Analysis of the efficacy of sacubitril/valsartan in the treatment of young myocardial infarction patients without heart failure
-
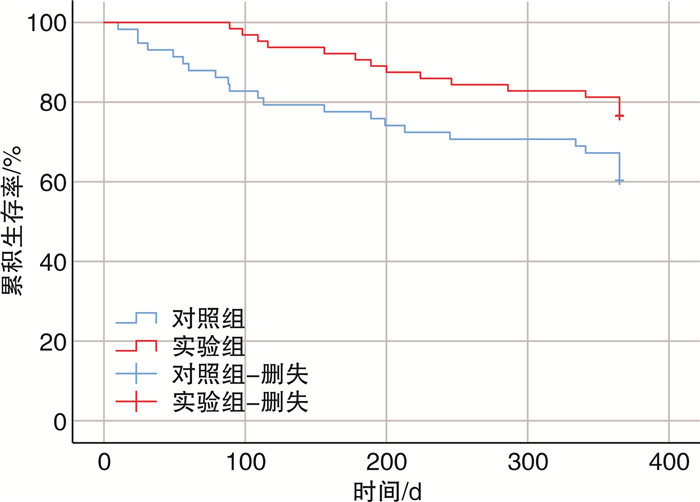
摘要: 目的 对沙库巴曲缬沙坦用于治疗不合并心力衰竭的年轻心肌梗死患者的临床效果进行观察和统计分析,为临床安全用药提供参考。方法 连续收集2019年3月—2020年12月就诊于我院诊断为急性心肌梗死(AMI)的122例年轻(< 45岁)患者,要求入院至少2次心脏彩超射血分数(EF)>50%、脑钠肽(BNP)/氨基末端脑钠肽前体(NT-proBNP)正常。将患者随机分为试验组(沙库巴曲缬沙坦治疗,64例)与对照组(培哚普利治疗,58例)。所有入选患者随访1年。采用Kaplan-Meier法绘制生存曲线,探究两组1年主要不良心血管事件(MACE)差异。采用多因素Cox回归对两组患者1年MACE发生的影响因素进行分析。结果 随访1年期间,试验组发生MACE 16例(25.00%),对照组发生MACE 27例(44.83%)。Kaplan-Meier曲线结果表明,与对照组比较,试验组MACE累积发生率更低(log-rank P=0.036)。多因素Cox回归分析结果显示,应用沙库巴曲缬沙坦治疗可降低院外不良事件的发生(HR=3.671,95%CI1.820~7.403,P=0.000)。结论 沙库巴曲缬沙坦可提高不合并心力衰竭的年轻AMI患者疗效,减少不良事件发生。Abstract: Objective To analyze the therapeutic efficacy of sacubitril/valsartan in young myocardial infarction (MI) patients without heart failure.Methods A retrospective analysis was conducted on a cohort of young patients (age younger than 45 years) admitted to our hospital for acute MI between March 2019 and September 2020. Selection criteria ensured that all cases had undergone echocardiography at least twice, with both instances indicating an ejection fraction (EF) above 40%, and normal levels of brain natriuretic peptide (BNP) or N-terminal pro-brain natriuretic peptide (NT-proBNP). The patients were randomly assigned to either the experimental group (treated with sacubitril/valsartan, n=64) or the control group (treated with peridopril, n=58). A one-year follow-up period was undertaken. Survival curves were generated using the Kaplan-Meier method to elucidate adverse outcomes between the two groups. Multivariate Cox regression analysis was employed to explore factors influencing one-year major adverse cardiovascular events (MACE).Results During the one-year follow-up, MACE occured in 16 cases (25.00%) in the experimental group and 27 cases (44.83%) in the control group. Kaplan-Meier survival curves revealed a lower cumulative incidence of MACE in the experimental group compared to the control group (log-rank P=0.036). Multivariate Cox regression analysis showed that sacubitril/valsartan therapy was associated with reduced the incidence of adverse outcomes (HR=3.671, 95%CI 1.820 - 7.403, P=0.000).Conclusion Sacubitril-valsartan can improve the efficacy and reduce the incidence of adverse events in young AMI patients without heart failure.
-

-
表 1 两组患者基础资料比较
Table 1. Comparison of general data
例(%), X±S 项目 对照组(58例) 试验组(64例) t/χ2 P 年龄/岁 37.07±4.71 36.17±5.44 -0.969 0.334 男性 38(65.5) 40(62.5) 0.12 0.729 BMI/(kg/m2) 24.96±2.82 24.97±2.77 -0.024 0.981 熬夜 32(55.2) 42(65.6) 1.393 0.238 缺乏体育锻炼 39(67.2) 43(67.2) 0 0.995 饮酒 37(63.8) 39(61.0) 0.106 0.745 吸烟史 32(55.2) 39(61.0) 0.416 0.519 高血压 16(27.6) 20(31.3) 0.001 0.980 高脂血症 30(51.7) 38(59.4) 0.722 0.396 2型糖尿病 14(24.1) 14(21.9) 0.088 0.767 高尿酸血症 21(34.5) 22(37.5) 0.045 0.832 冠心病家族史 19(32.8) 18(28.1) 0.309 0.578 冠状动脉病变情况 左主干病变 2(3.4) 4(4.7) 0.100 0.547 前降支病变 38(65.5) 39(61.0) 0.274 0.601 回旋支病变 11(19.0) 15(23.4) 0.363 0.547 右冠病变 16(27.6) 22(34.4) 0.654 0.419 3支病变 2(3.4) 3(4.7) 0.100 0.547 D-to-W/min 33.17±15.60 36.95±17.92 1.224 0.223 STEMI 19(15.5) 16(9.4) 0.895 0.344 累及前壁的AMI 14(24.1) 16(25.0) 0.012 0.912 累及下壁的AMI 10(17.2) 13(20.3) 0.188 0.665 检验及心功能指标 血红蛋白/(g/L) 125.90±11.81 127.42±12.93 0.678 0.499 LVEDD/mm 48.53±2.98 48.92±2.53 0.777 0.439 出院前LVEF/% 58.62±4.46 58.13±5.74 -0.529 0.598 NT-proBNP/(pg/mL) 84.03±21.63 76.13±26.19 -1.808 0.073 血运重建后药物 阿司匹林 57(98.3) 64(100) - 0.475 氯吡格雷 17(29.3) 18(28.1) 0.021 0.885 替格瑞洛 40(69.0) 46(71.9) 0.124 0.725 β受体阻滞剂 48(82.8) 50(78.1) 0.413 0.520 他汀类 57(98.3) 63(98.4) - 1.000 STEMI:ST段抬高型心肌梗死;LVEDD:左心室舒张末期内径;NT-proBNP:氨基末端脑钠肽前体。 表 2 两组患者不良反应发生情况
Table 2. Adverse reactions in two groups
例(%) 项目 对照组(58例) 试验组(64例) χ2 P 咳嗽 2(3.4) 0 0.224 低血压 3(5.2) 2(2.9) 0.013 0.910 肾功能不全 2(3.4) 1(1.6) 0.007 0.931 高钾血症 1(1.7) 1(1.6) 1.000 表 3 多因素Cox回归分析结果
Table 3. Multivariate Cox regression analysis results
因素 B SE Wald χ2 HR 95%CI P 组别 1.300 0.358 13.202 3.671 1.820~7.403 0.000 吸烟 2.657 0.616 18.633 14.254 4.266~47.632 0.000 β受体阻滞剂 -0.806 0.389 4.288 0.446 0.208~0.958 0.038 D-to-W 0.033 0.009 12.606 1.034 1.015~1.053 0.000 -
[1] Lurid LH, Benson L, Dahlstrom U, et al. Association between use of β-blockers and outcomes in patients with heart failure and preserved ejection fraction[J]. JAMA, 2014, 312(19): 2008-2018. doi: 10.1001/jama.2014.15241
[2] 王德征, 沈成凤, 张颖, 等. 天津市15年急性心肌梗死发病率变化趋势分析[J]. 中华心血管病杂志, 2017, 45(2): 154-159. doi: 10.3760/cma.j.issn.0253-3758.2017.02.016
[3] 高静, 王洁, 冯利娟, 等. 年龄≤45岁早发急性心肌梗死临床特点与临床结局的队列研究[J]. 中国医师杂志, 2021, 2(3): 347-353, 358. doi: 10.3760/cma.j.cn431274-20200226-00189
[4] Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction[J]. Circulatio, 2019, 139(8): 1047-1056. doi: 10.1161/CIRCULATIONAHA.118.037137
[5] 中国医师协会胸痛专业委员会, 中华心血管病杂志(网络版)编辑委员会, 急性心肌梗死后心室重构防治专家共识起草组. 急性心肌梗死后心室重构防治专家共识[J]. 中华心血管病杂志(网络版), 2020, 3(1): 1-7.
[6] 皮林, 孙子程, 李莉, 等. 急性心肌梗死住院患者临床特点的性别差异及死亡危险因素分析[J]. 中国医刊, 2017, 52(5): 30-33. doi: 10.3969/j.issn.1008-1070.2017.05.010
[7] 张海波, 吴鹏, 任平, 等. 高原中青年急性ST段抬高型心肌梗死患者的临床特点和近期预后[J]. 岭南心血管病杂志, 2018, 24(1): 30-33. doi: 10.3969/j.issn.1007-9688.2018.01.08
[8] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. Circulation, 2018, 13(20): e618-e651.
[9] Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010[J]. J Am Coll Cardiol, 2014, 64(4): 337-345. doi: 10.1016/j.jacc.2014.04.054
[10] 孙佳艺, 刘静, 谢学勤, 等. 2007至2009年北京市25岁以上居民急性冠心病事件发病率的监测[J]. 中华心血管病杂志, 2012, 40(3): 194-198. doi: 10.3760/cma.j.issn.0253-3758.2012.03.004
[11] Wang X, Gao M, Zhou S, et al. Trend in young coronary artery disease in China from 2010 to 2014: aretrospective study of young patients oung patientCardiovasc Disord, 2017, 17(1): 18.
[12] Cole JH, Miller III JI, Sperling LS, et al. Long-term follow-up of coronary artery disease presenting in young adults[J]. J Am Coll Cardiol 2003, 41: 521030.
[13] Wittlinger T, Seifert C, Simonis G, et al. Prognosis in myocardial infarction of young patients: Results of a prospective registry[J]. Int J Cardiol, 2019, 300: 1-6.
[14] Wu WY, Biery DW, Singh A, et al. Recovery of left ventricular systolic function and clinical outcomes in young adults with myocardial infarction[J]. J Am Coll Cardiol, 2020, 75(22): 2804-2815. doi: 10.1016/j.jacc.2020.03.074
[15] Gulati R, Behfar A, Narula J, et al. Acute myocardial infarction in young individuals[J]. Mayo Clinic Proc, 2020, 95(1): 136-156. doi: 10.1016/j.mayocp.2019.05.001
[16] Desala S, Solomon SD, Shah AM, et al. Effect of sacubitril-valsartan vs enalapril on aortic stiffness in patients withheart failure and reduced ejection fraction: A randomized clinical Trial[J]. JAMA, 2019, 322(11): 1077-1084. doi: 10.1001/jama.2019.12843
[17] Januzzi JJ, Prescott MF, Butler J, et al. Associationof change in N-terminal Pro-B-type natriuretic peptide followinginitiation of sacubitril-valsartan treatment with cardiac structureand function in patients with heart failure with reduced ejectionfraction[J]. JAMA, 2019, 322(11): 1085-1095. doi: 10.1001/jama.2019.12821
[18] 冯娟, 闫奎坡, 朱翠玲, 等. 沙库巴曲缬沙坦对急性心肌梗死后不良心血管事件及心功能影响的Meta分析[J]. 临床心血管病杂志, 2021, 37(6): 531-536. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.06.008
[19] Mehta SR, Eikelboom JW, Demers C, et al. Congestive heart failure complicating non-ST segment elevation acute coronary syndrome: incidence, predictors, and clinical outcomes[J]. Can J Physiol Pharmacol, 2005, 83(1): 98-103. doi: 10.1139/y05-003
[20] Feng L, Karpinski PH, Sutton P, et al. LCZ696: a dual-acting sodium supramolecular complex[J]. Tetrahedron Lett, 2012, 53(3): 275-276. doi: 10.1016/j.tetlet.2011.11.029
[21] 中国医疗保健国际交流促进会高血压分会, 中国医师协会心血管分会, 中国高血压联盟, 等. 沙库巴曲缬沙坦在高血压患者临床应用的中国专家建议[J]. 中华高血压杂志, 2021, 29(2): 108-114. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202102006.htm
[22] 刘岳, 汪芳. 沙库巴曲缬沙坦的药代动力学和药效学特点[J]. 中国循环杂志, 2018, 33(2): 198-200. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH201802026.htm
[23] Torrado J, Cain C, Mauro A G, et al. Sacubitril-Valsartan Averts Adverse Post-Infarction Ventricular Remodeling and Preserves Systolic Function in Rabbits[J]. J Am Coll Cardiol, 2018, 72(19): 2342-2356. doi: 10.1016/j.jacc.2018.07.102
[24] Mcmurray J, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure[J]. N Engl J Med, 2014, 371(11): 993-1004. doi: 10.1056/NEJMoa1409077
[25] Solomon SD, Vaduganathan M, Claggett BL, et al. Sacubitril-valsartan across the spectrum of ejection fraction in heart failure[J]. Circulation, 2020, 141(5): 352-361. doi: 10.1161/CIRCULATIONAHA.119.044586
[26] Desal AS, Solomon SD, Shah AM, et al. Effect of sacubitril-valsartan vs enalapril on aortic stiffness in patients with heart failure and reduced ejection fraction: A randomized clini-cal Trial[J]. JAMA, 2019, 322(11): 1077-1084.
[27] Januzzi JJ, Prescott MF, Butler J, et al. Association of change in N-terminal Pro-B-type natriuretic peptide following initiation of sacubitril-valsartan treatment with cardiac structure and function in patients with heart failure with reduced ejection fraction[J]. JAMA, 2019, 322(11): 1085-1095.
-




 下载:
下载: