Perioperative management and cardiovascular outcomes of patients with cardiac implantable electronic device undergoing surgery-a single center retrospective cohort study
-
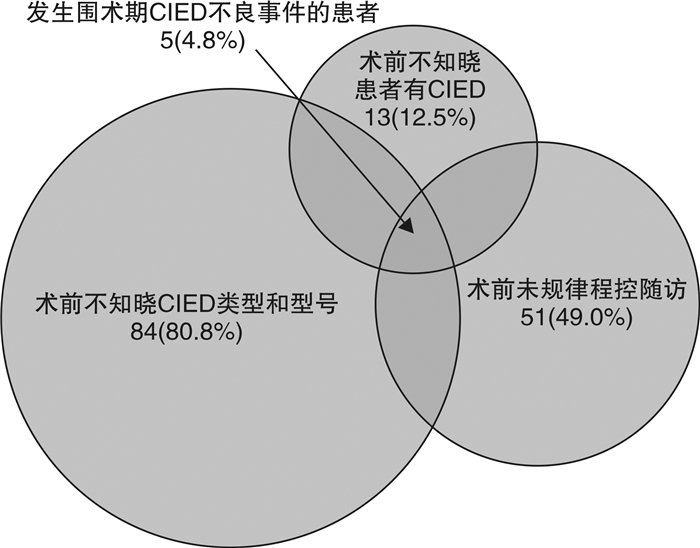
摘要: 目的 调查当前心脏植入式电子设备(CIED)患者外科手术围术期评估和管理措施,探讨目前处理流程与共识推荐的差距,以及与CIED患者围术期心脏结局的关系。方法 回顾性队列研究近2年来在本中心进行外科手术并具有CIED的患者。结果 纳入2020年7月—2022年7月在本中心接受外科手术的CIED患者共104例,平均年龄(73±11)岁,女性49例。术前评估发现12.5%的患者在手术科室未能确认其具有CIED,多达80.8%的会诊申请未能提供CIED类型及型号,49.0%的患者既往没有规律程控随访,总体术前评估与共识建议依从度仅8%。择期手术前准备时,所有患者均由专业随访护士联系电生理医师进行了CIED程控,获得CIED功能状态和电量的信息,并建议术中采用减少电磁干扰(EMI)和备用起搏/除颤的措施。部分CIED患者术前程控更改为非同步模式,术后由专业随访护士再次联系电生理医师程控确认参数良好,并恢复原工作模式。术前准备及术后管理流程与共识推荐依从度均达100%。术前因程控发现问题造成手术延迟2例,取消1例。CIED相关的复合终点事件发生共5例(4.8%),均与术前不规范的评估流程相关。围手术期心脏事件发生28例(27.2%),但均与CIED围术期处理无关。结论 目前CIED患者外科手术围术期评估过程与国际共识建议存在差距,专业规范的CIED围术期管理对避免手术延搁,降低围手术期器械和心脏事件的发生具有重要作用。Abstract: Objective We aimed to investigate the gap between current perioperative assessment and management for patients with cardiac implantable electronic devices(CIED) and recommendations from consensus, and to explore its possible association with the perioperative adverse outcomes involving CIED and cardiovascular events. A professional nurse-led perioperative workflow were suggested as a quality-improvement approach.Methods A retrospective cohort study was performed on patients with CIED who underwent surgery in our center in the past two years.Results A total of 104 CIED patients undergoing surgery in our center from July 2020 to July 2022 were enrolled. The average age of the subjects was(73±11) years, and 49 of them were females. In preoperative evaluation, it was found that up to 12.5% of patients failed to confirm the status of their CIED in the surgery ward, and 80.8% of the consultations failed to provide the type and model of the CIED, 49.0% of patients did not take regular follow-up for their devices. The general adherence of the practical preoperational evaluation to the current consensus was 8%. Before elective surgery, all patients were contacted by professional nurses for arranging cardiac electrophysiologist to interrogate and obtain information on the functional and battery status of CIED. Measures to avoid electromagnetic interference(EMI) and to provide pacing/defibrillation backup were recommended. Some patients were programmed to asynchronous mode before the operations. Professional nurses were contact after the operations and the CIED parameters were confirmed and re-programmed to the original mode. The general adherence of the practical preoperational and post-operational management to the current consensus was 100%. Two surgeries were delayed, and one was canceled due to CIED dysfunction found in the interrogation. The overall CIED-related composite events were found in 5 cases(4.8%), all of which were associated with inappropriate preoperational evaluation. The perioperative cardiac events occurred in 28 cases(27.2%) although no correlation was found between the occurrence and the perioperative management of CIED.Conclusion There is a gap between the perioperative evaluation of CIED patients in current clinical practice and the international consensus recommendations. Multidisciplinary collaboration and standardized perioperative management of CIED are essential to avoid surgery delays and reduce perioperative cardiac adverse events.
-

-
表 1 患者基线特征,植入的CIED类型和植入指征
Table 1. General data
例(%), X±S 指标 数值 年龄/岁 73±11 男/女/例 55/49 合并疾病 高血压 68(65.4) 冠心病 33(31.7) 心肌病 5(4.8) 心力衰竭史 15(14.4) 心房颤动 29(27.9) 糖尿病 35(33.7) 脑血管病 20(19.2) CIED类型 103(99.0)* PPM 单腔 8(7.7) 双腔 88(84.6) ICD 5(4.8) CRT-P/D 2(1.9) *1例患者在术前程控时发现电量完全耗竭,不能确认CIED类型。 表 2 CIED患者接受的外科手术特征
Table 2. Surgical characteristics of CIED patients
例(%), M(P25, P75) 手术情况 数值 涉及手术科室 泌尿外科 33(32.0) 骨科 19(18.4) 胃肠外科 16(15.5) 肝胆外科 3(2.9) 其他普通外科 8(7.8) 妇产科 9(8.7) 血管外科 4(3.9) 心胸外科 11(10.7) 麻醉方式 全身麻醉 90(87.4) 椎管内麻醉 10(9.7) 局部麻醉 3(2.9) 手术体位 平卧位 44(42.7) 侧卧位 22(21.2) 截石位 32(30.8) 俯卧位 5(4.8) 手术时间/min 93(56,149) 麻醉时间/min 153(110,219) 入ICU 49(47.6) 表 3 围术期CIED评估和处理与共识推荐的差距
Table 3. Assessment and management gap between perioperative CIED and consensus recommendation
例(%) 围术期CIED评估和处理 完成情况 术前评估 既往规律程控随访 53(51.0) 确定患者是否有CIED 91(87.5) 确定装置类型(PM、ICD、CRT-P/D) 20(19.2) 总体术前评估规范处理依从性/% 8.7 术前准备 确定装置类型(PM、ICD、CRT-P/D) 103(99.0)* 确定患者是否起搏依赖 104(100) 确定设备功能状态 104(100) 建议外科医师尽可能使用双极电外科或超声手术刀 104(100) 临时起搏和体外心脏复律除颤器可用 104(100) 暂停频率响应、夜间/休息频率功能 6(100) 永久起搏器和CRT 98例 评估不太可能有EMI的手术不需要额外的干预措施 50(51) 可能有EMI的手术,对起搏依赖的患者程控为非同步模式 48(49) ICD 5例 暂停抗心动过速治疗 5(100) 可能有EMI的手术,对起搏依赖的患者程控为非同步模式 5(100) 总体术前准备规范处理依从性/% 100 术后管理 持续监测心率和节律,备用起搏和心脏复律除颤设备应随时可用; 103(100) 询问和恢复CIED功能 53(100) 总体术后管理规范处理依从性/% 100 *1例患者在术前程控时发现电量完全耗竭,不能确认CIED类型。 表 4 CIED相关手术延迟或取消、器械相关不良事件和围术期心脏事件
Table 4. CIED-related surgical delay or cancellation, device-related adverse events, and perioperative cardiac events
例(%) 因CIED延迟或取消手术 2(1.9) 围术期CIED复合不良事件 5(4.8) 参数异常 4(3.8) 起搏或除颤功能异常 2(1.9) 围术期复合心脏事件 28(27.2) 围术期心肌梗死 20(19.2) 围术期心力衰竭 18(17.3) 围术期新发心律失常 2(1.9) 心源性死亡 3(2.9) 全因死亡 4(3.8) 表 5 CIED患者围术期复合心脏事件风险的单因素和多因素分析
Table 5. Univariate and multifactorial analysis of perioperative risk of complex cardiac events in CIED patients
围术期复合心脏事件 OR(95%CI) P 校正OR(95%CI) P 年龄 1.06(1.01,1.11) 0.017 1.06(1.01,1.12) 0.029 心力衰竭病史 10.85(3.09,38.08) < 0.001 12.50(3.13,49.07) < 0.001 心房颤动病史 3.73(1.48,9.40) 0.005 - - 术中舒张压 0.93(0.89,0.98) 0.002 - - -
[1] American Society of Anesthesiologists. Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators: an updated report by the american society of anesthesiologists task force on perioperative management of patients with cardiac implantable electronic devices[J]. Anesthesiology, 2011, 114(2): 247-61. doi: 10.1097/ALN.0b013e3181fbe7f6
[2] Practice Advisory for the Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Pacemakers and Implantable Cardioverter-Defibrillators 2020: An Updated Report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Erratum[J]. Anesthesiology, 2020, 132(4): 938.
[3] American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Rhythm Management Devices. Practice advisory for the perioperative management of patients with cardiac rhythm management devices: pacemakers and implantable cardioverter-defibrillators: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Rhythm Management Devices[J]. Anesthesiology, 2005, 103(1): 186-198. doi: 10.1097/00000542-200507000-00027
[4] Crossley GH, Poole JE, Rozner MA, et al. The Heart Rhythm Society(HRS)/American Society of Anesthesiologists(ASA)Expert Consensus Statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors: facilities and patient management: executive summary this document was developed as a joint project with the American Society of Anesthesiologists(ASA), and in collaboration with the American Heart Association(AHA), and the Society of Thoracic Surgeons(STS)[J]. Heart Rhythm, 2011, 8(7): e1-18. doi: 10.1016/j.hrthm.2011.05.010
[5] Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. Circulation, 2014, 130(25): 2354-2394. doi: 10.1161/CIR.0000000000000133
[6] 杜良刚. 植入心脏起搏器患者行非心脏手术围术期的管理[J]. 中国现代药物应用, 2014, 8: 51-52. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWYY201422039.htm
[7] Costa A, Richman DC. Implantable Devices: Assessment and Perioperative Management[J]. Anesthesiol Clin, 2016, 34(1): 185-199. doi: 10.1016/j.anclin.2015.10.014
[8] Rooke GA, Bowdle TA. Perioperative management of pacemakers and implantable cardioverter defibrillators: it's not just about the magnet[J]. Anesth Analg, 2013, 117(2): 292-294. doi: 10.1213/ANE.0b013e31829799f3
[9] Rooke GA, Lombaard SA, Van Norman GA, et al. Initial Experience of an Anesthesiology-based Service for Perioperative Management of Pacemakers and Implantable Cardioverter Defibrillators[J]. Anesthesiology, 2015, 123(5): 1024-1032. doi: 10.1097/ALN.0000000000000838
[10] Wilkoff BL, Auricchio A, Brugada J, et al. HRS/EHRA expert consensus on the monitoring of cardiovascular implantable electronic devices(CIEDs): description of techniques, indications, personnel, frequency and ethical considerations[J]. Heart Rhythm, 2008, 5(6): 907-925. doi: 10.1016/j.hrthm.2008.04.013
[11] Healey JS, Merchant R, Simpson C, et al. Society position statement: Canadian Cardiovascular Society/Canadian Anesthesiologists' Society/Canadian Heart Rhythm Society joint position statement on the perioperative management of patients with implanted pacemakers, defibrillators, and neurostimulating devices[J]. Can J Anaesth, 2012, 59(4): 394-407. doi: 10.1007/s12630-012-9678-8
[12] Chu SY, Li PW, Fan FF, et al. Combining CHA2DS2-VASc score into RCRI for prediction perioperative cardiovascular outcomes in patients undergoing non-cardiac surgery: a retrospective pilot study[J]. BMC Anesthesiol, 2021, 21(1): 276. doi: 10.1186/s12871-021-01496-2
[13] 程敏, 廖玉华, 袁璟. 2022ESC速递: 心力衰竭相关临床研究解读[J]. 临床心血管病杂志, 2022, 38(10): 774-776. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.10.003
-




 下载:
下载: