0.430, P < 0.001). Multivariate logistic regression analysis highlighted male gender (OR=5.000, 95%CI: 1.557 - 16.052, P=0.007), RDW (OR=5.601, 95%CI: 2.738 - 11.458, P=0.001), and HDL-C (OR=27.565, 95%CI: 3.800 - 199.941, P=0.001) were independent risk factors for layered plaques in culprit vessels in ACS patients. ROC curve analysis found RDW=13.05% was the cutoff point for predicting layered plaques in culprit vessels, displaying a sensitivity of 49.1% and specificity of 83.9%.Conclusion Layered plaques exhibit an association with plaque vulnerability. RDW demonstrates correlations with plaque rupture and TCFA, emerging as an independent risk determinant for layered plaques within lesioned vessels among patients afflicted with ACS.
-

-
表 1 非分层斑块组和分层斑块组基线特征比较
Table 1. Comparison of baseline characteristics between the non-layered and layered plaque groups
例(%), X±S 项目 非分层斑块组(74例) 分层斑块组(66例) P值 年龄/岁 59.73±10.06 59.77±11.98 0.928 男性 55(74.3) 54(81.8) 0.286 高血压 43(58.1) 42(63.6) 0.504 2型糖尿病 20(27.0) 16(24.2) 0.707 冠心病家族史 18(24.3) 15(22.7) 0.790 饮酒史 19(25.7) 24(36.4) 0.171 吸烟史 35(47.3) 31(47.0) 0.969 BMI/(kg/m2) 26.41±3.60 26.50±2.69 0.860 治疗用药 阿司匹林 73(98.4) 66(100.0) 0.999 P2Y12受体拮抗剂 26(35.1) 23(34.9) 0.890 他汀类 72(97.3) 66(100.0) 0.527 β受体阻滞剂 60(81.1) 52(78.8) 0.735 ACEI/ARB 41(55.4) 38(57.6) 0.796 CCB 28(37.8) 33(50.0) 0.147 临床诊断 0.331 不稳定型心绞痛 60(81.1) 49(74.2) 急性心肌梗死 14(18.9) 17(25.8) 病变血管 0.271 前降支 48(64.9) 48(72.7) 回旋支 18(24.3) 9(13.6) 右冠脉 8(10.8) 9(13.6) 病变血管支数 0.979 1支 36(48.6) 33(50.0) 2支 19(25.7) 17(25.8) 3支 19(25.7) 16(24.2) 病变位置 0.785 近段 48(64.9) 44(66.7) 中段 21(28.4) 16(24.2) 远段 5(6.7) 6(9.1) EF/% 59.23±8.15 58.71±7.74 0.548 ACEI/ARB:血管紧张素转化酶抑制剂/血管紧张素Ⅱ受体拮抗剂;CCB:钙通道阻滞剂。 表 2 非分层斑块组和分层斑块组临床生化指标比较
Table 2. Comparison of biochemical indicators between the non-layered and layered plaque groups
X±S, M(P25, P75) 项目 非分层斑块组(74例) 分层斑块组(66例) P值 白细胞计数/(×109/L) 6.96±1.89 7.40±1.99 0.181 红细胞计数/(×1012/L) 4.55±0.62 4.64±0.57 0.401 血小板计数/(×109/L) 234.651±58.39 240.83±69.09 0.399 RDW/% 12.52±0.55 13.30±1.04 <0.001 血红蛋白/(g/L) 139.24±17.44 140.08±15.77 0.768 白蛋白/(g/L) 41.93±3.31 43.17±4.30 0.056 纤维蛋白原/(g/L) 0.72(0.45,1.64) 0.66(0.42,1.31) 0.478 D-二聚体/(mg/L) 85.50(54.25,153.50) 83.50(52.75,138.50) 0.522 尿素氮/(mmol/L) 5.79±2.77 5.79±1.42 0.991 肌酐/(μmol/L) 82.29±26.01 75.00±23.55 0.549 eGFR/(mL/min/1.73m2) 93.61±15.44 95.65±18.81 0.483 总胆红素/(μmol/L) 12.82±4.05 13.68±5.33 0.288 AST/(U/L) 27.93(17.48,39.11) 26.36(13.69,39.37) 0.799 ALT/(U/L) 25.52(19.98,32,32) 26.67(18.86,34.27) 0.910 TG/(mmol/L) 1.52(1.13,2.34) 1.65(1.14,2.45) 0.634 TC/(mmol/L) 3.59±1.02 3.71±1.12 0.516 HDL-C/(mmol/L) 1.01±0.21 0.89±0.25 0.006 LDL-C/(mmol/L) 2.15±0.83 2.26±1.30 0.548 NT-proBNP/(pg/L) 149.50(52.50,243.00) 158.50(56.50,250.00) 0.625 AST:谷草转氨酶;ALT:谷丙转氨酶。 表 3 非分层斑块组和分层斑块组OCT参数比较
Table 3. Comparison of OCT parameters between the non-layered plaque and layered plaque groups
例(%), X±S, M(P25, P75) 项目 非分层斑块组(74例) 分层斑块组(66例) P值 脂质弧/° 139.00(109.75,185.0) 146.00(92.75,198.50) 0.815 纤维帽厚度/μm 120.00(60.00,212.50) 100.00(50.00,192.50) 0.229 TCFA 25(33.8) 25(37.9) 0.492 斑块破裂 5(6.8) 8(12.1) 0.275 斑块侵蚀 8(10.8) 5(7.6) 0.510 巨噬细胞分级 0.026 0级 38(51.4) 19(28.8) 1级 26(35.1) 33(50.0) 2级 9(12.2) 10(15.2) 3级 1(1.3) 4(6.0) 4级 0(0) 0(0) 胆固醇结晶 30(40.5) 37(56.1) 0.066 滋养血管 28(37.8) 33(50.0) 0.147 血栓 4(5.4) 13(19.7) 0.010 钙化小结 3(4.1) 9(13.6) 0.034 斑块类型 0.322 纤维斑块 24(32.4) 18(27.3) 脂质斑块 45(60.8) 39(59.1) 钙化斑块 5(6.8) 9(13.6) 最小管腔面积/mm2 2.11±0.75 1.88±0.70 0.176 正常管腔面积/mm2 8.14±2.36 7.71±2.12 0.371 狭窄率/% 75(60,90) 80(70,95) 0.021 表 4 分层斑块的多因素logistic回归分析
Table 4. Multivariate logistic regression analysis of layered plaques
变量 B SE Wals P OR 95%CI 性别 1.609 0.595 7.314 0.007 5.000 1.557~16.052 年龄 -0.024 0.020 1.424 0.233 0.976 0.938~1.016 BMI -0.005 0.066 0.005 0.942 0.995 0.874~1.144 HDL-C 3.317 1.011 10.762 0.001 27.565 3.800~199.941 RDW 1.723 0.365 22.268 0.001 5.601 2.738~11.458 表 5 RDW与斑块易损性的相关性分析
Table 5. Correlation analysis
变量 RDW r P TCFA 0.565 <0.001 斑块破裂 0.430 <0.001 斑块侵蚀 0.030 0.100 -
[1] Fracassi F, Crea F, Sugiyama T, et al. Healed Culprit Plaques in Patients With Acute Coronary Syndromes[J]. J Am Coll Cardiol, 2019, 73(18): 2253-2263. doi: 10.1016/j.jacc.2018.10.093
[2] Burke AP, Kolodgie FD, Farb A, et al. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression[J]. Circulation, 2001, 103(7): 934-940. doi: 10.1161/01.CIR.103.7.934
[3] Kurihara O, Russo M, Kim HO, et al. Clinical significance of healed plaque detected by optical coherence tomography: a 2-year follow-up study[J]. J Thromb Thrombolysis, 2020, 50(4): 895-902. doi: 10.1007/s11239-020-02076-w
[4] Salvagno GL, Sanchis-Gomar F, Picanza A, et al. Red blood cell distribution width: A simple parameter with multiple clinical applications[J]. Crit Rev Clin Lab Sci, 2015, 52(2): 86-105. doi: 10.3109/10408363.2014.992064
[5] Jin P, Wu SJ, Ma Q, et al. The Relation Between Red Blood Cell Distribution Width and Coronary Atherosclerotic Plaque Vulnerability Detected by Intracoronary Optical Coherence Tomography[J]. Curr Vasc Pharmacol, 2022, 20(6): 501-507. doi: 10.2174/1570161120666220527093551
[6] Ma FL, Li S, Li XL, et al. Correlation of red cell distribution width with the severity of coronary artery disease: a large Chinese cohort study from a single center[J]. Chin Med J(Engl), 2013, 126(6): 1053-1057.
[7] Moriarty PM, Steg PG, McGinniss J, et al. Relation of red blood cell distribution width to risk of major adverse cardiovascular events, death, and effect of alirocumab after acute coronary syndromes[J]. J Clin Lipidol, 2022, 16(5): 747-756. . doi: 10.1016/j.jacl.2022.08.004
[8] Ziada KM, Misumida N. In Vivo Identification of Healed Plaques in Culprit Lesions: Is What We're Seeing Really There?[J]. J Am Coll Cardiol, 2019, 73(18): 2264-2266. doi: 10.1016/j.jacc.2019.03.023
[9] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 非ST段抬高型急性冠状动脉综合征诊断和治疗指南(2016)[J]. 中华心血管病杂志, 2017, 45(5): 359-376. doi: 10.3760/cma.j.issn.0253-3758.2017.05.003
[10] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019(10): 766-783. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXB201709002.htm
[11] Prati F, Regar E, Mintz GS, et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis[J]. Eur Heart J, 2010, 31(4): 401-415. doi: 10.1093/eurheartj/ehp433
[12] Tearney GJ, Regar E, Akasaka T, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation[J]. J Am Coll Cardiol, 2012, 59(12): 1058-1072. doi: 10.1016/j.jacc.2011.09.079
[13] Shimokado A, Matsuo Y, Kubo T, et al. In vivo optical coherence tomography imaging and histopathology of healed coronary plaques[J]. Atherosclerosis, 2018, 275: 35-42. doi: 10.1016/j.atherosclerosis.2018.05.025
[14] Dai JN, Fang C, Zhang ST, et al. Frequency, Predictors, Distribution, and Morphological Characteristics of Layered Culprit and Nonculprit Plaques of Patients With Acute Myocardial Infarction: In Vivo 3-Vessel Optical Coherence Tomography Study[J]. Circ Cardiovasc Interv, 2020, 13(10): e009125.
[15] Mann J, Davies MJ. Mechanisms of progression in native coronary artery disease: role of healed plaque disruption[J]. Heart, 1999, 82(3): 265-268. doi: 10.1136/hrt.82.3.265
[16] Kimura S, Cho S, Misu Y, et al. Optical coherence tomography and coronary angioscopy assessment of healed coronary plaque components[J]. Int J Cardiovasc Imaging, 2021, 37(10): 2849-2859. doi: 10.1007/s10554-021-02287-z
[17] Russo M, Kim HO, Kurihara O, et al. Characteristics of non-culprit plaques in acute coronary syndrome patients with layered culprit plaque[J]. Eur Heart J Cardiovasc Imaging, 2020, 21(12): 1421-1430. doi: 10.1093/ehjci/jez308
[18] Russo M, Fracassi F, Kurihara O, et al. Healed Plaques in Patients With Stable Angina Pectoris[J]. Arterioscler Thromb Vasc Biol, 2020, 40(6): 1587-1597. doi: 10.1161/ATVBAHA.120.314298
[19] Kurihara O, Shinohara H, Kim HO, et al. Comparison of post-stent optical coherence tomography findings: Layered versus non-layered culprit lesions[J]. Catheter Cardiovasc Interv, 2021, 97(7): 1320-1328. doi: 10.1002/ccd.28940
[20] Crea F, Libby P. Acute Coronary Syndromes: The Way Forward From Mechanisms to Precision Treatment[J]. Circulation, 2017, 136(12): 1155-1166. doi: 10.1161/CIRCULATIONAHA.117.029870
[21] 韩娟, 华文龙. 红细胞分布宽度/血小板计数对多发性骨髓瘤预后预测价值的研究[J]. 临床血液学杂志, 2022, 35(2): 121-126. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202202009.htm
[22] Pan J, Borné Y, Gonçalves I, et al. Associations of Red Cell Distribution Width With Coronary Artery Calcium in the General Population[J]. Angiology, 2022, 73(5): 445-452. doi: 10.1177/00033197211052124
[23] Li N, Zhou H, Tang Q. Red Blood Cell Distribution Width: A Novel Predictive Indicator for Cardiovascular and Cerebrovascular Diseases[J]. Dis Markers, 2017, 2017: 7089493.
[24] 张林, 陈玥, 张宝红. 血小板-淋巴细胞比率、中性粒细胞-淋巴细胞比率及红细胞分布宽度在冠心病严重程度中的诊断价值[J]. 临床心血管病杂志, 2020, 36(9): 824-827. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2020.09.010
[25] Bujak K, Wasilewski J, Osadnik T, et al. The Prognostic Role of Red Blood Cell Distribution Width in Coronary Artery Disease: A Review of the Pathophysiology[J]. Dis Markers, 2015: 824624.
[26] Inuzuka R, Abe J. Red blood cell distribution width as a link between ineffective erythropoiesis and chronic inflammation in heart failure[J]. Circ J, 2015, 79(5): 974-975. doi: 10.1253/circj.CJ-15-0254
[27] Montagnana M, Cervellin G, Meschi T, et al. The role of red blood cell distribution width in cardiovascular and thrombotic disorders[J]. Clin Chem Lab Med, 2011, 50(4): 635-641.
-




 下载:
下载: