Predictive value of electrocardiography for infarct size in patients with ST-segment elevation myocardial infarction
-
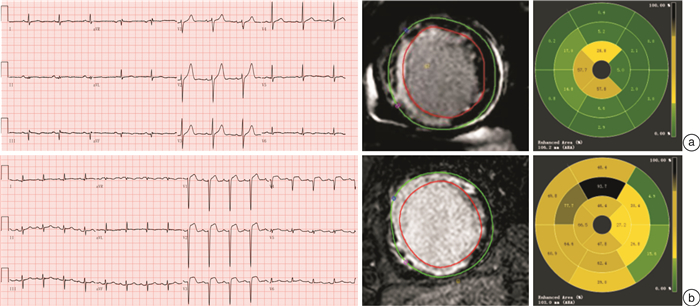
摘要: 梗死面积是ST段抬高型心肌梗死主要不良心血管事件的独立预测指标。心脏磁共振(CMR)可全面展现梗死后心肌组织学变化特征,其晚期钆增强图像是活体检测和量化梗死面积及微血管阻塞的金标准。然而CMR获取成本较高,且存在禁忌证,而心电图评估梗死面积简便易行。本研究总结了目前心电图评估梗死面积的研究,为临床决策提供依据。
-
关键词:
- 心脏磁共振 /
- 左室射血分数 /
- 梗死面积 /
- Selvester QRS评分
Abstract: Infarct size is an independent predictor of major adverse cardiovascular events in ST-segment elevation myocardial infarction. Cardiac magnetic resonance(CMR) can fully demonstrate the histological characteristics of myocardial infarction, and late gadolinium enhanced images are the gold standard for in vivo detection and quantification of infarct size as well as microvascular obstruction. However, the acquisition cost of CMR is high and there are contraindications. ECG is simple and easy to evaluate the infarct size. This study summarizes the current studies on ECG assessment of infarct size and provides evidence for clinical decision-making. -

-
表 1 AMI梗死面积的评分系统
Table 1. Scoring system of size in AMI
研究人群来源 样本量/例 评分系统及主要发现 梗死面积测量(金标准) 杜克大学医学中心 349(正常人)+50(AMI患者) 基于12导联心电图的初始Selvester QRS评分(52项标准32分)改良为37项标准29分制的简易Selvester QRS评分系统[20-21]。 活检 急性心肌梗死-乙酰半胱氨酸临床研究(NACIAM)(澳大利亚) 60 Aldrich评分[28]:前壁梗死:3×[1.5(ST↑的导联数)-0.4];下壁梗死:3×[0.6(∑ ST↑Ⅱ,Ⅲ,aVF)+ 2.0]
Wilkins评分[29]:前壁梗死:1.88×(ST↑的导联数)+ 2.19 ×(异常Q波的导联数)+ 1.56×(高T波的导联数)+ 5.80;下壁梗死:0.94×(∑ST↑)+ 1.13×(∑Excess Q)+ 8.73[30]心脏磁共振(LGE-CMR) 来自DETERMINE研究和PRE-DETERMINE研究的66个医学中心(美国) 551 DETERMINE评分=[有Q的导联数×2]+[FQRS的导联数]+[TWI的导联数][22]。 心脏磁共振(LGE-CMR) -
[1] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2020概要[J]. 中国循环杂志, 2021, 36(6): 1005-1009. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXB202307002.htm
[2] Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2018, 39(2): 119-177. doi: 10.1093/eurheartj/ehx393
[3] Miller TD, Christian TF, Hopfenspirger MR, et al. Infarct size after acute myocardial infarction measured by quantitative tomographic 99mTc sestamibi imaging predicts subsequent mortality[J]. Circulation, 1995, 92(3): 334-341. doi: 10.1161/01.CIR.92.3.334
[4] Zhang SR, Li RX, Jiao YD, et al. The prognostic value of myocardial infarct size measured by cardiovascular magnetic resonance in patients with acute ST-segment elevation myocardial infarction[J]. Zhonghua Nei Ke Za Zhi, 2021, 60(8): 751-756.
[5] Stone GW, Selker HP, Thiele H, et al. Relationship Between Infarct Size and Outcomes Following Primary PCI: Patient-Level Analysis From 10 Randomized Trials[J]. J Am Coll Cardiol, 2016, 67(14): 1674-1683. doi: 10.1016/j.jacc.2016.01.069
[6] Bello D, Fieno DS, Kim RJ, et al. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia[J]. J Am Coll Cardiol, 2005, 45(7): 1104-1108. doi: 10.1016/j.jacc.2004.12.057
[7] Scott PA, Morgan JM, Carroll N, et al. The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators[J]. Circ Arrhythm Electrophysiol, 2011, 4(3): 324-330. doi: 10.1161/CIRCEP.110.959544
[8] Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association[J]. Circulation, 2011, 124(25): 2951-2960. doi: 10.1161/CIR.0b013e31823b21e2
[9] Symons R, Pontone G, Schwitter J, et al. Long-Term Incremental Prognostic Value of Cardiovascular Magnetic Resonance After ST-Segment Elevation Myocardial Infarction: A Study of the Collaborative Registry on CMR in STEMI[J]. JACC Cardiovasc Imaging, 2018, 11(6): 813-825. doi: 10.1016/j.jcmg.2017.05.023
[10] Schmidt A, Azevedo CF, Cheng A, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction[J]. Circulation, 2007, 115(15): 2006-2014. doi: 10.1161/CIRCULATIONAHA.106.653568
[11] Taylor AJ, Al-Saadi N, Abdel-Aty H, et al. Detection of acutely impaired microvascular reperfusion after infarct angioplasty with magnetic resonance imaging[J]. Circulation, 2004, 109(17): 2080-2085. doi: 10.1161/01.CIR.0000127812.62277.50
[12] Hamirani YS, Wong A, Kramer CM, et al. Effect of microvascular obstruction and intramyocardial hemorrhage by CMR on LV remodeling and outcomes after myocardial infarction: a systematic review and meta-analysis[J]. JACC Cardiovasc Imaging, 2014, 7(9): 940-952. doi: 10.1016/j.jcmg.2014.06.012
[13] Gibbons RJ, Miller TD, Christian TF. Infarct size measured by single photon emission computed tomographic imaging with(99 m)Tc-sestamibi: A measure of the efficacy of therapy in acute myocardial infarction[J]. Circulation, 2000, 101(1): 101-108. doi: 10.1161/01.CIR.101.1.101
[14] Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography(SPECT)perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study[J]. Lancet, 2003, 361(9355): 374-379. doi: 10.1016/S0140-6736(03)12389-6
[15] Ibanez B, Aletras AH, Arai AE, et al. Cardiac MRI Endpoints in Myocardial Infarction Experimental and Clinical Trials: JACC Scientific Expert Panel[J]. J Am Coll Cardiol, 2019, 74(2): 238-256. doi: 10.1016/j.jacc.2019.05.024
[16] Selvester RH, Wagner GS, Hindman NB. The Selvester QRS scoring system for estimating myocardial infarct size. The development and application of the system[J]. Arch Intern Med, 1985, 145(10): 1877-1881. doi: 10.1001/archinte.1985.00360100147024
[17] Bounous EP Jr, Califf RM, Harrell FE Jr, et al. Prognostic value of the simplified Selvester QRS score in patients with coronary artery disease[J]. J Am Coll Cardiol, 1988, 11(1): 35-41. doi: 10.1016/0735-1097(88)90163-5
[18] Roubin GS, Shen WF, Kelly DT, et al. The QRS scoring system for estimating myocardial infarct size: clinical, angiographic and prognostic correlations[J]. J Am Coll Cardiol, 1983, 2(1): 38-44. doi: 10.1016/S0735-1097(83)80374-X
[19] Anderson CI, Harrison DG, Stack NC, et al. Evaluation of serial QRS changes during acute inferior myocardial infarction using a QRS scoring system[J]. Am J Cardiol, 1983, 52(3): 252-256. doi: 10.1016/0002-9149(83)90117-0
[20] Selvester RH, Rubin HB. Quantitation of myocardial infarct size and location by electrocardiogram and vectorcardiogram[J]. Cardiology, 1971, 8: 111.
[21] Wagner GS, Freye CJ, Palmeri ST, et al. Evaluation of a QRS scoring system for estimating myocardial infarct size. I. Specificity and observer agreement[J]. Circulation, 1982, 65(2): 342-347. doi: 10.1161/01.cir.65.2.342.
[22] Lee DC, Albert CM, Narula D, et al. Estimating Myocardial Infarction Size With a Simple Electrocardiographic Marker Score[J]. J Am Heart Assoc, 2020, 9(3): e014205. doi: 10.1161/JAHA.119.014205
[23] 崔永春, 田忠, 唐跃, 等. 心电图计分法定量评价糖尿病小型猪心肌梗死面积[J]. 中国比较医学杂志, 2013, 23(6). 39-69. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGDX201306007.htm
[24] Badertscher P, Strebel I, Honegger U, et al. Automatically computed ECG algorithm for the quantification of myocardial scar and the prediction of mortality[J]. Clin Res Cardiol, 2018, 107(9): 824-835. doi: 10.1007/s00392-018-1253-z
[25] Xia X, Wieslander B, Strauss DG, et al. Automatic QRS Selvester scoring system in patients with left bundle branch block[J]. Europace, 2016, 18(2): 308-314. doi: 10.1093/europace/euv040
[26] Waks JW, Buxton AE. Risk Stratification for Sudden Cardiac Death After Myocardial Infarction[J]. Annu Rev Med, 2018, 69: 147-164. doi: 10.1146/annurev-med-041316-090046
[27] Banks L, Al-Mousawy S, Altaha MA, et al. Cardiac remodeling in middle-aged endurance athletes: relation between signal-averaged electrocardiogram and LV mass[J]. Am J Physiol Heart Circ Physiol, 2021, 320(1): H316-H322. doi: 10.1152/ajpheart.00602.2020
[28] Aldrich HR, Wagner NB, Boswick J, et al. Use of initial ST-segment deviation for prediction of final electrocardiographic size of acute myocardial infarcts[J]. Am J Cardiol, 1988, 61(10): 749-753. doi: 10.1016/0002-9149(88)91060-0
[29] Wilkins ML, Maynard C, Annex BH, et al. Admission prediction of expected final myocardial infarct size using weighted ST-segment, Q wave, and T wave measurements[J]. J Electrocardiol, 1997, 30(1): 1-7. doi: 10.1016/S0022-0736(97)80029-5
[30] Du YT, Pasupathy S, Air T, et al. Validation of contemporary electrocardiographic indices of area at risk and infarct size in acute ST elevation myocardial infarction(STEMI)[J]. Int J Cardiol, 2020, 303: 1-7. doi: 10.1016/j.ijcard.2019.10.041
[31] Smith FM. The ligation of coronary arteries with electrocardiographic study. 1918[J]. Ann Noninvasive Electrocardiol, 2004, 9(1): 80-93. doi: 10.1111/j.1542-474X.2004.91003.x
[32] Younis A, Goldenberg M, Kutyifa V, et al. Applicability of the MADIT-CRT Response Score for Prediction of Long-Term Clinical and Arrhythmic Events by QRS Morphology[J]. Circ Arrhythm Electrophysiol, 2020, 13(9): e008499. doi: 10.1161/CIRCEP.120.008499
[33] Nijveldt R, van der Vleuten PA, Hirsch A, et al. Early electrocardiographic findings and MR imaging-verified microvascular injury and myocardial infarct size[J]. JACC Cardiovasc Imaging, 2009, 2(10): 1187-1194. doi: 10.1016/j.jcmg.2009.06.008
[34] Yasuda M, Iida H, Itagane H, et al. Significance of Q wave disappearance in the chronic phase following transmural acute myocardial infarction[J]. Jpn Circ J, 1990, 54(12): 1517-1524. doi: 10.1253/jcj.54.12_1517
[35] Yang H, Pu M, Rodriguez D, et al. Ischemic and viable myocardium in patients with non-Q-wave or Q-wave myocardial infarction and left ventricular dysfunction: a clinical study using positron emission tomography, echocardiography, and electrocardiography[J]. J Am Coll Cardiol, 2004, 43(4): 592-598. doi: 10.1016/j.jacc.2003.07.052
[36] Rommel KP, Badarnih H, Desch S, et al. QRS complex distortion(Grade 3 ischaemia)as a predictor of myocardial damage assessed by cardiac magnetic resonance imaging and clinical prognosis in patients with ST-elevation myocardial infarction[J]. Eur Heart J Cardiovasc Imaging, 2016, 17(2): 194-202. doi: 10.1093/ehjci/jev135
[37] Das MK, Khan B, Jacob S, et al. Significance of a fragmented QRS complex versus a Q wave in patients with coronary artery disease[J]. Circulation, 2006, 113(21): 2495-2501. doi: 10.1161/CIRCULATIONAHA.105.595892
[38] Dabbagh Kakhki VR, Ayati N, Zakavi SR, et al. Comparison between fragmented QRS and Q waves in myocardial scar detection using myocardial perfusion single photon emission computed tomography[J]. Kardiol Pol, 2015, 73(6): 437-444. doi: 10.5603/KP.a2014.0242
[39] Zhao Q, Zhang R, Hou J, et al. Relationship between Fragmented QRS and NT-proBNP in Patients with ST Elevation Myocardial Infarction Who Underwent Primary Percutaneous Coronary Intervention[J]. Acta Cardiol Sin, 2018, 34(1): 13-22.
[40] DePace NL, Colby J, Hakki AH, et al. Poor R wave progression in the precordial leads: clinical implications for the diagnosis of myocardial infarction[J]. J Am Coll Cardiol, 1983, 2(6): 1073-1079. doi: 10.1016/S0735-1097(83)80332-5
[41] Kurisu S, Iwasaki T, Watanabe N, et al. Poor R-wave progression and myocardial infarct size after anterior myocardial infarction in the coronary intervention era[J]. Int J Cardiol Heart Vasc, 2015, 7: 106-109.
[42] Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society[J]. Circulation, 2018, 138(13): e272-e391.
[43] Weir RA, Martin TN, Murphy CA, et al. Comparison of serial measurements of infarct size and left ventricular ejection fraction by contrast-enhanced cardiac magnetic resonance imaging and electrocardiographic QRS scoring in reperfused anterior ST-elevation myocardial infarction[J]. J Electrocardiol, 2010, 43(3): 230-236. doi: 10.1016/j.jelectrocard.2010.01.003
[44] 张勇, 张奇, 王德国, 等. 心电图Selvester QRS积分评价急性病毒性心肌炎并发左心功能异常的临床价值[J]. 临床心血管病杂志, 2021, 37(2): 137-140. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.02.010
[45] Palmeri ST, Harrison DG, Cobb FR, et al. A QRS scoring system for assessing left ventricular function after myocardial infarction[J]. N Engl J Med, 1982, 306(1): 4-9. doi: 10.1056/NEJM198201073060102
[46] Seino Y, Staniloff HM, Shell WE, et al. Evaluation of a QRS scoring system in acute myocardial infarction: relation to infarct size, early stage left ventricular ejection fraction, and exercise performance[J]. Am J Cardiol, 1983, 52(1): 37-42. doi: 10.1016/0002-9149(83)90065-6
[47] Pollard JD, Haq KT, Lutz KJ, et al. Sex differences in vectorcardiogram of African-Americans with and without cardiovascular disease: a cross-sectional study in the Jackson Heart Study cohort[J]. BMJ Open, 2021, 11(1): e042899. doi: 10.1136/bmjopen-2020-042899
[48] 买买提伊明, 都雯, 高嵩. 不同平面QRS-T夹角水平陈旧性心肌梗死患者心功能不全的评估价值研究[J]. 四川医学, 2017, 38(2): 111. https://www.cnki.com.cn/Article/CJFDTOTAL-SCYX201707010.htm
[49] Selvaraj S, Ilkhanoff L, Burke MA, et al. Association of the frontal QRS-T angle with adverse cardiac remodeling, impaired left and right ventricular function, and worse outcomes in heart failure with preserved ejection fraction[J]. J Am Soc Echocardiogr, 2014, 27(1): 74-82 e72. doi: 10.1016/j.echo.2013.08.023
[50] Adedinsewo D, Carter RE, Attia Z, et al. Artificial Intelligence-Enabled ECG Algorithm to Identify Patients With Left Ventricular Systolic Dysfunction Presenting to the Emergency Department With Dyspnea[J]. Circ Arrhythm Electrophysiol, 2020, 13(8): e008437. doi: 10.1161/CIRCEP.120.008437
[51] Raghunath S, Ulloa Cerna AE, Jing L, et al. Prediction of mortality from 12-lead electrocardiogram voltage data using a deep neural network[J]. Nat Med, 2020, 26(6): 886-891. doi: 10.1038/s41591-020-0870-z
[52] Potter EL, Rodrigues C, Ascher DB, et al. Machine Learning of ECG Waveforms to Improve Selection for Testing for Asymptomatic Left Ventricular Dysfunction[J]. JACC Cardiovasc Imaging, 2021, 14(10): 1904-1915. doi: 10.1016/j.jcmg.2021.04.020
[53] Potter E, Liu Y, Teo S, et al. Machine learning applied to energy waveform ECG for prediction of subclinical myocardial dysfunction[J]. European Heart Journal, 2019, 40(Supplement_1): 111.
[54] Kagiyama N, Piccirilli M, Yanamala N, et al. Machine Learning Assessment of Left Ventricular Diastolic Function Based on Electrocardiographic Features[J]. J Am Coll Cardiol, 2020, 76(8): 930-941. doi: 10.1016/j.jacc.2020.06.061
[55] Bouzid Z, Faramand Z, Gregg RE, et al. In Search of an Optimal Subset of ECG Features to Augment the Diagnosis of Acute Coronary Syndrome at the Emergency Department[J]. J Am Heart Assoc, 2021, 10(3): e017871. doi: 10.1161/JAHA.120.017871
-




 下载:
下载:
