Development of a predictive model for ventricular fibrillation in acute ST-segment elevation myocardial infarction
-
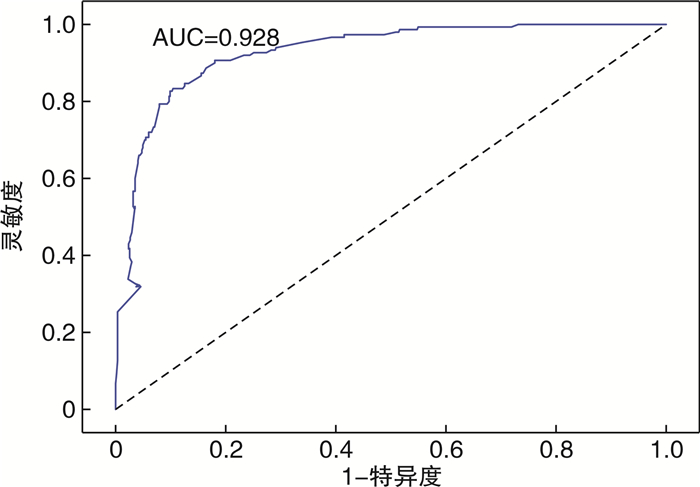
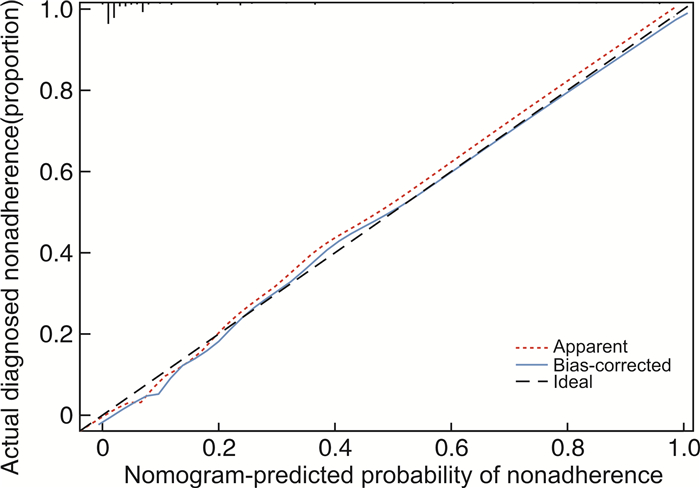
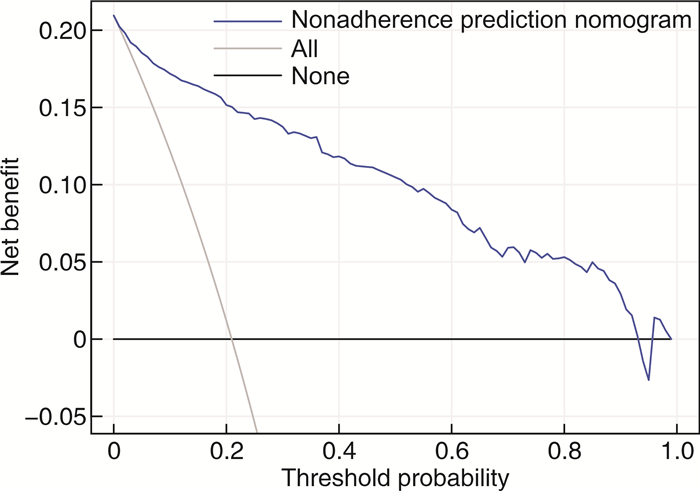
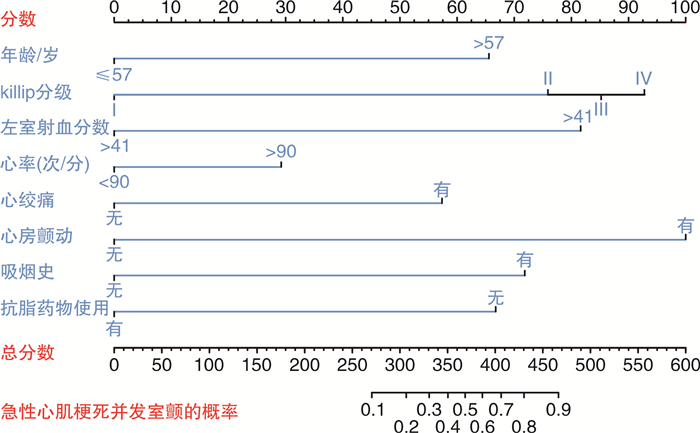
摘要: 目的 构建急性ST抬高型心肌梗死并发心室颤动的预测模型。方法 回顾性纳入2017年—2022年716例急性ST段抬高型心肌梗死患者的临床资料,根据介入治疗前有无心室颤动分成两组。应用多因素分析筛选出危险因素,然后使用Lasso回归筛选全部变量,合并共同变量,并与实际相结合,绘制列线图对心室颤动发生概率进行预测。利用ROC曲线下面积(AUC)、Harrell的C指数和校准曲线用于评估和内部验证该模型的性能。应用决策曲线分析评估该模型的临床效用。结果 ST段抬高型急性心肌梗死介入治疗前并发心室颤动的预测因素有年龄>57岁、Killip分级、左室射血分数≤41%、心率>90次/min、心绞痛、心房颤动、吸烟史、降脂药物使用。同时根据实际情况和差异变量,构造可信度比较高的列线图预测心室颤动的发生概率。结论 基于年龄、Killip分级、左室射血分数、心率、心绞痛、心房颤动、吸烟史、降脂药物等因素,构建了具有一定可信度的预测急性ST段抬高型心肌梗死介入治疗前并发心室颤动的模型。
-
关键词:
- ST抬高型急性心肌梗死 /
- 心室颤动 /
- 列线图 /
- 预测模型
Abstract: Objective To construct a prediction model for forecasting the occurrence of ventricular fibrillation in cases of acute ST-segment elevation myocardial infarction.Methods Clinical data of 716 patients with acute ST-segment elevation myocardial infarction from 2017 to 2022 were retrospectively included. Patients were divided into two groups according to the presence or absence of ventricular fibrillation before interventional therapy. Risk factors were selected by applying multivariate analysis, then all variables were further screened by using Lasso regression. Common variables were integrated with clinical context to formulate a nomogram predicting the likelihood of ventricular fibrillation. The area under the ROC curve (AUC), Harrell's C-index, and calibration curves were used to assess and internally validate the performance of the model. Decision curve analysis was applied to assess the model's clinical utility.Results Predictors of ventricular fibrillation complicating acute ST-segment elevation myocardial infarction before intervention were age >57 years, Killip classification, left ventricular ejection fraction ≤41%, heart rate >90 beats/min, angina pectoris, atrial fibrillation, history of smoking, and antilipidemic medication use. Based on the actual situation and difference variables, we developed a nomogram with relatively high reliability for predicting the probability of ventricular fibrillation.Conclusion We have constructed a nomogram with moderate reliability for predicting ventricular fibrillation before interventional treatment in acute ST-segment elevation myocardial infarction. This nomogram incorporates age, Killip classification, left ventricular ejection fraction, heart rate, angina pectoris, atrial fibrillation, history of smoking, and antilipid medication use. -

-
表 1 并发和非并发室颤患者临床资料比较
Table 1. Comparison of clinical data between patients with and without ventricular fibrillation
例(%), M(P25, P75) 项目 非并发室颤(566例) 并发室颤(150例) 统计量 P 男性 368(65.01) 101(67.33) 0.28 0.596 吸烟史 219(38.69) 114(76.00) 66.33 < 0.001 高血压病 157(27.73) 56(37.33) 5.22 0.022 糖尿病 88(15.54) 33(22.00) 3.51 0.061 IABP植入 26(4.59) 28(18.66) 33.67 < 0.001 心房颤动 195(34.45) 111(74.00) 75.78 < 0.001 心绞痛 8(1.41) 15(10.00) 28.11 < 0.001 呼吸困难 92(16.25) 58(38.66) 35.96 < 0.001 心肌梗死治疗史 163(28.79) 72(48.00) 19.82 < 0.001 抗血小板药物使用史 487(86.04) 133(88.66) 0.70 0.402 降脂药物使用史 501(88.51) 134(89.33) 19.89 < 0.001 脑卒中 163(28.79) 46(30.66) 0.20 0.655 病变血管支数 30.37 < 0.001 1 101(17.84) 55(36.66) 2 178(31.44) 50(33.33) 3 287(50.70) 45(30.00) Killip分级 125.44 < 0.001 Ⅰ 457(80.74) 54(36.00) Ⅱ 41(7.24) 22(14.66) Ⅲ 36(6.36) 33(22.00) Ⅳ 32(5.65) 41(27.33) 病变血管部位 45.63 < 0.001 左前降支 253(44.69) 103(68.66) 左回旋 49(8.65) 2(1.33) 右冠脉 240(42.40) 30(20.00) 左主干 24(4.24) 15(10.00) 年龄/岁 51(42,59) 70(60~76) -14.89 < 0.001 BMI/(kg/m2) 24.6(22.2,26.8) 24.2(22,26.6) -1.11 0.264 心率/(次/min) 73(65,82) 102(92,111) -17.31 < 0.001 收缩压/mmHg 120(110,131) 131(120,148) -8.95 < 0.001 舒张压/mmHg 80(72,88) 72(65,80) -8.60 < 0.001 WBC/(109/L) 9(7.5,10.6) 13.2(10.2,16.1) -5.71 < 0.001 PLT/(109/L) 216(184,248) 211.5(187.5,242.25) -13.42 < 0.001 Hb/(g/L) 122(107,136) 116(105,135) -1.73 0.083 ALB/(g/L) 34(31.8,36.3) 34.1(31.8,36.6) -0.46 0.642 ALT/(U/L) 77.4(55.5,101.4) 75.4(51.7,100.5) -0.27 0.783 AST/(U/L) 337.95(205.2,492.3) 372.55(211.1,509.6) -0.83 0.402 TBil/(μmol/L) 33.3(20.9,47.1) 36.55(22.6,51.1) -0.62 0.535 ALP/(U/L) 83(66,96) 79.5(66,99) -1.38 0.167 Scr/(μmol/L) 96(77,114) 90.5(75,112) -0.28 0.778 血钙/(mmol/L) 2.14(2.10,2.28) 2.16(2.02,2.28) -1.13 0.256 血镁/(mmol/L) 0.89(0.8,1) 0.93(0.84,1.03) -0.21 0.826 血钾/(mmol/L) 4.5(3.8,5.2) 4.25(3.7,5.2) -2.54 0.011 CK-MB/(U/L) 274.6(174.4,372.3) 273.4(178.8,383.9) -1.13 0.257 TG/(mmol/L) 1.225(0.99,1.43) 1.35(1.17,1.62) -0.75 0.451 TC/(mmol/L) 5.175(4.1,6.1) 5.26(4.3,6.2) -7.02 < 0.001 HDL-C/(mmol/L) 1.06(0.93,1.18) 1.05(0.93,1.19) -0.95 0.340 LDL-C/(mmol/L) 2.515(2.22,2.81) 2.52(2.28,2.83) -0.01 0.991 NT-proBNP/(pg/mL) 1 151(735,1 586) 1 461(875,2 290) -0.90 0.366 CRP/(mg/dL) 6.6(4.5,9.05) 6.53(3.8,9.7) -5.61 < 0.001 LVEF/% 48(44,51) 41(35,45) -0.28 < 0.001 发病时长/h 5(3,7) 6.5(5,8) -11.67 0.777 1 mmHg=0.133 kPa。 表 2 各变量的截断值
Table 2. Cut-off values of variables
变量 AUC 截断值 灵敏度/% 特异度/% P 年龄 0.895 57岁 91.33 69.43 < 0.000 1 心率 0.959 90次/min 76.67 100.00 < 0.000 1 LVEF 0.809 41% 56.00 88.69 < 0.000 1 -
[1] Risgaard B, Nielsen JB, Jabbari R, et al. Prior myocardial infarction in the young: predisposes to a high relative risk but low absolute risk of a sudden cardiac death[J]. Europace, 2013, 15(1): 48-54. doi: 10.1093/europace/eus190
[2] Kosmidou I, Embacher M, McAndrew T, et al. Early Ventricular Tachycardia or Fibrillation in Patients With ST Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention and Impact on Mortality and Stent Thrombosis(from the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial)[J]. Am J Cardiol, 2017, 120(10): 1755-1760. doi: 10.1016/j.amjcard.2017.07.080
[3] Wijesekera VA, Mullany DV, Tjahjadi CA, et al. Routine angiography in survivors of out of hospital cardiac arrest with return of spontaneous circulation: a single site registry[J]. BMC Cardiovasc Disord, 2014, 14: 30. doi: 10.1186/1471-2261-14-30
[4] 翟虎, 张纯溪, 王禹, 等. 急性ST段抬高型心肌梗死患者急诊介入前心室颤动预测模型构建及验证[J]. 临床心血管病杂志, 2023, 39(6): 459-465. doi: 10.13201/j.issn.1001-1439.2023.06.010
[5] Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction[J]. Nat Rev Cardiol, 2012, 9(11): 620-633. doi: 10.1038/nrcardio.2012.122
[6] Sawada H, Ando H, Takashima H, et al. Epidemiological Features and Clinical Presentations of Acute Coronary Syndrome in Young Patients[J]. Intern Med, 2020, 59(9): 1125-1131. doi: 10.2169/internalmedicine.4138-19
[7] Wu J, Zhang H, Li L, et al. A nomogram for predicting overall survival in patients withlow-grade endometrial stromal sarcoma: A population-based analysis[J]. Cancer Commun(Lond), 2020, 40(7): 301-312.
[8] 孙瑞雪, 周强, 周志明, 等. 心脏移植早期死亡的影响因素及预测模型构建[J]. 中华器官移植杂志, 2022, 43(12): 723-729. doi: 10.3760/cma.j.cn421203-20220816-00204
[9] Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American HeartAssociation Task Force on Clinical Practice Guidelines[J]. Circulation, 2019, 140(11): e563-e595.
[10] Ashok D, Papanicolaou K, Sidor A, et al. Mitochondrial membrane potential instability on reperfusion after ischemia does not depend on mitochondrial Ca(2+)uptake[J]. J Biol Chem, 2023, 299(6): 104708. doi: 10.1016/j.jbc.2023.104708
[11] Takada T, Shishido K, Hayashi T, et al. Impact of Late Ventricular Arrhythmias on Cardiac Mortality in Patients with Acute Myocardial Infarction[J]. J Interv Cardiol, 2019: 5345178.
[12] Fishman GI, Chugh SS, Dimarco JP, et al. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm SocietyWorkshop[J]. Circulation, 2010, 122(22): 2335-2348. doi: 10.1161/CIRCULATIONAHA.110.976092
[13] Misumida N, Kobayashi A, Saeed M, et al. Association Between Preinfarction Angina andAngiographic Findings in Non-ST-Segment Elevation Myocardial Infarction[J]. Clin Cardiol, 2015, 38(9): 535-541. doi: 10.1002/clc.22439
[14] Ng FS, Shadi IT, Peters NS, et al. Selective heart rate reduction with ivabradine slows ischaemia-induced electrophysiological changes and reduces ischaemia-reperfusion-induced ventricular arrhythmias[J]. J Mol Cell Cardiol, 2013, 59: 67-75. doi: 10.1016/j.yjmcc.2013.02.001
[15] Vaillant F, Dehina L, Mazzadi A, et al. Heart rate reduction with ivabradine increases ischaemia-induced ventricular fibrillation threshold: role of myocyte structure and myocardial perfusion[J]. Resuscitation, 2011, 82(8): 1092-1099. doi: 10.1016/j.resuscitation.2011.03.032
[16] Schmidt G, Malik M, Barthel P, et al. Heart-rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction[J]. Lancet, 1999, 353(9162): 1390-1396. doi: 10.1016/S0140-6736(98)08428-1
[17] Gheeraert PJ, Henriques JP, De Buyzere ML, et al. Preinfarction angina protects against out-of-hospital ventricular fibrillation in patients with acute occlusion of the left coronary artery[J]. J Am Coll Cardiol, 2001, 38(5): 1369-1374. doi: 10.1016/S0735-1097(01)01561-3
[18] Janzon E, Hedblad B, Berglund G, et al. Tobacco and myocardial infarction in middle-aged women: a study of factors modifying the risk[J]. J Intern Med, 2004, 256(2): 111-118. doi: 10.1111/j.1365-2796.2004.01346.x
[19] Rasmussen T, Frestad D, Kober L, et al. Development and progression of coronary artery calcification in long-term smokers: adverse effects of continued smoking[J]. J Am Coll Cardiol, 2013, 62(3): 255-257. doi: 10.1016/j.jacc.2013.04.013
[20] Ghaisas MM, Dandawate PR, Zawar SA, et al. Antioxidant, antinociceptive and anti-inflammatory activities of atorvastatin and rosuvastatin in various experimental models[J]. Inflammopharmacology, 2010, 18(4): 169-177. doi: 10.1007/s10787-010-0044-6
-




 下载:
下载: