Meta-analysis of the relationship between homocysteine level and metabolic cardiovascular disease
-
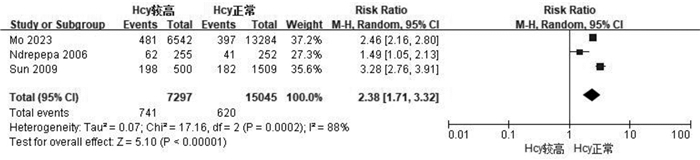
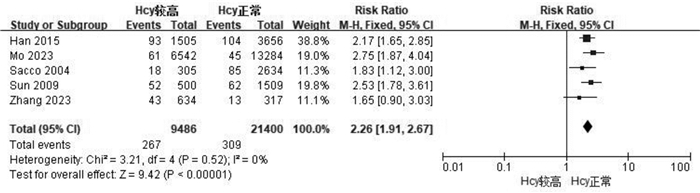
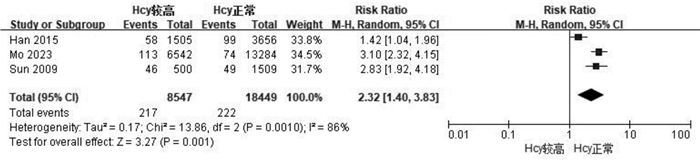
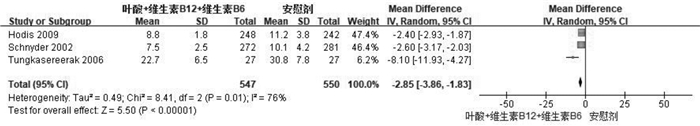
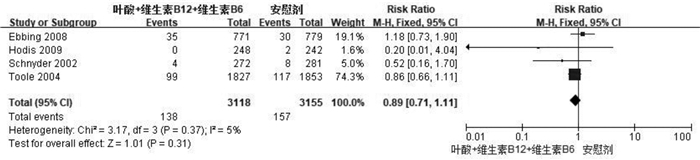
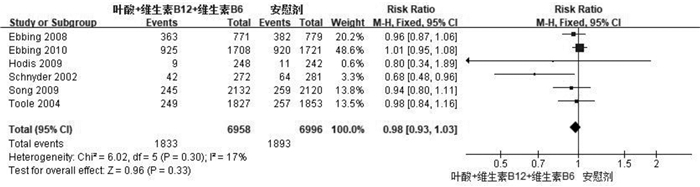
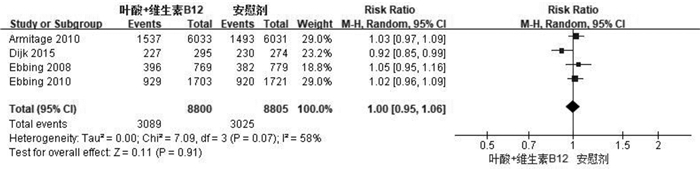
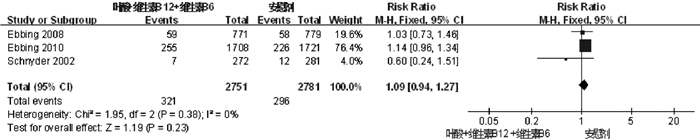
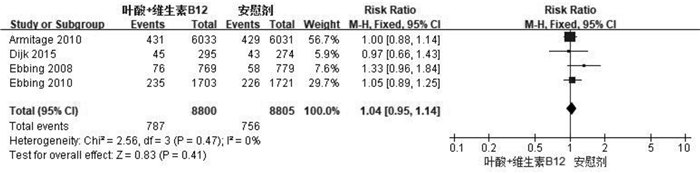
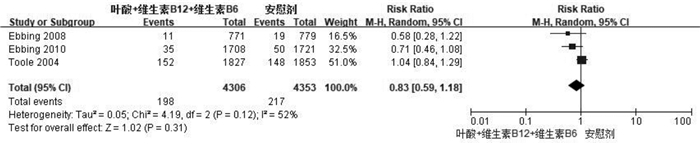
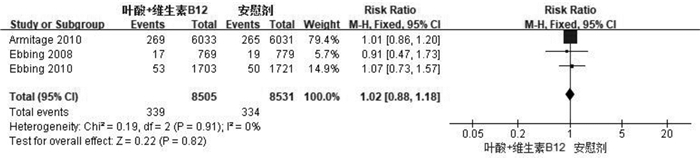
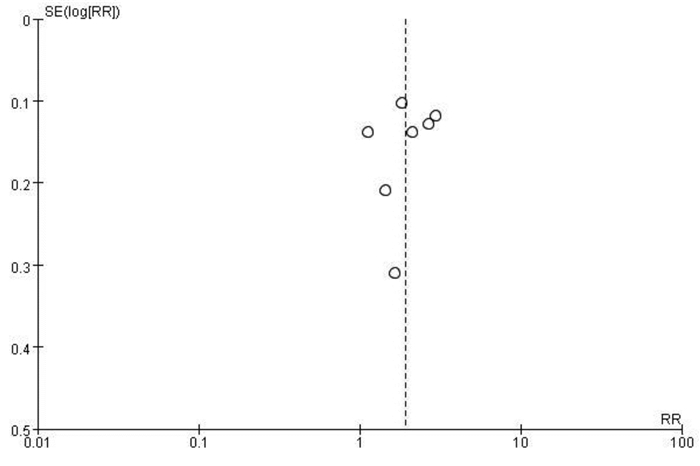
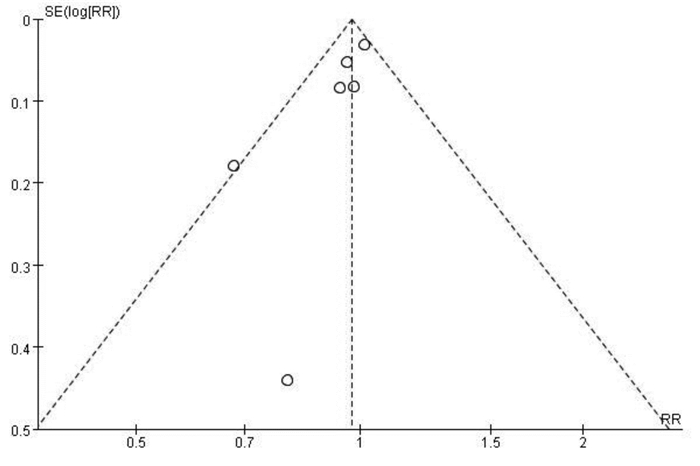
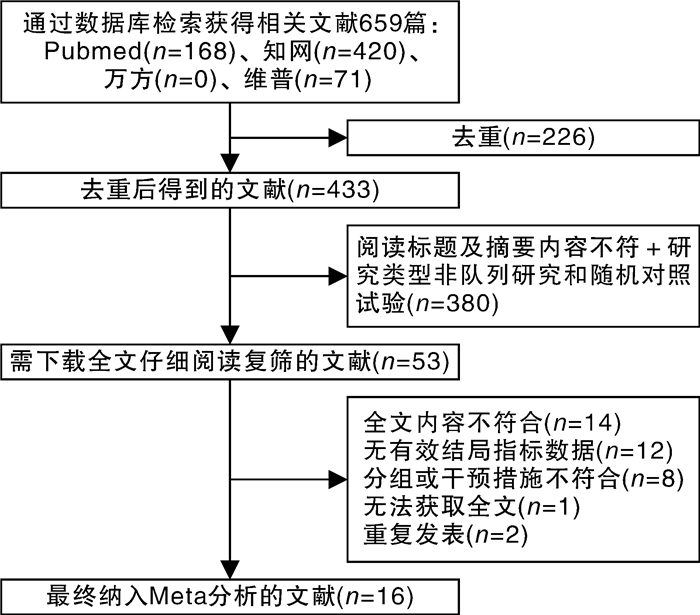
摘要: 目的 通过meta分析评估同型半胱氨酸(homocysteine,Hcy)水平与代谢性心血管疾病发生及死亡风险的相关性。方法 计算机检索Pubmed、中国知网(CNKI)、万方数据库和维普数据库,检索时限为建库至2023年7月24日。经过文献筛选、资料提取和质量评价,采用RevMan 5.3软件进行meta分析。结果 共纳入16篇文献,其中7篇为队列研究,9篇为随机对照试验(randomized controlled trial,RCT)。队列研究meta分析结果显示,与Hcy水平正常者相比,Hcy水平较高者全因死亡率(RR=2.38,95%CI:1.71~3.32)、代谢性心血管疾病(RR=1.91,95%CI:1.46~2.49)、卒中(RR=2.26,95%CI:1.91~2.67)和冠心病(RR=2.32,95%CI:1.40~3.83)的发生/死亡风险增加;RCT研究meta分析结果显示,叶酸联合B族维生素干预可降低人体内Hcy水平(RR=-2.85,95%CI:-3.86~-1.83),但试验组和对照组全因死亡率、代谢性心血管疾病、心肌梗死和卒中的发生/死亡风险均无统计学意义(均P>0.05)。结论 队列研究结果显示,体内Hcy水平升高会增加代谢性心血管疾病的发生风险和全因死亡风险。RCT结果显示,叶酸联合B族维生素干预虽然能降低体内Hcy水平,但远期内并不能观测到对代谢性心血管疾病的影响。Abstract: Objective The study was aimed to evaluate the correlation between homocysteine(Hcy) levels and the risk of metabolic cardiovascular diseases and death through meta-analysis.Methods Pubmed, CNKI, Wanfang Database, and VIP Database were searched by computer to collect literature till July 24th, 2023. After literature screening, data extraction, and quality evaluation, meta-analysis was conducted using RevMan 5.3 software.Results A total of 16 articles were included, of which 7 were cohort studies and 9 were RCTs. The meta-analysis results from cohort studies showed that comparing with those with normal Hcy levels, those with higher Hcy levels had a higher risk of all-cause mortality(RR=2.38, 95%CI1.71-3.32), metabolic cardiovascular diseases(RR=1.91, 95%CI1.46-2.49), stroke(RR=2.26, 95%CI1.91-2.67), and coronary heart diseases(RR=2.32, 95%CI1.40-3.83). The meta-analysis results from RCTs showed that folic acid combined with B vitamins intervention could reduce Hcy levels in the human body(RR=-2.85, 95%CI-3.86--1.83), but there were no significant differences in the incidence of all-cause mortality, metabolic cardiovascular diseases, myocardial infarction and stroke in the experimental and control groups(P > 0.05).Conclusion The results of cohort studies indicate that an increase in Hcy levels in the body over a period of time increases the risk of metabolic cardiovascular diseases and all-cause mortality. The results of RCTs indicate that although exogenous folic acid combined with B vitamins intervention can reduce Hcy levels in the body for a certain period of time, while the long-term impact on metabolic cardiovascular diseases cannot be observed.
-

-
表 1 纳入队列研究文献的基本特征
Table 1. Basic characteristics of included cohort studies
纳入研究 国家 研究对象特征 随访时间/年 年龄/岁 例数 结局指标 Hcy水平较高(>15 μmol/L) Hcy水平正常(≤15 μmol/L) Han 2015[12] 中国 原发性高血压患者 2.7 58.52±12.19 1505 3656 ③④⑤ Mo 2023[13] 中国 无冠心病、卒中、癌症者 5.69 62.93±8.25 6542 13284 ①②③ ④⑤ Ndrepepa 2006[6] 德国 2型糖尿病和冠状动脉疾病患者 4 59.9~77.0 255 252 ①②③ Sacco 2004[14] 美国 未患过卒中者 4 68.9±10.2 305 2634 ③④ Sun 2009[5] 中国 未患过卒中、心血管疾病和癌症者 11.95 Q1:51.1±9.1
Q2:55.8±10.3
Q3:60.0±10.7
Q4:64.2±11.4500 1509 ①③ ④⑤ Xiao 2013[15] 中国 接受冠状动脉造影的患者 3 21~87 249 754 ③ Zhang 2023[16] 中国 急性缺血性卒中和H型高血压患者 1 65.5±11.7 634 317 ③④ 注:结局指标:①全因死亡;②代谢性心血管疾病死亡;③代谢性心血管疾病发生;④卒中;⑤冠心病。 表 2 干预措施为叶酸+维生素B12+维生素B6的RCT研究文献的基本特征
Table 2. Basic characteristics of included RCTs(The intervention measure includes folic acid, vitamin B12 and vitamin B6)
纳入研究 国家 研究对象特征 随访时间/年 平均年龄/岁 例数 干预措施/mg 结局指标 试验组 对照组 试验组 对照组 试验组 对照组 Ebbing 2008[10] 挪威 疑似冠脉瓣狭窄而接受冠状动脉造影和(或)主动脉瓣造影者 3.2 61.7±10.3 62.0±9.9 771 779 0.8叶酸+0.4维生素B12+40维生素B6 安慰剂 ①③ ④⑤ Ebbing 2010[17] 挪威 缺血性心脏病患者 6.5 62.7±11.2 62.3±10.7 1708 1721 0.8叶酸+0.4维生素B12+40维生素B6 安慰剂 ②③ ④⑤ Hodis 2009[8] 美国 无CVD临床体征/症状者 3.1 61.7±10.1 61.1±9.6 248 242 5叶酸+0.4维生素B12+50维生素B6 安慰剂 ①③ Schnyder 2002[18] 瑞士 冠状动脉狭窄患者 1 63.4±10.6 61.8±11.0 272 281 1叶酸+0.4维生素B12+10维生素B6 安慰剂 ①② ③④ Song 2009[11] 美国 有CVD病史或危险因素大于等于3个者 7.3 63.1±8.9 62.9±8.9 2132 2120 2.5叶酸+1维生素B12+50维生素B6 安慰剂 ③ Toole 2004[19] 美国、加拿大、英国 急性缺血性卒中患者 2 66.4±10.8 66.2±10.8 1827 1853 2.5叶酸+0.4维生素B12+25维生素B6 0.02叶酸+0.006维生素B12+0.2维生素B6 ①③⑤ Tungkasereerak 2006[20] 泰国 同型半胱氨酸>10 mmol/L者 0.5 55.86± 13.44 55.17± 13.86 27 27 15叶酸+1维生素B12+50维生素B6 5叶酸 ⑥ 注:结局指标:①全因死亡;②代谢性心血管疾病死亡;③代谢性心血管疾病发生;④心肌梗死;⑤卒中;⑥颈动脉IMT变化。 表 3 干预措施为叶酸+维生素B12的RCT研究文献的基本特征
Table 3. Basic characteristics of included RCTs(The intervention measure includes folic acid and vitamin B12)
纳入研究 国家 研究对象特征 随访时间/年 平均年龄/岁 例数 干预措施/mg 结局指标 试验组 对照组 试验组 对照组 Armitage 2010[21] 英国 有心肌梗死病史者 6.7 64.2±8.9 6033 6031 2叶酸+1维生素B12 安慰剂 ①②③ ④⑤ Dijk 2015[22] 荷兰 同型半胱氨酸12~50 μmol/L者 2 试验组72.5±5.8对照组72.5±5.3 295 274 0.4叶酸+0.5维生素B12 安慰剂 ③④⑥ Ebbing 2008[10] 挪威 疑似冠脉瓣狭窄而接受冠状动脉造影和(或)主动脉瓣造影者 3.2 试验组61.3±10.0对照组62.0±9.9 769 779 0.8叶酸+0.4维生素B12 安慰剂 ①③ ④⑤ Ebbing 2010[17] 挪威 缺血性心脏病患者 6.5 试验组62.3±10.9对照组62.3±10.7 1703 1721 0.8叶酸+0.4维生素B12 安慰剂 ②③ ④⑤ 注:结局指标:①全因死亡;②代谢性心血管疾病死亡;③代谢性心血管疾病发生;④心肌梗死;⑤卒中;⑥颈动脉内膜中层厚度变化。 -
[1] Hu Y, Wang X, Huan J, et al. Effect of dietary inflammatory potential on the aging acceleration for cardiometabolic disease: A population-based study[J]. Front Nutr, 2022, 9: 1048448. doi: 10.3389/fnut.2022.1048448
[2] Chakaroun RM, Olsson LM, Bäckhed F. The potential of tailoring the gut microbiome to prevent and treat cardiometabolic disease[J]. Nat Rev Cardiol, 2023, 20(4): 217-235. doi: 10.1038/s41569-022-00771-0
[3] Saklayen MG. The Global Epidemic of the Metabolic Syndrome[J]. Current hypertension reports, 2018, 20(2): 12. doi: 10.1007/s11906-018-0812-z
[4] Lu J, Chen K, Chen W, et al. Association of serum homocysteine with cardiovascular and all-cause mortality in adults with diabetes: a prospective cohort study[J]. Oxid Med Cell Longev, 2022, 2022: 2156483.
[5] Sun Y, Chien KL, Hsu HC, et al. Use of serum homocysteine to predict stroke, coronary heart disease and death in ethnic Chinese. 12-year prospective cohort study[J]. Circ J, 2009, 73(8): 1423-1430. doi: 10.1253/circj.CJ-08-1077
[6] Ndrepepa G, Kastrati A, Braun S, et al. A prospective cohort study of predictive value of homocysteine in patients with type 2 diabetes and coronary artery disease[J]. Clin Chim Acta, 2006, 373(1-2): 70-76. doi: 10.1016/j.cca.2006.05.011
[7] 马娟, 严宁, 马学平, 等. Hcy联合CRP/Alb比值对STEMI合并代谢综合征患者急诊PCI术后无复流的预测价值[J]. 临床心血管病杂志, 2022, 38(4): 308-314. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.04.011
[8] Hodis HN, Mack WJ, Dustin L, et al. High-dose B vitamin supplementation and progression of subclinical atherosclerosis: a randomized controlled trial[J]. Stroke, 2009, 40(3): 730-736. doi: 10.1161/STROKEAHA.108.526798
[9] Huang T, Chen Y, Yang B, et al. Meta-analysis of B vitamin supplementation on plasma homocysteine, cardiovascular and all-cause mortality[J]. Clinical nutrition(Edinburgh, Scotland), 2012, 31(4): 448-454. doi: 10.1016/j.clnu.2011.01.003
[10] Ebbing M, Bleie Ø, Ueland PM, et al. Mortality and cardiovascular events in patients treated with homocysteine-lowering B vitamins after coronary angiography: a randomized controlled trial[J]. JAMA, 2008, 300(7): 795-804. doi: 10.1001/jama.300.7.795
[11] Song Y, Cook NR, Albert CM, et al. Effect of homocysteine-lowering treatment with folic Acid and B vitamins on risk of type 2 diabetes in women: a randomized, controlled trial[J]. Diabetes, 2009, 58(8): 1921-1928. doi: 10.2337/db09-0087
[12] Han L, Wu Q, Wang C, et al. Homocysteine, ischemic stroke, and coronary heart disease in hypertensive patients: a population-based, prospective cohort study[J]. Stroke, 2015, 46(7): 1777-1786. doi: 10.1161/STROKEAHA.115.009111
[13] Mo T, Long P, Wang Y, et al. Genetic susceptibility, homocysteine levels, and risk of all-cause and cause-specific mortality: A prospective cohort study[J]. Clin Chim Acta, 2023, 538: 1-8. doi: 10.1016/j.cca.2022.11.001
[14] Sacco RL, Anand K, Lee H, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the Northern Manhattan Study[J]. Stroke, 2004, 35(10): 110.
[15] Xiao Y, Zhang Y, Wang M, et al. Plasma S-adenosylhomocysteine is associated with the risk of cardiovascular events in patients undergoing coronary angiography: a cohort study[J]. Am J Clin Nutr, 2013, 98(5): 1162-1169. doi: 10.3945/ajcn.113.058727
[16] Zhang D, Liu Z, Guo W, et al. Serum homocysteine level is an independent risk factor for 1-year stroke recurrence in patients with acute ischemic stroke and H-type hypertension: results from the Xi'an stroke registry study of China[J]. Front Neurol, 2023, 14: 1161318. doi: 10.3389/fneur.2023.1161318
[17] Ebbing M, Bønaa KH, Arnesen E, et al. Combined analyses and extended follow-up of two randomized controlled homocysteine-lowering B-vitamin trials[J]. J Int Med, 2010, 268(4): 110.
[18] Schnyder G, Roffi M, Flammer Y, et al. Effect of homocysteine-lowering therapy with folic acid, vitamin B12, and vitamin B6 on clinical outcome after percutaneous coronary intervention: the Swiss Heart study: a randomized controlled trial[J]. JAMA, 2002, 288(8): 973-979. doi: 10.1001/jama.288.8.973
[19] Toole JF, Malinow MR, Chambless LE, et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention(VISP)randomized controlled trial[J]. JAMA, 2004, 291(5): 110.
[20] Tungkasereerak P, Ong-ajyooth L, Chaiyasoot W, et al. Effect of short-term folate and vitamin B supplementation on blood homocysteine level and carotid artery wall thickness in chronic hemodialysis patients[J]. J Med Assoc Thai, 2006, 89(8): 1187-1193.
[21] Armitage JM, Bowman L, Clarke RJ, et al. Effects of homocysteine-lowering with folic acid plus vitamin B12 vs placebo on mortality and major morbidity in myocardial infarction survivors: a randomized trial[J]. JAMA, 2010, 303(24): 2486-2494. doi: 10.1001/jama.2010.840
[22] van Dijk SC, Enneman AW, Swart KM, et al. Effects of 2-year vitamin B12 and folic acid supplementation in hyperhomocysteinemic elderly on arterial stiffness and cardiovascular outcomes within the B-PROOF trial[J]. J Hypertens, 2015, 33(9): 1897-1906.
[23] Moretti R, Caruso P. The controversial role of homocysteine in neurology: from labs to clinical practice[J]. Int J Mol Sci, 2019, 20(1): 231.
[24] Guieu R, Ruf J, Mottola G. Hyperhomocysteinemia and cardiovascular diseases[J]. Ann Bio Clin, 2022, 80(1): 7-14.
[25] Song S, Song BM, Park H. Associations of serum folate and homocysteine concentrations with all-cause, cardiovascular disease, and cancer mortality in men and women in korea: the cardiovascular disease association study[J]. J Nut, 2023, 153(3): 760-770.
[26] du Plessis JP, Lammertyn L, Schutte AE, et al. H-type hypertension among black south africans and the relationship between homocysteine, its genetic determinants and estimates of vascular function[J]. J Cardiovasc Develop Dis, 2022, 9(12): 447.
[27] Chrysant SG, Chrysant GS. The current status of homocysteine as a risk factor for cardiovascular disease: a mini review[J]. Exp Rev Cardiovasc Ther, 2018, 16(8): 559-565.
[28] Mohan A, Kumar R, Kumar V, et al. Homocysteine, Vitamin B12 and folate level: possible risk factors in the progression of chronic heart and kidney disorders[J]. Curr Cardiol Revs, 2023, 19(4): e028900323.
-




 下载:
下载: