TAPSE/PASP evaluates the prognosis of elderly patients with heart failure with preserved ejection fraction
-
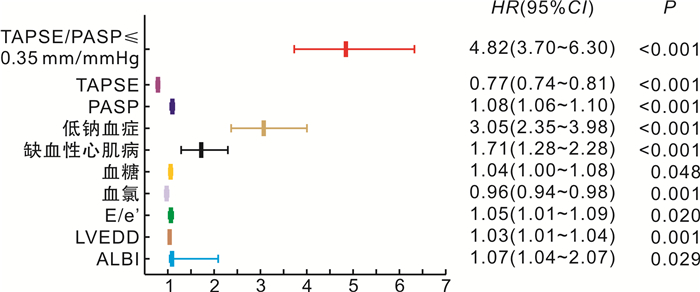
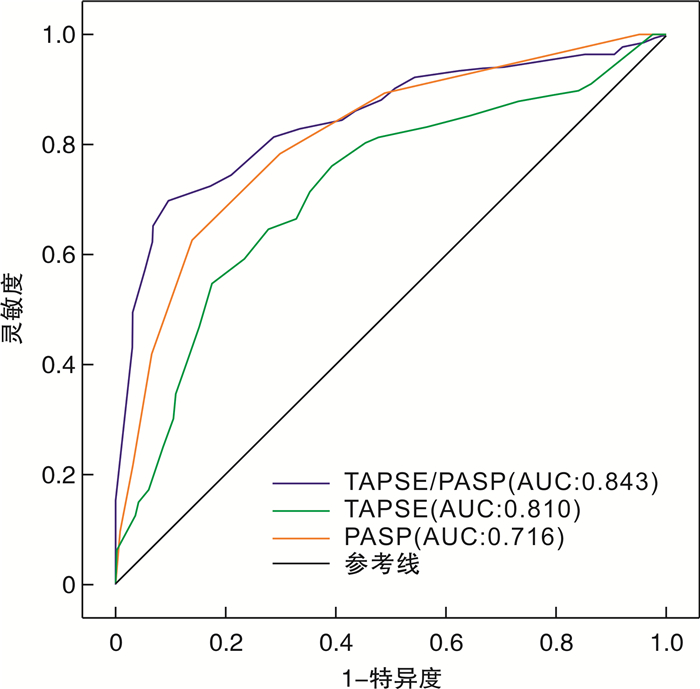
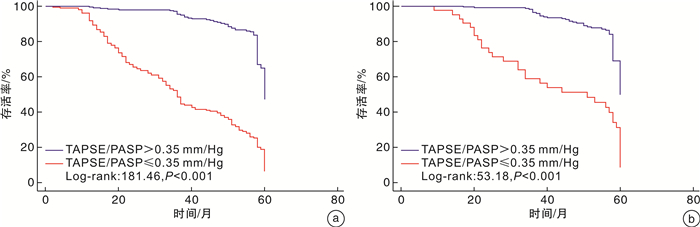
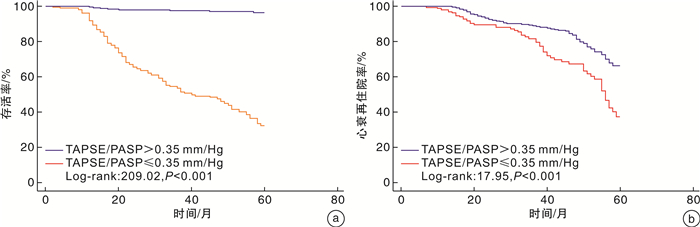
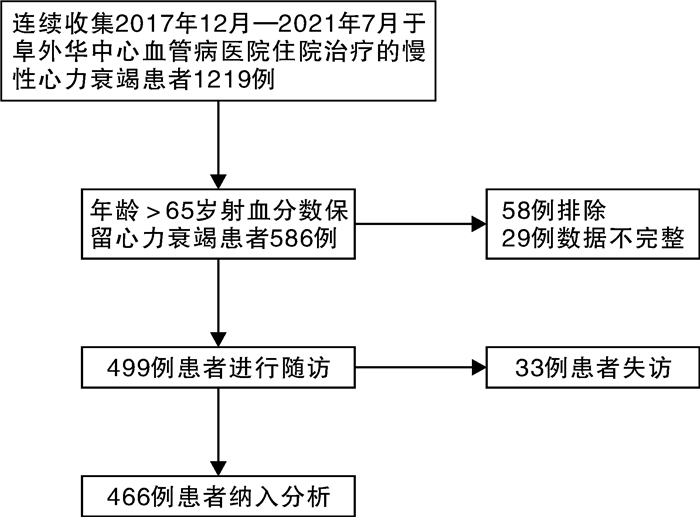
摘要: 目的 三尖瓣环收缩期位移(tricuspid annular plane systolic excursion,TAPSE)与肺动脉收缩压(pulmonary artery systolic pressure,PASP)的比值是评估右心室-肺动脉耦联的重要指标。本研究评估TAPSE/PASP对老年射血分数保留心力衰竭(heart failure with preserved ejection fraction,HFpEF)患者的预后价值。方法 回顾性分析2017年12月—2021年7月于阜外华中心血管病医院住院的年龄>65岁HFpEF患者466例,以全因死亡和心力衰竭再住院作为复合终点,2022年11月—2022年12月完成随访。Cox比例风险回归模型分析终点事件的危险因素,受试者工作特征曲线(ROC)分析TAPSE、PASP及TAPSE/PASP对复合终点的预测价值。采用Kaplan-Meier生存曲线比较组间的累积生存率。结果 多因素Cox回归模型显示,TAPSE/PASP≤0.35 mm/mmHg、低钠血症、血糖、缺血性心肌病为老年HFpEF患者发生复合终点事件的独立预测因子。ROC曲线显示,TAPSE/PASP、TAPSE及PASP对老年HFpEF患者发生全因死亡和心力衰竭再住院的预测AUC分别为0.843(95%CI 0.807~0.879,P<0.001)、0.810(95%CI 0.770~0.849,P<0.001)、0.716(95%CI 0.669~0.764,P<0.001)。Kaplan-Meier生存曲线显示,TAPSE/PASP≤0.35 mm/mmHg组患者的累积生存率显著低于TAPSE/PASP>0.35 mm/mmHg组(P<0.001)。结论 TAPSE/PASP是老年HFpEF患者全因死亡和心力衰竭再住院的独立预测因子。TAPSE/PASP>0.35 mm/mmHg时生存率较高。
-
关键词:
- 右心室-肺动脉耦联 /
- 三尖瓣环收缩期位移 /
- 肺动脉收缩压 /
- 射血分数保留型心力衰竭
Abstract: Objective The ratio of tricuspid annular systolic plane excursion(TAPSE) to pulmonary artery systolic pressure(PASP) is an important index for evaluating right ventricle-pulmonary artery coupling. The aim of this study was to evaluate the prognostic value of TAPSE/PASP in elderly patients with heart failure with preserved ejection fraction(HFpEF).Methods A total of 466 HFpEF patients aged>65 years who were hospitalized Fuwai Huazhong Cardiovascular Hospital from December 2017 to July 2021 were retrospectively analyzed. All-cause death and rehospitalization for heart failure were used as the composite endpoint. Follow-up was completed from November 2022 to December 2022. Kaplan-Meier survival analysis curves were used to compare cumulative survival between groups. Cox proportional hazards regression models were used to analyze risk factors for endpoint events; and receiver operating characteristic curves(ROC) were used to analyze the predictive value of TAPSE/PASP, TAPSE, and PASP for composite endpoint events.Results Multivariate Cox regression models showed that TAPSE/PASP≤0.35 mm/mmHg, hyponatremia, blood glucose, and ischemic cardiomyopathy were independent predictors of composite endpoint events in elderly HFPEF patients. ROC curves showed that TAPSE/PASP was superior to TAPSE and PASP alone in predicting all-cause mortality and rehospitalization for heart failure in elderly patients with HFpEF, with AUCs of 0.843(95%CI: 0.807-0.879, P<0.001), 0.810(95%CI: 0.770-0.849, P<0.001), and 0.716(95%CI: 0.669-0.764, P<0.001), respectively. Kaplan-Meier survival analysis curves showed that the cumulative survival rate of patients in the TAPSE/PASP≤0.35 mm/mmHg group was significantly lower than that in the TAPSE/PASP>0.35 mm/mmHg group(P<0.001).Conclusion TAPSE/PASP is an independent predictor of all-cause death and heart failure rehospitalization in elderly HFpEF patients. The survival rate was higher when TAPSE/PASP>0.35 mm/mmHg. -

-
表 1 研究人群的基线临床特征
Table 1. General data
例(%), X±S, M(P25, P75) 项目 无事件组(204例) 终点事件组(262例) P 年龄/岁 73±6 74±6 0.339 男性 111(45.5) 133(54.5) 0.434 缺血性心肌病 98(32.6) 203(67.4) <0.001 高血压病 97(42.2) 133(57.8) 0.491 2型糖尿病 56(42.7) 75(57.3) 0.780 利尿剂 173(43.8) 222(56.2) 0.983 β受体阻滞剂 170(44.4) 213(55.6) 0.569 螺内酯 143(44.0) 182(56.0) 0.883 NYHA心功能分级 0.049 Ⅱ 81(38.8) 128(61.2) Ⅲ~Ⅳ 123(47.9) 134(52.1) SBP/mmHg 129±19 131±21 0.371 DBP/mmHg 80±13 78±13 0.099 心率/(次/min) 81±17 82±15 0.750 BMI/(kg/m2) 24.0±3.9 24.2±3.8 0.555 血钠/(mmol/L) 140±4 137±5 <0.001 血钾/(mmol/L) 4.31±0.55 4.38±0.58 0.190 血氯/(mmol/L) 102±5 100±4 0.003 尿酸/(μmol/L) 424±56 431±63 0.207 eGFR/(mL/min/1.73 m2) 59±17 57±16 0.288 血红蛋白/(g/L) 124±21 123±19 0.446 NT-proBNP/(pg/mL) 4 557 (3 762,5 839) 4 844 (3 348,6 937) 0.315 MLWHFQ评分/分 30±3 31±4 0.199 ALBI评分/分 -2.44±0.35 -2.34±0.36 0.002 eGFR:估测的肾小球滤过率。 表 2 患者超声心动图指标比较
Table 2. Comparison of echocardiographic indexes in patients
X±S 参数 无事件组(204例) 终点事件组(262例) P值 LVEF/% 53±2 53±3 0.457 LVEDD/mm 60±8 62±9 0.071 LAVI/(mL/m2) 37±4 38±5 0.324 CI/(L/min/m2) 2.54±0.48 2.48±0.40 0.130 E/e' 16±2 17±3 0.001 TAPSE/mm 18±2 16±2 <0.001 右心室内径/mm 25±5 mm 26±4 0.073 PASP/ mmHg 43±7 49±7 <0.001 RV s'/(cm/s) 8.9±2.3 8.5±1.5 0.048 TAPSE/PASP/(mm/mmHg) 0.43±0.07 0.33±0.08 <0.001 RV s':右心室收缩期峰值速度。 表 3 复合终点事件的多因素Cox回归分析
Table 3. Multivariate Cox regression analysis
变量 HR(95%CI) P值 TAPSE/PASP≤0.35 mm/mmHg 2.32(1.49~3.59) <0.001 血钠<135 mmol/L 1.86(1.38~2.52) <0.001 缺血性心肌病 1.48(1.09~2.02) 0.011 血糖 1.05(1.01~1.09) 0.014 TAPSE 0.86(0.71~1.05) 0.148 PASP 1.02(0.96~1.09) 0.456 表 4 根据TAPSE/PAS分组的基线临床特征
Table 4. Baseline clinical features based on TAPSE/PAS
例(%), X±S, M(P25, P75) 项目 TAPSE/PASP >0.35 mm/ mmHg组(263例) TAPSE/PASP ≤0.35 mm/ mmHg (203例) P值 年龄/岁 74±6 73±6 0.592 男性 144(59.0) 100(41.0) 0.239 缺血性心肌病 156(46.5) 145(53.5) 0.007 高血压病 133(57.8) 97(42.2) 0.551 2型糖尿病 78(59.5) 53(40.5) 0.398 利尿剂 224(56.7) 171(43.3) 0.781 β受体阻滞剂 215(56.1) 168(43.9) 0.778 螺内酯 178(54.8) 147(45.2) 0.270 NYHA心功能分级 0.050 Ⅱ级 107(51.2) 102(48.8) Ⅲ~Ⅳ级 156(60.7) 101(39.3) SBP/mmHg 130±19 131±22 0.630 DBP/mmHg 79±14 78±13 0.951 心率/(次/min) 80±17 84±14 0.017 BMI/(kg/m2) 23.9±3.9 24.4±3.8 0.128 血钠/(mmol/L) 140±5 137±5 <0.001 血钾/(mmol/L) 4.33±0.56 4.38±0.57 0.382 血氯/(mmol/L) 101±5 100±4 0.358 尿酸/(μmol/L) 428±57 428±63 0.921 eGFR/(mL/min/1.73 m2) 57±17 59±16 0.142 血红蛋白/(g/L) 123±21 124±19 0.963 NT-proBNP/(pg/mL) 4 589 (3 707,5 960) 4 850 (3 265,6 986) 0.457 MLWHFQ评分/分 31±3 31±4 0.809 ALBI评分/分 -2.43±0.34 -2.33±0.36 0.002 超声心动图 LVEF/% 53±2 53±3 0.852 LVEDD/ mm 60±8 63±9 <0.001 LAVI/(mL/m2) 37±4 38±5 0.018 CI/(L/min/m2) 2.54±0.46 2.45±0.40 0.012 E/e' 17±2 18±3 <0.001 右心室内径/mm 26±5 25±5 0.281 RV s'/(cm/s) 8.8±2.1 8.5±1.5 0.058 -
[1] Cai A, Qiu W, Zhou Y, et al. Clinical characteristics and 1-year outcomes in hospitalized patients with heart failure with preserved ejection fraction: results from the China Cardiovascular Association Database-Heart Failure Center Registry[J]. Eur J Heart Fail, 2022, 24(11): 2048-2062. doi: 10.1002/ejhf.2654
[2] American College of Cardiology/Heart Failure Society of America. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure[J]. J Card Fail, 2022, 28(5): e1-e167. doi: 10.1016/j.cardfail.2022.02.010
[3] 中华医学会老年医学分会心血管疾病学组, 《老年慢性心力衰竭诊治中国专家共识》编写组. 老年人慢性心力衰竭诊治中国专家共识(2021)[J]. 中华老年医学杂志, 2021, 40(5): 550-561.
[4] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 急性心力衰竭中国急诊管理指南(2022)[J]. 中华急诊医学杂志, 2022, 31(8): 1016-1041.
[5] McManus DD, Shah SJ, Fabi MR, et al. Prognostic value of left ventricular end-systolic volume index as a predictor of heart failure hospitalization in stable coronary artery disease: data from the Heart and Soul Study[J]. J Am Soc Echocardiogr, 2009, 22(2): 190-197. doi: 10.1016/j.echo.2008.11.005
[6] Dini FL, Cortigiani L, Baldini U, et al. Prognostic value of left atrial enlargement in patients with idiopathic dilated cardiomyopathy and ischemic cardiomyopathy[J]. Am J Cardiol, 2002, 89(5): 518-523. doi: 10.1016/S0002-9149(01)02290-1
[7] 刘修颖, 孙阳. 超声心动图评估射血分数保留型心力衰竭患者右心结构及功能研究进展[J]. 中国医学影像技术, 2020, 36(4): 614-617.
[8] Masarone D, Errigo V, Melillo E, et al. Effects of Sacubitril/Valsartan on the Right Ventricular Arterial Coupling in Patients with Heart Failure with Reduced Ejection Fraction[J]. J Clin Med, 2020, 9(10): 110.
[9] Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension[J]. Eur Heart J, 2022, 43(38): 3618-3731. doi: 10.1093/eurheartj/ehac237
[10] Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Kardiol Pol, 2016, 74(10): 1037-1147. doi: 10.5603/KP.2016.0141
[11] Tello K, Wan J, Dalmer A, Vanderpool R, et al. Validation of the tricuspid annular plane systolic excursion/systolic pulmonary artery pressure ratio for the assessment of right ventricular-arterial coupling in severe pulmonary hypertension[J]. Circ Cardiovasc Imag, 2019, 12: e009047. doi: 10.1161/CIRCIMAGING.119.009047
[12] Guazzi M, Dixon D, Labate V, et al. RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: stratification of clinical phenotypes and outcomes[J]. JACC Cardiovasc Imaging, 2017, 10: 1211-1221. doi: 10.1016/j.jcmg.2016.12.024
[13] Gevaert AB, Kataria R, Zannad F, et al. Heart failure with preserved ejection fraction: recent concepts in diagnosis, mechanisms and management[J]. Heart, 2022, 108(17): 1342-1350. doi: 10.1136/heartjnl-2021-319605
[14] Abdellatif M, Kroemer G. Heart failure with preserved ejection fraction: An age-related condition[J]. J Mol Cell Cardiol, 2022, 167: 83-84. doi: 10.1016/j.yjmcc.2022.03.008
[15] 程显声. 心室相互依赖与右心心肌力学功能模式[J]. 中华心血管病杂志, 2020, 48(10): 814-822.
[16] Melenovsky V, Hwang SJ, Lin G, et al. Right heart dysfunction in heart failure with preserved ejection fraction[J]. Eur Heart J, 2014, 35(48): 3452-3462. doi: 10.1093/eurheartj/ehu193
[17] Guazzi M, Bandera F, Pelissero G, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis[J]. Am J Physiol Heart Circ Physiol, 2013, 305(9): H1373-1381. doi: 10.1152/ajpheart.00157.2013
[18] Iacoviello M, Monitillo F, Citarelli G, et al. Right ventriculo-arterial coupling assessed by two-dimensional strain: A new parameter of right ventricular function independently associated with prognosis in chronic heart failure patients[J]. Int J Cardiol, 2017, 241: 318-321. doi: 10.1016/j.ijcard.2017.04.051
[19] Ghio S, Temporelli PL, Klersy C, et al. Prognostic relevance of a non-invasive evaluation of right ventricular function and pulmonary artery pressure in patients with chronic heart failure[J]. Eur J Heart Fail, 2013, 15(4): 408-414. doi: 10.1093/eurjhf/hfs208
[20] Guazzi M, Dixon D, Labate V, et al. RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: stratification of clinical phenotypes and outcomes[J]. JACC Cardiovasc Imaging, 2017, 10(10 Pt B): 1211-1221.
[21] Pecini R, Møller DV, Torp-Pedersen C, et al. Heart failure etiology impacts survival of patients with heart failure[J]. Int J Cardiol, 2011, 149(2): 211-215. doi: 10.1016/j.ijcard.2010.01.011
[22] Zhang ZH, Meng FQ, Hou XF, et al. Clinical characteristics and long-term prognosis of ischemic and non-ischemic cardiomyopathy[J]. Indian Heart J, 2020, 72(2): 93-100. doi: 10.1016/j.ihj.2020.04.004
[23] Reddy YNV, Obokata M, Verbrugge FH, et al. Atrial dysfunction in patients with heart failure with preserved ejection fraction and atrial fibrillation[J]. J Am Coll Cardiol, 2020, 76(9): 1051-1064. doi: 10.1016/j.jacc.2020.07.009
[24] McHugh K, DeVore AD, Wu J, et al. Heart failure with preserved ejection fraction and diabetes: JACC State-of-the-Art Review[J]. J Am Coll Cardiol, 2019, 73(5): 602-611. doi: 10.1016/j.jacc.2018.11.033
[25] MacDonald MR, Petrie MC, Varyani F, et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity(CHARM)programme[J]. Eur Heart J, 2008, 29(11): 1377-1385. doi: 10.1093/eurheartj/ehn153
[26] Lund LH, Claggett B, Liu J, et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum[J]. Eur J Heart Fail, 2018, 20(8): 1230-1239. doi: 10.1002/ejhf.1149
[27] Aguilar D, Deswal A, Ramasubbu K, et al. Comparison of patients with heart failure and preserved left ventricular ejection fraction among those with versus without diabetes mellitus[J]. Am J Cardiol, 2010, 105(3): 373-377. doi: 10.1016/j.amjcard.2009.09.041
[28] Kristensen SL, Mogensen UM, Jhund PS, et al. Clinical and echocardiographic characteristics and cardiovascular outcomes according to diabetes status in patients with heart failure and preserved ejection fraction: a report from the I-PRESERVE trial(irbesartan in heart failure with preserved ejection fraction)[J]. Circulation, 2017, 135: 724-735. doi: 10.1161/CIRCULATIONAHA.116.024593
[29] Lawson CA, Jones PW, Teece L, et al. Association between type 2 diabetes and all-cause hospitalization and mortality in the uk general heart failure population: stratification by diabetic glycemic control and medication intensification[J]. JACC Heart Fail, 2018, 6(1): 18-26. doi: 10.1016/j.jchf.2017.08.020
[30] 黄燕, 邹长虹, 张荣成, 等. 住院心力衰竭患者入院时低钠血症的发生率及其对预后的影响[J]. 中华心血管病杂志, 2015, 43(10): 868-873.
[31] Heesun Lee, Sang Eun Lee, Chan Soon Park, et al. Hyponatraemia and its prognosis inacute heart failure is related to right ventricular dysfunction[J]. BMJ Heart, 2018, 104(20): 1670-1677.
[32] Rusinaru D, Buiciuc O, Leborgne L, et al. Relation of serum sodium level to long-term outcome after a first hospitalization for heart failure with preserved ejection fraction[J]. Am J Cardiol, 2009, 103(3): 405-410. doi: 10.1016/j.amjcard.2008.09.091
[33] 贺玉琴, 刘永铭, 薛丽丽, 等. 射血分数中间型心力衰竭患者的临床特征及心脏结构功能变化[J]. 临床心血管病杂志, 2021, 37(6): 541-546. doi: 10.13201/j.issn.1001-1439.2021.06.010
[34] 张班, 刘晓刚, 胡立群. 射血分数保留的心力衰竭研究新进展[J]. 临床心血管病杂志, 2022, 38(4): 271-275. doi: 10.13201/j.issn.1001-1439.2022.04.004
-




 下载:
下载: