Clinical efficacy of transcatheter tricuspid valve replacement for isolated severe tricuspid regurgitation after left-side valve surgery
-
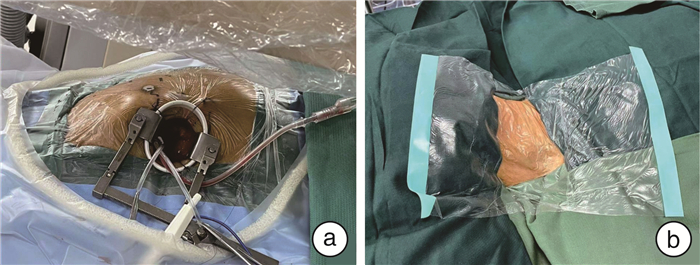
摘要: 目的 评估经导管三尖瓣置换术治疗左心瓣膜术后重度三尖瓣反流的临床疗效。方法 2020年10月—2022年10月,共7例左心瓣膜术后重度三尖瓣反流患者于广东省人民医院(广东省心血管病研究所)接受经导管三尖瓣置换术治疗,其中5例采用Lux-Valve装置(经右心房径路),2例采用Lux-Valve Plus装置(经颈静脉径路)。收集患者住院诊疗及随访资料,总结和分析临床效果。结果 患者年龄为(65.1±8.8)岁,以女性居多(5/7),5例(71.4%)患者伴随下肢水肿等典型右心衰竭症状;患者术前三尖瓣反流均达4+及以上,CRS评分中值8.0分,Child-Pugh评分均值7.3分,肺动脉收缩压(38.9±10.1) mmHg(1 mmHg=0.133 kPa),右室面积变化分数(42.3±3.6)%,三尖瓣环收缩期位移(15.6±1.8) mm。术中顺利置入经导管三尖瓣装置,术后即刻器械成功率、手术成功率达100%(即刻三尖瓣反流改善至1+瓣周漏2例,5例无反流),无死亡、中转开胸、瓣膜移位等并发症。平均随访(14.2±10.2)个月,期间所有患者的人工三尖瓣瓣膜装置功能良好,仅1例患者残余1+的瓣周漏,与术前比较仍显著改善(P < 0.001),无中度以上肺动脉高压、肝静脉逆流、再次手术或因心力衰竭住院;NYHA心功能等级均恢复至Ⅱ级。结论 在右心衰竭早期对左心瓣膜术后重度三尖瓣反流患者行经导管三尖瓣置换术是安全可靠的,早中期临床结果优异,重度三尖瓣反流得到显著改善。未来仍需更进一步研究明确经导管三尖瓣置换系统对此类患者的疗效和优势。Abstract: Objective To evaluate the clinical efficacy of transcatheter tricuspid valve replacement (TTVR) for isolated severe tricuspid regurgitation following left-side valve surgery.Methods From October 2020 to October 2022, seven patients with isolated severe tricuspid regurgitation after left-side valve surgery underwent TTVR at Guangdong Provincial People's Hospital (Guangdong Institute of Cardiovascular Diseases). Among them, five were treated with the Lux-Valve device (via the right atrial pathway), and two with the Lux-Valve Plus device (via the jugular vein pathway). Inpatient treatment and follow-up data were collected for summarizing and analyzing clinical outcomes.Results The mean age of the patients was (65.1±8.8)years, with a female predominance (5/7). Five patients (71.4%) exhibited typical right heart failure symptoms such as lower limb edema. All patients had preoperative tricuspid regurgitation of 4+ or greater, a median CRS score of 8.0, average Child-Pugh score of 7.3, pulmonary artery systolic pressure of (38.9±10.1)mmHg, fractional area change of right ventricular (42.3±3.6)%, tricuspid annular plane systolic excursion 15.6±1.8 mm. Intraoperatively, the transcatheter tricuspid valve device was successfully placed, with an immediate postoperative device success rate and surgical success rate of 100% (immediate tricuspid regurgitation improvement, 2 cases of 1+ perivalvular leakage, 5 cases with no regurgitation). No complications such as death, thoracotomy conversion, or valve displacement occurred. The mean follow-up time was (14.2±10.2) months, during which the prosthetic tricuspid valve devices all functioned well. Only one patient had residual 1+ perivalvular leakage, significantly improved compared to preoperative conditions (P < 0.001). There were no instances of more than moderate pulmonary hypertension, hepatic venous regurgitation, reoperation, or hospitalization for heart failure. All NYHA cardiac function classes recovered to ClassⅡ.Conclusion Transcatheter tricuspid valve replacement is safe and reliable in patients with severe tricuspid regurgitation after left-side valve surgery at the early stage of right heart failure. It demonstrates excellent early and mid-term clinical outcomes with a significant improvement in severe tricuspid regurgitation. Future research on the specific effects and advantages of TTVR for these patients is still needed.
-

-
表 1 7例患者的基线资料
Table 1. Baseline data of 7 patients
编号 性别 年龄/岁 心力衰竭症状 瓣膜手术史/间隔年限 风湿性心脏病 CRS评分 Child-Pugh评分/分级 NYHA分级 置入人工瓣膜 01 女 68 气促、腹胀、下肢水肿 MVR+TVP/17 是 8 7/B Ⅲ Lux-Valve 02 女 50 胸闷、下肢水肿 MVR/20 是 8 6/A Ⅲ Lux-Valve 03 女 64 胸闷、晕厥 MVR/17 否 9 8/B Ⅲ Lux-Valve 04 女 68 下肢水肿、气促 MVR/13 是 8 6/A Ⅲ Lux-Valve 05 男 58 气促 DVR+TVP/12 否 9 8/B Ⅲ Lux-Valve 06 男 72 下肢水肿、腹水增多、脾大 DVR+TVP/9 是 8 9/B Ⅲ Lux-Valve Plus 07 女 76 下肢水肿 MVR+TVP/21 否 10 7/B Ⅳ Lux-Valve Plus MVR:二尖瓣置换;AVR:主动脉瓣置换;DVR:双瓣(二尖瓣+主动脉瓣)置换;TVP:三尖瓣成形。 表 2 7例患者术前及最新随访期的心脏超声资料比较
Table 2. Preoperative and latest follow-up cardiac ultrasound data of 7 patients
例(%), X±S 项目 术前(7例) 随访(7例) P值 TR等级 0.001 5+ 1(14.3) 0 4+ 6(85.7) 0 3+ 0 0 2+ 0 0 1+ 0 1(14.3) 0 0 6(85.7) PASP 30~55 mmHg 6(85.7) 0 0.005 左心房容积/mL 217.8±131.1 157.8±70.5 0.102 右心房容积/mL 117.0±27.9 83.0±10.4 0.025 左心室舒张末期容积/mL 69.4±18.4 64.8±21.4 0.457 右心室舒张末期容积/mL 82.8±55.4 57.0±25.8 0.239 LVEF/% 61.0±6.4 65.3±3.9 0.067 FAC/% 42.3±3.6 40.9±5.4 0.626 TAPSE/mm 15.6±1.8 15.7±2.5 0.940 表 3 TTVR手术结果
Table 3. TTVR results
X±S 项目 总体(7例) Lux-Valve(5例) Lux-Valve(2例) P值 手术成功率/% 100 100 100 - 器械成功率/% 100 100 100 - 出血量/mL 167.1±101.1 204.0±95.3 75.0±35.4 0.049 机械通气 < 24 h 7(100) 5(100) 2(100) - 肺炎/例(%) 2(28.6) 1(20.0) 1(50.0) 1 -
[1] Braunwald NS, Ross J Jr, Morrow AG. Conservative management of tricuspid regurgitation in patients undergoing mitral valve replacement[J]. Circulation, 1967, 35(4 Suppl): I63-69.
[2] Mangieri A, Montalto C, Pagnesi M, et al. Mechanism and Implications of the Tricuspid Regurgitation: From the Pathophysiology to the Current and Future Therapeutic Options[J]. Circ Cardiovasc Interv, 2017, 10(7): e005043. doi: 10.1161/CIRCINTERVENTIONS.117.005043
[3] Desai RR, Vargas Abello LM, Klein AL, et al. Tricuspid regurgitation and right ventricular function after mitral valve surgery with or without concomitant tricuspid valve procedure[J]. J Thorac Cardiovasc Surg, 2013, 146(5): 1126-1132.e10. doi: 10.1016/j.jtcvs.2012.08.061
[4] Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease[J]. Eur Heart J, 2022, 43(7): 561-632. doi: 10.1093/eurheartj/ehab395
[5] Hahn RT, Thomas JD, Khalique OK, et al. Imaging Assessment of Tricuspid Regurgitation Severity[J]. JACC Cardiovasc Imaging, 2019, 12(3): 469-490. doi: 10.1016/j.jcmg.2018.07.033
[6] Izumi C. Tricuspid regurgitation following left-sided valve surgery: echocardiographic evaluation and optimal timing of surgical treatment[J]. J Echocardiogr, 2015, 13(1): 15-19. doi: 10.1007/s12574-014-0236-y
[7] Hwang HY, Kim KH, Kim KB, et al. Reoperations after tricuspid valve repair: re-repair versus replacement[J]. J Thorac Dis, 2016, 8(1): 133-139.
[8] Jeganathan R, Armstrong S, Al-Alao B, et al. The risk and outcomes of reoperative tricuspid valve surgery[J]. Ann Thorac Surg, 2013, 95(1): 119-124. doi: 10.1016/j.athoracsur.2012.08.058
[9] Yang L, Zhou K, Yang YC, et al. Outcomes of redo-isolated tricuspid valve surgery after left-sided valve surgery[J]. J Card Surg, 2021, 36(9): 3060-3069. doi: 10.1111/jocs.15694
[10] 宁小平, 安朝, 乔帆, 等. 经导管介入三尖瓣置换装置LuX-Valve在重度三尖瓣反流治疗中的应用[J]. 中华心血管病杂志, 2021, 49(5): 455-460.
-




 下载:
下载: