Influencing factors of 1-year readmission for heart failure patients based on optimal length of stay
-
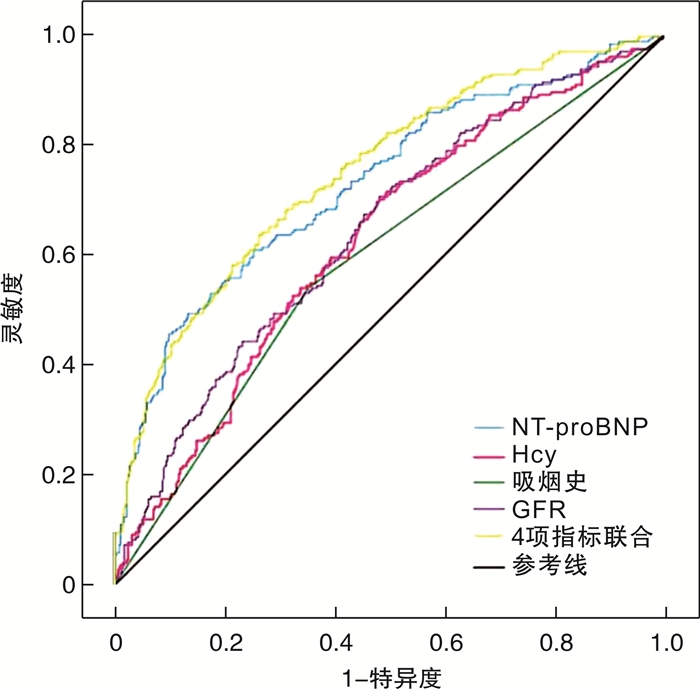
摘要: 目的 评估心力衰竭(心衰)患者住院时间(LOS)与1年内再入院风险的关系,探索最佳LOS患者再入院的影响因素。方法 收集2018-01-01—2020-12-31于川北医学院附属医院心血管内科住院治疗的心衰患者的临床资料,根据住院时间进行分组(LOS1:≤5 d、LOS2:6~10 d、LOS3:11~15 d、LOS4:≥16 d),通过单因素logistic回归分析展示不同LOS组与再入院的关系,筛选出OR比值最低的LOS组,根据1年内因心衰再入院的随访结果,把OR值最低的LOS患者分为再入院组、非再入院组,比较两组患者之间的基线资料,将差异有统计学意义的变量纳入多因素logistic回归分析,绘制受试者工作特征曲线(ROC)。结果 通过单因素回归分析可知,LOS2组患者OR值最低,共649例患者,其中再入院组为216例,非再入院组为433例;通过多因素logistic回归分析可知吸烟史、血同型半胱氨酸(Hcy)、N型末端脑钠肽前体(NT-proBNP)以及肾小球滤过率(eGFR)是LOS2组心衰患者1年内再入院的独立影响因素(P<0.05)。ROC曲线分析显示吸烟史、Hcy、eGFR、NT-proBNP单独以及联合预测LOS2患者1年内再入院的ROC曲线下面积(AUC)分别为0.594、0.627、0.643、0.733、0.775。结论 LOS2再入院风险最低。吸烟史、Hcy、NT-proBNP以及eGFR在LOS2组患者1年内再入院的风险中表现出良好的预测价值。Abstract: Objective To evaluate the relationship between the length of stay(LOS) and the risk of readmission within 1 year in patients with heart failure, and explore the optimal LOS patients and the influencing factors of readmission.Methods Clinical data of patients with heart failure admitted to the Department of Cardiology, Affiliated Hospital of North Sichuan Medical College, between January 1, 2018 and December 31, 2020 were collected. The patients were categorized into four groups based on their length of stay(LOS1: ≤5 days, LOS2: 6-10 days, LOS3: 11-15 days, LOS4: ≥16 days). Univariate logistic regression analysis was conducted to assess the relationship between the different LOS groups and readmission risk, and the hospitalization period with the lowest odds ratio(OR) was identified. Patients in the LOS group with the lowest OR were further divided into the readmission and non-readmission groups based on their follow-up readmission status within 1 year. Baseline data between the two groups were compared, and variables with statistically significant differences were included in multivariate logistic regression analysis and receiver operating characteristic curve(ROC).Results The LOS2 had the lowest OR value. A total of 649 patients was in LOS2 group, including 216 in the readmission group and 433 in the non-readmission group. Multivariate logistic regression analysis revealed that smoking history, blood homocysteine(Hcy), N-terminal pro-brain natriuretic peptide(NT-proBNP), and glomerular filtration rate(eGFR) were independent influencing factors for 1-year hospital readmission in patients with heart failure in the LOS2 group(P<0.05). ROC curve analysis shows that the area under the ROC curve(AUC) for predicting readmission within 1 year for LOS2 patients based on smoking history, Hcy, NT-proBNP, eGFR as individual predictors and in combination were 0.594, 0.627, 0.643, 0.733, and 0.775, respectively.Conclusion LOS2 had the lowest risk of readmission. The smoking history, Hcy, NT-proBNP, and eGFR are risk factors in the readmission within 1 year for patients in the LOS2 group.
-
Key words:
- heart failure /
- length of stay /
- readmission /
- influencing factors /
- risk prediction model
-

-
表 1 不同LOS患者的临床资料
Table 1. Clinical data of different LOS patients
X±S, M(P25, P75), 例(%) 变量 LOS1组(162例) LOS2组(649例) LOS3组(456例) LOS4组(220例) F/H/χ2值 P值 年龄/岁 70.16±12.48 68.93±12.43 71.80±11.16 70.64±11.71 5.289 0.001 男性 91(56.2) 379(58.4) 232(50.9) 121(55.0) 6.185 0.103 BMI/(kg/m2) 22.22±2.71 22.53±2.97 22.32±3.13 22.53±2.95 0.818 0.484 吸烟 63(38.9) 270(41.6) 158(34.6) 84(38.2) 5.487 0.139 饮酒 38(23.5) 204(31.4) 114(25.0) 52(23.6) 9.451 0.024 高血压 68(42.0) 312(48.1) 222(48.7) 123(56.0) 7.608 0.55 糖尿病 27(16.7) 134(20.6) 119(26.1) 76(34.5) 23.325 <0.001 冠心病 105(64.8) 439(67.6) 320(70.2) 160(72.7) 3.587 0.310 心房颤动 56(34.6) 233(36.0) 190(41.7) 77(35.0) 5.265 0.153 COPD 19(11.7) 95(14.6) 83(18.2) 44(20.0) 7.236 0.065 同型半胱氨酸/(μmol/L) 16.71(14.28,19.95) 17.35(14.23,21.15) 17.19(13.90,21.81) 16.40(13.58,20.34) 3.917 0.271 肌酐/(μmol/L) 86.20(68.20,108.00) 83.00(67.00,104.50) 83.30(67.00,105.60) 89.68(70.00,113.50) 8.150 0.043 GFR/(mL/min) 73.55(56.07,90.18) 73.99(55.43,91.12) 70.58(54.73,85.17) 68.09(48.16,83.67) 13.590 0.004 血钠/(mmol/L) 136.05±5.13 136.50±5.21 136.89±4.62 136.23±5.40 1.507 0.211 血钙/(mmol/L) 2.25±0.15 2.24±0.14 2.25±0.14 2.24±0.15 1.155 0.326 血钾/(mmol/L) 3.84±0.71 3.71±0.58 3.73±0.62 3.80±0.80 2.394 0.067 总胆红素/(μmol/L) 16.35(11.30,22.52) 17.40(12.36,24.30) 16.09(12.20,23.30) 16.57(11.53,25.47) 6.578 0.087 甘油三酯/(mmol/L) 1.17(0.87,1.53) 1.09(0.81,1.42) 1.10(0.83,1.45) 1.06(0.82,1.45) 3.797 0.284 NT-proBNP/(pg/mL) 2 249.08(860.00,5 373.00) 2 646.00(957.60,6 437.00) 2 729.00(968.20,6 583.50) 3 627.00(1 372.50,9 951.50) 11.439 0.010 纤维蛋白(原)降解产物/(μg/mL) 3.25(2.20,6.53) 3.10(2.00,5.40) 3.52(2.20,5.88) 3.50(2.30,6.45) 10.227 0.017 VLDL-C/(mmol/L) 0.69±0.36 0.71±0.36 0.71±0.33 0.70±0.37 0.134 0.940 HDL-C/(mmol/L) 1.11±0.39 1.11±0.35 1.12±0.37 1.10±0.41 0.265 0.851 LDL-C/(mmol/L) 2.16±0.76 2.15±0.79 2.13±0.75 2.16±0.80 0.134 0.940 血总胆固醇/(mmol/L) 3.96±1.08 3.96±1.12 3.96±1.07 3.96±1.12 0.002 1.000 血小板计数/(×109/L) 145.50(114.00,197.00) 151.00(112.00,194.00) 158.00(118.50,200.00) 154.00(112.00,213.50) 3.981 0.264 白细胞计数/(×109/L) 6.56(5.38,8.53) 6.54(5.35,8.16) 6.41(5.21,8.11) 7.10(5.73,9.41) 13.413 0.004 凝血酶原时间/s 14.20(13.50,15.40) 14.30(13.50,15.40) 14.30(13.50,15.50) 14.60(13.65,15.65) 5.606 0.132 血红蛋白/(g/L) 122.58±22.41 124.12±22.80 122.18±22.87 118.64±23.40 3.202 0.022 淋巴细胞计数/(×109/L) 1.17(0.83,1.58) 1.18(0.84,1.54) 1.17(0.79,1.54) 1.05(0.74,1.45) 5.839 0.120 左室舒张末期前后径/mm 53.41±8.85 54.41±10.13 53.82±9.63 54.22±10.20 0.613 0.606 左室射血分数/% 51.24±12.95 49.04±13.60 49.42±13.30 48.33±13.63 1.598 0.188 NYHA分级 5.108 0.164 Ⅰ 6(3.7) 43(6.6) 30(6.6) 12(5.5) Ⅱ 55(34.0) 212(32.7) 140(30.7) 60(27.3) Ⅲ 75(46.3) 312(48.1) 213(46.7) 108(49.1) Ⅳ 26(16.0) 82(12.6) 73(16.0) 40(18.2) 住院期间药物服用情况 降血脂药物 104(64.2) 438(67.5) 339(74.3) 157(71.4) 8.776 0.032 利尿剂 149(92.0) 601(92.6) 427(93.6) 209(95.0) 2.013 0.570 β受体阻滞剂 76(46.9) 428(65.9) 330(72.4) 140(63.6) 34.681 <0.001 ACEI/ARB 15(9.3) 119(18.3) 91(20.0) 37(16.8) 9.843 0.020 抗血小板聚集 104(64.2) 478(73.7) 344(75.4) 165(75.0) 8.300 0.040 抗凝药物 63(38.9) 279(43.0) 220(48.2) 108(49.1) 6.930 0.074 注:VLDL-C:极低密度脂蛋白胆固醇;HDL-C:高密度脂蛋白胆固醇;LDL-C:低密度脂蛋白胆固醇。 表 2 再入院的单因素logistic回归分析
Table 2. Univariate logistic regression of readmission
类别 β SE Wald χ2值 P值 OR值 95%CI LOS(以LOS2为参考) - - - - - - LOS1 0.447 0.179 6.249 0.012 1.564 (1.101~2.221) LOS3 0.458 0.126 13.217 <0.001 1.580 (1.235~2.022) LOS4 0.750 0.159 22.381 <0.001 2.117 (1.552~2.889) 常量 -0.695 0.083 69.701 <0.001 0.499 - 表 3 LOS2组再入院与非再入院患者的临床资料比较
Table 3. Clinical data between readmitted and non-readmitted patients in LOS2 group
X±S, M(P25, P75), 例(%) 变量 再入院组(216例) 非再入院组(433例) Z/χ2/t值 P值 年龄/岁 68.89±12.79 68.94±12.26 0.047 0.962 男性 140(64.8) 239(55.2) 5.488 0.019 BMI/(kg/m2) 22.77±3.07 22.57±2.92 0.409 0.683 吸烟 117(54.2) 153(35.3) 21.036 <0.001 饮酒 80(37.0) 124(28.6) 4.718 0.030 高血压 111(51.4) 201(46.4) 1.425 0.233 糖尿病 45(20.8) 89(20.6) 0.007 0.934 冠心病 145(67.1) 294(67.9) 0.039 0.844 心房颤动 79(36.6) 154(35.6) 0.064 0.801 COPD 29(13.4) 66(15.2) 0.381 0.537 Hcy/(μmol/L) 18.96(15.97,23.12) 16.73(13.56,20.28) -5.280 <0.001 肌酐/(μmol/L) 90.55(76.05,122.15) 78.00(63.80,97.20) -5.911 <0.001 GFR/(mL/min) 66.06(48.38,81.46) 77.71(61.12,96.25) -5.957 <0.001 血钠/(mmol/L) 135.91±5.53 136.79±5.03 2.047 0.041 血钙/(mmol/L) 2.24±0.15 2.24±0.13 -0.281 0.779 血钾/(mmol/L) 3.77±0.57 3.68±0.59 -1.905 0.057 总胆红素/(μmol/L) 17.95(13.15,27.63) 17.00(11.97,23.50) -2.102 0.036 甘油三酯/(mmol/L) 1.12(0.83,1.47) 1.06(0.80,1.40) -1.389 0.165 纤维蛋白(原)降解产物/(μg/mL) 3.60(2.30,5.93) 2.89(1.90,5.09) -2.972 0.003 VLDL-C/(mmol/L) 0.67±0.33 0.72±0.37 1.571 0.117 HDL-C/(mmol/L) 1.09±0.38 1.12±0.33 1.089 0.277 LDL-C/(mmol/L) 2.09±0.72 2.17±0.82 1.345 0.179 血总胆固醇/(mmol/L) 3.88±1.10 4.00±1.13 1.806 0.071 血小板计数/(×109/L) 151.00(110.50,191.50) 150.00(113.00,196.00) -0.632 0.527 白细胞计数/(×109/L) 6.80(5.24,8.39) 6.51(5.38,7.99) -0.977 0.328 凝血酶原时间/s 14.60(13.80,15.85) 14.10(13.0,15.20) -3.983 <0.001 血红蛋白/(g/L) 123.32±24.10 124.51±22.14 0.628 0.530 淋巴细胞计数/(×109/L) 1.16(0.83,1.52) 1.19(0.87,1.56) -0.549 0.583 左室舒张末期前后径/mm 57.74±9.93 52.75±9.82 -6.084 <0.001 左室射血分数/% 44.61±13.33 51.26±13.21 6.021 <0.001 NYHA分级 -3.909 <0.001 Ⅰ 8(3.7) 35(8.1) Ⅱ 57(26.4) 155(35.8) Ⅲ 113(52.3) 199(46.0) Ⅳ 38(17.6) 44(10.2) NT-proBNP -10.032 <0.001 ≤1 000 pg/mL 23(10.6) 148(34.2) 1 001~4 000 pg/mL 61(28.2) 171(39.5) 4 001~7 000 pg/mL 31(14.4) 65(15.0) 7 001~10 000 pg/mL 30(13.9) 23(5.3) >10 000 pg/mL 71(32.9) 26(6.0) 住院期间药物服用情况 降血脂药物 144(66.7) 294(67.9) 0.100 0.752 利尿剂 207(95.8) 394(91.0) 4.930 0.026 β受体阻滞剂 149(69.0) 279(64.4) 1.327 0.249 ACEI/ARB 49(22.7) 70(16.2) 4.090 0.043 抗血小板聚集 153(70.8) 325(75.1) 1.325 0.250 抗凝药物 96(44.4) 183(42.3) 0.280 0.597 表 4 LOS2组患者再入院的多因素logistic回归分析结果
Table 4. Multivariate logistic regression of readmission in LOS2 group
变量 β SE Waldχ2值 P值 OR值 95%CI 吸烟史 0.701 0.194 13.010 <0.001 2.015 (1.377~2.948) Hcy 0.022 0.011 4.054 0.044 1.023 (1.001~1.045) GFR -0.010 0.004 7.955 0.005 0.990 (0.983~0.997) NT-proBNP(以≤1 000 pg/mL为参照) - - - - - - 1 001~4 000 pg/mL 0.768 0.276 7.756 0.005 2.156 (1.256~3.703) 4 001~7 000 pg/mL 1.026 0.325 9.943 0.002 2.791 (1.475~5.282) 7 001~10 000 pg/mL 1.927 0.368 27.387 <0.001 6.868 (3.337~14.132) >10 000 pg/mL 2.735 0.331 68.369 <0.001 15.409 (8.058~29.467) 常量 -1.793 0.449 15.914 <0.001 0.166 - -
[1] 王华, 刘宇佳, 杨杰孚. 心力衰竭流行病学[J]. 临床心血管病杂志, 2023, 39(4): 243-247. doi: 10.13201/j.issn.1001-1439.2023.04.001
[2] Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association[J]. Circulation, 2013, 127(1): 143-152. doi: 10.1161/CIR.0b013e318282ab8f
[3] Savarese G, Becher PM, Lund LH et al. Global burden of heart failure: a comprehensive and updated review of epidemiology[J]. Cardiovasc Res, 2023, 118(17): 3272-3287. doi: 10.1093/cvr/cvac013
[4] Gorodeski EZ, Goyal P, Hummel SL, et al. Domain Management Approach to Heart Failure in the Geriatric Patient: Present and Future[J]. J Am Coll Cardiol, 2018, 71(17): 1921-1936. doi: 10.1016/j.jacc.2018.02.059
[5] Arundel C, Lam PH, Faselis C, et al. Length of stay and readmission in older adults hospitalized for heart failure[J]. Arch Med Sci, 2021, 17(4): 891-899. doi: 10.5114/aoms.2019.89702
[6] Olchanski N, Vest AR, Cohen JT, et al. Two-year outcomes and cost for heart failure patients following discharge from the hospital after an acute heart failure admission[J]. Int J Cardiol, 2020.307: 109-113. doi: 10.1016/j.ijcard.2019.10.033
[7] Kaboli PJ, Go JT, Hockenberry J, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals[J]. Ann Intern Med, 2012, 157(12): 837-845. doi: 10.7326/0003-4819-157-12-201212180-00003
[8] Reynolds K, Butler MG, Kimes TM, et al. Relation of acute heart failure hospital length of stay to subsequent readmission and all-cause mortality[J]. Am J Cardiol, 2015, 116(3): 400-405. doi: 10.1016/j.amjcard.2015.04.052
[9] Tigabe Tekle M, Bekalu AF, Tefera YG. Length of hospital stay and associated factors among heart failure patients admitted to the University Hospital in Northwest Ethiopia[J]. PLoS One, 2022, 17(7): e0270809. doi: 10.1371/journal.pone.0270809
[10] Khan H, Greene SJ, Fonarow GC, et al. Length of hospital stay and 30-day readmission following heart failure hospitalization: insights from the EVEREST trial[J]. Eur J Heart Fail, 2015, 17(10): 1022-1031. doi: 10.1002/ejhf.282
[11] Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[J]. Circulation, 2022, 145(18): e876-e894.
[12] 中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789.
[13] Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia[J]. JAMA, 2013, 309(4): 355-363. doi: 10.1001/jama.2012.216476
[14] Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis[J]. Ann Intern Med, 2014, 160(11): 774-784. doi: 10.7326/M14-0083
[15] Mai D, Brand C, Haschtmann D, et al. Non-medical factors significantly influence the length of hospital stay after surgery for degenerative spine disorders[J]. Eur Spine J, 2020, 29(2): 203-212. doi: 10.1007/s00586-019-06209-5
[16] Aung YN, Nur AM, Ismail A, et al. Determining the cost and length of stay at intensive care units and the factors influencing them in a teaching hospital in Malaysia[J]. Value Health Reg Issues, 2020, 21: 149-156. doi: 10.1016/j.vhri.2019.09.006
[17] Yoshimura Y, Wakabayashi H, Shiraishi A, et al. Hemoglobin Improvement is Positively Associated with Functional Outcomes in Stroke Patients with Anemia[J]. J Stroke Cerebrovasc Dis, 2021, 30(1): 105453. doi: 10.1016/j.jstrokecerebrovasdis.2020.105453
[18] Han GL, Yu Y, Han CS, et al. Logistic regression analysis of factors influencing hospitalization time for community acquired pneumonia[J]. Prac Med, 2021, 16: 28-32.
[19] Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review[J]. Patient Educ Couns, 2018, 101(3): 363-374. doi: 10.1016/j.pec.2017.10.002
[20] Fonarow GC, Ziaeian B. Hospital Readmission Reduction Program for Heart Failure: The Spread of Intended and Unintended Consequences[J]. J Am Coll Cardiol, 2019, 73(9): 1013-1015.
[21] Yoo JE, Jeong SM, Yeo Y, et al. Smoking Cessation Reduces the Risk of Heart Failure: A Nationwide Cohort Study[J]. JACC Heart Fail, 2023, 11(3): 277-287. doi: 10.1016/j.jchf.2022.07.006
[22] Kaplan P, Tatarkova Z, Sivonova MK, et al. Homocysteine and Mitochondria in Cardiovascular and Cerebrovascular Systems[J]. Int J Mol Sci, 2020, 21(20): 110.
[23] Strauss E, Supinski W, Radziemski A, et al. Is hyperhomocysteinemia a causal factor for heart failure? The impact of the functional variants of MTHFR and PON1 on ischemic and non-ischemic etiology[J]. Int J Cardiol, 2017, 228: 37-44. doi: 10.1016/j.ijcard.2016.11.213
[24] Vasan RS, Beiser A, D'Agostino RB, et al. Plasma homocysteine and risk for congestive heart failure in adults without prior myocardial infarction[J]. JAMA, 2003, 289(10): 1251-1257. doi: 10.1001/jama.289.10.1251
[25] Wang X, Yang Y, Xu L, et al. Association between homocysteine level and length of stay in patients with lower extremity atherosclerotic disease: a retrospective cohort study[J]. BMJ Open, 2023, 13(7): e067677. doi: 10.1136/bmjopen-2022-067677
[26] Karger AB, Steffen BT, Nomura SO, et al. Association Between Homocysteine and Vascular Calcification Incidence, Prevalence, and Progression in the MESA Cohort[J]. J Am Heart Assoc, 2020, 9(3): e013934. doi: 10.1161/JAHA.119.013934
[27] Vodovar N, Mebazaa A, Januzzi JL Jr, et al. Evolution of natriuretic peptide biomarkers in heart failure: Implications for clinical care and clinical trials[J]. Int J Cardiol, 2018, 254: 215-221. doi: 10.1016/j.ijcard.2017.11.001
[28] Kubler P, Petruk-Kowalczyk J, Majda J, et al. Persistent high NTpro-BNP concentration as a negative prognostic factor in patients with decompensated heart failure[J]. Kardiol Pol, 2006, 64(3): 250-256;discussion 257-258.
[29] Bayés-GenísA, Lopez L, Zapico E, et al. NT-ProBNP reduction percentage during admission for acutely decompensated heart failure predicts long-term cardiovascular mortality[J]. J Card Fail, 2005, 11(5 Suppl): S3-8.
[30] KhanA, Johnson DK, Carlson S, et al. NT-ProBNP Predicts Myocardial Injury Post-vascular Surgery and is Reduced with CoQ(10): A Randomized Double-Blind Trial[J]. Ann Vasc Surg, 2020, 64: 292-302. doi: 10.1016/j.avsg.2019.09.017
[31] Krim SR, Vivo RP, Krim NR, et al. Racial/Ethnic differences in B-type natriuretic peptide levels and their association with care and outcomes among patients hospitalized with heart failure: findings from Get With The Guidelines-Heart Failure[J]. JACC Heart Fail, 2013, 1(4): 345-352. doi: 10.1016/j.jchf.2013.04.008
[32] Pocock SJ, Ferreira JP, Packer M, et al. Biomarker-driven prognostic models in chronic heart failure with preserved ejection fraction: the EMPEROR-Preserved trial[J]. Eur J Heart Fail, 2022, 24(10): 1869-1878. doi: 10.1002/ejhf.2607
[33] Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study[J]. Eur Heart J, 2006, 27(3): 330-337. doi: 10.1093/eurheartj/ehi631
[34] Bettencourt P, Azevedo A, Pimenta J, et al. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients[J]. Circulation, 2004, 110(15): 2168-2174. doi: 10.1161/01.CIR.0000144310.04433.BE
[35] Beldhuis IE, Streng KW, van der Meer P, et al. Trajectories of changes in renal function in patients with acute heart failure[J]. J Card Fail, 2019, 25(11): 866-874. doi: 10.1016/j.cardfail.2019.07.004
[36] de la Espriella R, Navarro J, Mollar A, et al. Long-term prognostic impact of estimated glomerular filtration rate on admission in patients hospitalized for acute heart failure[J]. Cardiorenal Med, 2022, 12(4): 179-188. doi: 10.1159/000526105
[37] Greene SJ, Gheorghiade M, Vaduganathan M, et al. Haemoconcentration, renal function, and post-discharge outcomes among patients hospitalized for heart failure with reduced ejection fraction: insights from the EVEREST trial[J]. Eur J Heart Fail, 2013, 15(12): 1401-1411. doi: 10.1093/eurjhf/hft110
[38] Szlagor M, Dybiec J, Młynarska E, et al. Chronic Kidney Disease as a Comorbidity in Heart Failure[J]. Int J Mol Sci, 2023, 24(3): 110.
[39] McCallum W, Tighiouart H, Kiernan MS, et al. Relation of Kidney Function Decline and NT-proBNP With Risk of Mortality and Readmission in Acute Decompensated Heart Failure[J]. Am J Med, 2020, 133(1): 115-122.e2. doi: 10.1016/j.amjmed.2019.05.047
-




 下载:
下载: