Effect of immediate interventional therapy on prognosis of middle-and high-risk non-ST-segment elevation myocardial infarction patients
-
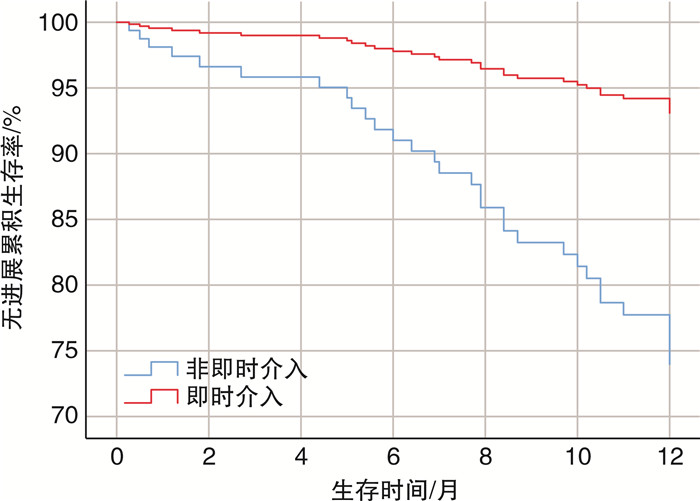
摘要: 目的 探讨即时介入治疗与非即时介入治疗对GRACE评分中高危的非ST段抬高型心肌梗死(non-ST-segment elevation myocardial infarction,NSTEMI)患者临床结局的影响。方法 回顾性分析2019年1月—2021年2月于同济大学附属东方医院心内科住院行介入治疗(D to B时间在72 h内)、GRACE评分中高危且资料完整的NSTEMI患者130例。依据D to B时间将患者分为即时介入组(D to B时间≤2 h,39例)和非即时介入组(D to B时间2~72 h,91例)。收集并比较两组患者住院期间的临床资料、实验室指标、影像学结果、治疗情况,以及随访1年的主要不良心血管事件(MACE)情况。采用Cox回归分析MACE发生的影响因素。结果 即时介入组MACE事件发生率(29.6% vs 7.7%)和再发心肌梗死率(16.5% vs 2.6%)均显著低于非即时介入组(P < 0.05)。Cox分析显示,即时介入(HR=0.233,P < 0.05)、年龄(HR=1.043,P < 0.05)和肌酐(HR=1.007,P < 0.05)是MACE发生的影响因素。结论 即时介入能显著降低NSTEMI患者MACE的发生风险,且延长无MACE生存时间。
-
关键词:
- 非ST段抬高型心肌梗死 /
- 即时介入 /
- 危险因素 /
- 预后
Abstract: Objective To investigate the effects of immediate intervention and indirect intervention on clinical outcomes in patients with high-risk non-ST-segment elevation myocardial infarction (NSTEMI) based on the Global Registry of Acute Coronary Events (GRACE) score.Methods A retrospective analysis was conducted on a cohort of 130 NSTEMI patients admitted to the Department of Cardiology, Dongfang Hospital, Affiliated to Tongji University, between January 2019 and February 2021. All enrolled patients underwent interventional therapy (D to B time within 72 hours) and exhibited high-risk profiles according to the GRACE score, with complete datasets available. Patients were divided into two groups: the immediate intervention group (D to B time ≤ 2 h, n=39) and the indirect intervention group (D to B time 2-72 h, n=91), based on their D to B time. Clinical data, laboratory indicators, imaging findings, in-hospital treatments, and major adverse cardiac events (MACE) during a one-year follow-up were meticulously documented and compared between the two groups. Cox regression analysis was employed to elucidate the risk factors associated with MACE.Results The incidence of MACE (29.6% vs 7.7%) and recurrent myocardial infarction (16.5% vs 2.6%) in the immediate intervention group were significantly lower than those in the non-immediate intervention group (both P < 0.05). Cox regression analysis revealed that immediate intervention (HR=0.233, P < 0.05), age (HR=1.043, P < 0.05), and serum creatinine (HR=1.007, P < 0.05) were risk factors of MACE.Conclusion Immediate intervention is associated with a substantial reduction the risk of MACE occurrence and extended MACE-free survival in patients with NSTEMI. -

-
表 1 两组一般资料比较
Table 1. General data
例(%), X±S 项目 非即时介入组(91例) 即时介入组(39例) χ2/t P 年龄/岁 80.29±15.24 75.36±14.70 -1.678 0.090 男性 65(71.43) 31(66.67) 0.918 0.338 BMI/(kg/m2) 25.00±3.17 24.80±3.27 -0.329 0.743 心率/(次/min) 80.29±15.24 75.36±14.70 1.707 0.090 收缩压/mmHg 140.47±22.52 136.74±25.64 0.829 0.408 高血压 61(67.03) 26(66.67) 0.002 0.968 糖尿病 35(38.46) 7(17.95) 5.253 0.022 吸烟史 49(53.85) 28(71.79) 3.642 0.056 脑卒中 4(4.40) 4(10.26) 1.624 0.203 冠心病 20(21.98) 3(7.69) 3.826 0.049 陈旧性心肌梗死 15(16.48) 3(7.69) 1.769 0.184 PCI史 15(16.48) 3(7.69) 1.769 0.184 CABG史 4(4.40) 0 0.512 心房颤动史 2(2.20) 1(2.56) 0.016 0.899 新发心房颤动史 5(5.49) 1(2.56) 0.533 0.466 尿毒症史 1(1.10) 1(2.56) 0.512 饮酒史 25(27.47) 11(28.21) 0.007 0.932 Killip分级 0.391 Ⅰ级 57(62.64) 28(71.79) Ⅱ级 29(31.87) 11(28.21) Ⅲ级 5(5.49) 0 GRACE评分 2.103 0.147 中危 32(35.16) 19(48.72) 高危 59(64.84) 20(51.28) 1 mmHg=0.133 kPa;CABG:冠脉旁路移植术。 表 2 两组实验室资料比较
Table 2. Laboratory indicators
例(%), X±S, M(P25, P75) 项目 非即时介入组(91例) 即时介入组(39例) χ2/t/Z P cTnT/(ng/mL) 0.38(0.15,1.02) 0.67(0.41,2.17) -2.624 0.009 Myo/(ng/mL) 74.43(34.38,201.15) 121.2(39.64,293.75) -1.288 0.198 CK-MB/(ng/mL) 14.00(5.73,48.10) 31.50(9.89,115.15) -2.228 0.026 NT-proBNP/(ng/mL) 455.1(141.9,1758.5) 471.6(255.5,1065.0) -0.404 0.686 HbA1c/% 6.69±1.37 6.39±1.30 -1.158 0.249 ALB/(g/L) 40.00±4.43 40.59±3.48 0.739 0.461 ALT/(U/L) 25.00(17.25,35.95) 26.00(18.90,40.50) -0.836 0.403 AST/(U/L) 43.00(24.50,66.75) 60.00(29.00,113.50) -2.157 0.031 TC/(mmol/L) 4.25(3.52,5.16) 4.19(3.68,4.63) -0.986 0.324 TG/(mmol/L) 1.38(1.07,2.10) 1.70(1.22,1.97) -1.313 0.189 HDL-C/(mmol/L) 1.10(0.92,1.24) 0.98(0.85,1.10) -2.604 0.009 LDL-C/(mmol/L) 2.80(1.98,3.60) 2.68(2.28,3.20) -0.851 0.395 Cr/(μmol/L) 73.40(63.10,89.45) 75.00(67.50,88.85) -0.798 0.425 BUN/(mmol/L) 5.65(4.90,6.55) 5.46(4.18,6.68) -0.643 0.520 PT/s 11.68±0.91 11.74±1.22 0.313 0.755 APTT/s 28.53±4.22 28.69±3.71 0.215 0.830 Fib/(g/L) 2.88(2.46,3.34) 3.13(2.63,3.49) -1.364 0.173 FDP/(mg/L) 2.50(2.50,2.69) 2.50(1.77,2.50) -1.645 0.100 D二聚体/(mg/L) 0.29(0.22,0.61) 0.38(0.23,0.55) -0.812 0.417 LVEF/% 57.54±9.10 57.59±7.06 0.031 0.975 C反应蛋白/(mg/L) 2.65(1.60,9.06) 4.50(1.77,12.16) -1.803 0.071 白细胞计数/(×109/L) 8.48±2.40 8.87±2.10 0.878 0.381 中性粒细胞百分比/% 70.56±9.44 72.65±8.49 1.192 0.235 淋巴细胞百分比/% 21.40(15.60,25.89) 17.80(13.85,21.90) -2.276 0.023 中性粒细胞计数/(×109/L) 6.20±2.50 6.53±1.88 0.74 0.461 淋巴细胞计数/(×109/L) 1.56(1.27,2.06) 1.51(1.15,2.10) -0.765 0.444 红细胞计数/(×1012/L) 4.39±0.62 4.50±0.56 0.925 0.357 血红蛋白/(g/L) 136.89±18.23 139.92±18.44 0.866 0.388 红细胞压积/% 41.11±5.20 40.36±7.05 -0.676 0.500 血小板/(×109/L) 199.92±55.18 201.82±48.04 0.187 0.852 PT: 凝血酶原时间; APTT: 活化部分凝血活酶时间; Fib: 纤维蛋白原; FDP: 纤维蛋白降解产物。 表 3 两组造影及治疗资料比较
Table 3. Coronary angiography and treatment data
例(%), X±S 项目 非即时介入组(91例) 即时介入组(39例) χ2/t P 冠脉病变支数 2.39 0.303 单支 13(14.29) 8(20.51) 双支 25(27.47) 14(35.90) 3支 53(58.24) 17(43.59) 阿司匹林+氯吡格雷 29(31.87) 12(30.77) 0.015 0.902 阿司匹林+替格瑞洛 57(62.64) 23(58.97) 0.155 0.694 阿司匹林+西洛他唑 3(3.30) 4(10.26) 0.196 单药抗血小板 2(2.20) 0 1.000 β受体阻滞剂 73(80.22) 29(74.36) 0.555 0.456 ACEI/ARB 66(72.53) 28(71.79) 0.007 0.932 他汀类 90(98.90) 39(100.00) 1.000 抗凝药物 5(5.49) 1(2.56) 0.668 此次平均植入支架数/枚 1 1 -1.128 0.259 平均住院天数/d 7 7 1.458 0.145 计划内再次择期干预 15(16.48) 19(48.72) 14.687 < 0.001 罪犯血管TIMI分级 14.189 0.003 0 76(83.52) 20(51.28) Ⅰ 3(3.30) 1(2.56) Ⅱ 25(27.47) 5(12.82) Ⅲ 44(48.35) 12(30.77) PCI 81(89.01) 34(87.18) 0.09 0.765 PTCA 91(100.00) 39(100.00) 1.000 CABG 5(5.49) 0 0.321 IVUS 3(3.30) 6(15.38) 0.021 IABP 0 0 1.000 ACEI/ARB: 血管紧张素转化酶抑制剂/血管紧张素Ⅱ受体拮抗剂; IABP: 主动脉内球囊反搏。 表 4 两组MACE发生率比较
Table 4. The incidence of MACE
例(%) 项目 非即时介入组(91例) 即时介入组(39例) P MACE 27(29.7) 3(7.7) 0.006 死亡 1(1.1) 0 1 再发心肌梗死 15(16.5) 1(2.6) 0.038 脑卒中 5(5.5) 0 0.321 再次血运重建 0 1(2.6) 0.300 心力衰竭 6(6.6) 1(2.6) 0.434 表 5 单因素Cox回归分析结果
Table 5. The result of univariate Cox regression analysis
项目 B SE Wald χ2 P HR 95%CI 性别 -0.844 0.369 5.247 0.022 0.430 0.029~0.885 年龄 0.043 0.017 6.719 0.010 1.044 1.011~1.079 心率 0.028 0.010 6.968 0.008 1.028 1.007~1.049 Killip分级 Ⅱ -0.339 0.439 0.594 0.441 0.713 0.310~1.686 Ⅲ 1.234 0.622 3.938 0.047 3.434 1.015~11.616 cTnT 0.050 0.113 0.197 0.657 1.051 0.843~1.312 TC -0.071 0.168 0.177 0.674 0.932 0.670~1.295 LDL-C 0.020 0.179 0.013 0.910 1.021 0.718~1.450 Cr 0.004 0.001 12.745 < 0.001 1.004 1.002~1.007 BUN 0.127 0.048 6.879 0.009 1.135 1.033~1.248 干预时机 0.609 5.422 0.020 0.242 0.073~0.799 其中性别以女性为参照,Killip分级以Ⅰ级为参照,干预时机以非即时介入为参照。下同。 表 6 多因素Cox回归分析
Table 6. The result of multivariate Cox regression analysis
项目 B SE Wald χ2 P HR 95%CI 性别 -0.462 0.425 1.183 0.277 0.630 0.274~1.448 年龄 0.042 0.019 4.674 0.031 1.043 1.004~1.083 心率 0.018 0.012 2.492 0.114 1.019 0.996~1.042 Killip分级 Ⅱ -0.669 0.467 2.048 0.152 0.512 0.205~1.280 Ⅲ 0.328 0.751 0.191 0.662 1.388 0.318~6.054 Cr 0.007 0.002 9.103 0.003 1.007 1.002~1.012 BUN -0.053 0.090 0.341 0.559 0.949 0.794~1.133 干预时机 -1.456 0.722 4.063 0.044 0.233 0.057~0.961 表 7 无MACE生存时间比较
Table 7. MACE-free survival time
组别 平均生存时间/月 95%CI χ2 P 即时介入组(39例) 11.78 10.88~12.67 6.421 0.011 非即时介入组(91例) 10.64 10.06~11.22 总体(130例) 11.27 10.76~11.78 -
[1] Bhatt DL, Lopes RD, Harrington RA. Diagnosis and Treatment of Acute Coronary Syndromes: A Review[J]. JAMA, 2022, 327(7): 662-675. doi: 10.1001/jama.2022.0358
[2] Jobs A, Thiele H, European Society of Cardiology. ESC guidelines 2015. Non-ST-elevation acute coronary syndrome[J]. Herz, 2015, 40(8): 1027-1033. doi: 10.1007/s00059-015-4369-1
[3] Ahrens I, Averkov O, Zúñiga EC, et al. Invasive and antiplatelet treatment of patients with non-ST-segment elevation myocardial infarction: Understanding and addressing the global risk-treatment paradox[J]. Clin Cardiol, 2019, 42(10): 1028-1040. doi: 10.1002/clc.23232
[4] Awan A, Ogunti R, Fatima U, et al. Timing of Percutaneous Coronary Intervention in Non-ST Elevation Acute Coronary Syndrome-Meta-Analysis and Systematic Review of Literature[J]. Cardiovasc Revasc Med, 2020, 21(11): 1398-1404. doi: 10.1016/j.carrev.2019.10.004
[5] Kite TA, Kurmani SA, Bountziouka V, et al. Timing of invasive strategy in non-ST-elevation acute coronary syndrome: a meta-analysis of randomized controlled trials[J]. Eur Heart J, 2022, 43(33): 3148-3161. doi: 10.1093/eurheartj/ehac213
[6] Guedeney P, Thiele H, Collet JP. Timing of invasive management of NSTE-ACS: is the time up for early management?[J]. Eur Heart J, 2022, 43(33): 3161-3163. doi: 10.1093/eurheartj/ehac212
[7] Javat D, Heal C, Buchholz S, et al. Early Versus Delayed Invasive Strategies in High-Risk Non-ST Elevation Acute Coronary Syndrome Patients-A Systematic Literature Review and Meta-Analysis of Randomised Controlled Trials[J]. Heart Lung Circ, 2017, 26(11): 1142-1159. doi: 10.1016/j.hlc.2017.02.031
[8] Bonello L, Laine M, Puymirat E, et al. Timing of Coronary Invasive Strategy in Non-ST-Segment Elevation Acute Coronary Syndromes and Clinical Outcomes: An Updated Meta-Analysis[J]. JACC Cardiovasc Interv, 2016, 9(22): 2267-2276. doi: 10.1016/j.jcin.2016.09.017
[9] Kite TA, Bountziouka V, Ladwiniec A. Timing of invasive strategy in non-ST-elevation acute coronary syndrome: risk and reward?[J]. Eur Heart J, 2022, 43(44): 4661. doi: 10.1093/eurheartj/ehac467
[10] Eggers KM, James SK, Jernberg T, et al. Timing of coronary angiography in patients with non-ST-elevation acute coronary syndrome: long-term clinical outcomes from the nationwide SWEDEHEART registry[J]. EuroIntervention, 2022, 18(7): 582-589. doi: 10.4244/EIJ-D-21-00982
[11] 马嘉政, 叶泽康, 李冉, 等. 光比浊法检测氯吡格雷血小板抑制作用的稳态时间[J]. 临床心血管病杂志, 2022, 38(4): 276-281. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.04.005
[12] Yang B, Zheng C, Yu H, et al. Comparison of Ticagrelor and Clopidogrel for Patients Undergoing Emergency Percutaneous Coronary Intervention[J]. Iran J Public Health, 2018, 47(7): 952-957.
[13] Bavishi C, Panwar S, Messerli FH, et al. Meta-Analysis of Comparison of the Newer Oral P2Y12 Inhibitors(Prasugrel or Ticagrelor)to Clopidogrel in Patients With Non-ST-Elevation Acute Coronary Syndrome[J]. Am J Cardiol, 2015, 116(5): 809-817. doi: 10.1016/j.amjcard.2015.05.058
[14] 司家章, 冯雪茹, 刘梅林. 老年患者服用不同剂量氯吡格雷、替格瑞洛的反应性及安全性分析[J]. 临床心血管病杂志, 2022, 38(6): 460-466. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.06.007
[15] Kofoed KF, Kelbæk H, Hansen PR, et al. Early Versus Standard Care Invasive Examination and Treatment of Patients With Non-ST-Segment Elevation Acute Coronary Syndrome[J]. Circulation, 2018, 138(24): 2741-2750. doi: 10.1161/CIRCULATIONAHA.118.037152
[16] Katritsis DG, Siontis GC, Kastrati A, et al. Optimal timing of coronary angiography and potential intervention in non-ST-elevation acute coronary syndromes[J]. Eur Heart J, 2011, 32(1): 32-40. doi: 10.1093/eurheartj/ehq276
[17] Lemesle G, Laine M, Pankert M, et al. Optimal Timing of Intervention in NSTE-ACS Without Pre-Treatment: The EARLY Randomized Trial[J]. JACC Cardiovasc Interv, 2020, 13(8): 907-917. doi: 10.1016/j.jcin.2020.01.231
[18] Milosevic A, Vasiljevic-Pokrajcic Z, Milasinovic D, et al. Immediate Versus Delayed Invasive Intervention for Non-STEMI Patients: The RIDDLE-NSTEMI Study[J]. JACC Cardiovasc Interv, 2016, 9(6): 541-549. doi: 10.1016/j.jcin.2015.11.018
[19] 孟阳, 郭爽, 李健超, 等. 非ST段抬高型心肌梗死患者罪犯血管闭塞的特殊心电图表现[J]. 临床心血管病杂志, 2022, 38(11): 876-881. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.11.007
[20] Bergmark BA, Mathenge N, Merlini PA, et al. Acute coronary syndromes[J]. Lancet, 2022, 399(10332): 1347-1358. doi: 10.1016/S0140-6736(21)02391-6
[21] Smit M, Coetzee AR, Lochner A. The Pathophysiology of Myocardial Ischemia and Perioperative Myocardial Infarction[J]. J Cardiothorac Vasc Anesth, 2020, 34(9): 2501-2512. doi: 10.1053/j.jvca.2019.10.005
-




 下载:
下载: