Chinese guideline for lipid management(primary care version 2024)
-
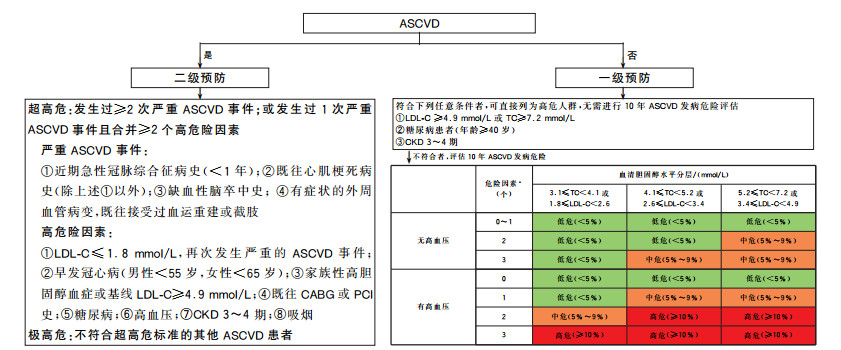
摘要: 低密度脂蛋白胆固醇(LDL-C)是动脉粥样硬化性心血管疾病(ASCVD)的致病性危险因素。近几十年来,中国人群的血脂异常患病率不断升高,血脂管理刻不容缓,在基层开展血脂规范管理尤为重要。《中国血脂管理指南(基层版2024年)》简明地推荐LDL-C作为血脂干预的首要靶点,以ASCVD危险分层确定其目标值;推荐在生活方式干预的基础上,以中等强度他汀类药物作为起始药物治疗,必要时联用胆固醇吸收抑制剂和(或)前蛋白转化酶枯草溶菌素9抑制剂的达标策略;并就常见特殊人群的血脂管理策略进行了推荐。本指南旨在为基层医生开展血脂管理提供指导,全面提升基层医生的血脂管理水平,推进ASCVD的一级和二级预防工作。Abstract: Low-density lipoprotein cholesterol (LDL-C) is a pathogenic risk factor for atherosclerotic cardiovascular disease (ASCVD). In recent decades, the prevalence of dyslipidemia in the Chinese population increases continuously, it is urgent to improve blood lipid management in China. It is particularly important to carry out standardized blood lipid management at primary healthcare institutions. The Chinese guideline for lipid management (primary care version 2024) concisely recommends that LDL-C should be the preferred intervention target in lipid management, and the target values of LDL-C should be determined based on ASCVD risk stratification. The present guideline recommends to use moderate-intensity statins at the beginning of treatment on the basis of lifestyle intervention. If the LDL-C target level can not be reached, other lipid-lowering drugs like cholesterol absorption inhibitors and (or) proprotein convertase subtilisin/kexin type 9 inhibitors should be jointly used for the purpose of reaching the target value. The present guideline also provides blood lipid management strategies for special populations. We aim to provide guidance for primary healthcare professionals to carry out blood lipid management, and comprehensively improve their ability on blood lipid management, and thereby improve the primary and secondary prevention of ASCVD in China.
-

-
表 1 中国ASCVD一级预防低危人群非糖尿病患者主要血脂指标的参考标准
Table 1. Reference values of blood lipids for the primary prevention of ASCVD in low-risk populations without diabetes
mmol/L 分类 TC LDL-C HDL-C TG 非HDL-C 理想水平 - <2.6 - - <3.4 合适水平 <5.2 <3.4 - <1.7 <4.1 边缘升高 ≥5.2且<6.2 ≥3.4且<4.1 - ≥1.7且<2.3 ≥4.1且<4.9 升高 ≥6.2 ≥4.1 - ≥2.3 ≥4.9 降低 - - <1.0 - - 注:表中所列数值是干预前空腹12 h测定的血脂水平。-:无。 表 2 降脂靶点的目标值
Table 2. The goal attainment values of LDL-C
表 3 血脂管理膳食治疗建议
Table 3. Recommendation of dietary therapy for lipid management
表 4 降TG的药物治疗建议
Table 4. Recommendation of drugs for TG-lowering treatment
表 5 他汀类药物降胆固醇强度
Table 5. The cholesterol reduction intensity of stains
降胆固醇强度 药物及其剂量 高强度(每日剂量可降低 阿托伐他汀40~80 mg LDL-C ≥50%) 瑞舒伐他汀20 mg 中等强度(每日剂量可降 阿托伐他汀10~20 mg 低LDL-C 25%~<50%) 瑞舒伐他汀5~10 mg 氟伐他汀80 mg 洛伐他汀40 mg 匹伐他汀1~4 mg 普伐他汀40 mg 辛伐他汀20~40 mg 血脂康1.2 g 表 6 主要降TG的药物
Table 6. Main TG-lowering drugs
药物分类 剂量 不良反应 贝特类药物 非诺贝特片 0.1 g,3次/d 包括肝脏、肌肉和肾毒性等 微粒化非诺贝特 0.2 g,1次/d 非诺贝特缓释胶囊 0.25 g,1次/d 苯扎贝特 0.2 g,3次/d 苯扎贝特缓释片 0.4 g,1次/d 吉非贝齐 0.6 g,2次/d ω-3脂肪酸 IPE 1~4 g/d 胃肠道反应,大剂量应用可能增加轻微出血、新发心房颤动风险 EPA+DHA 1~4 g/d 烟酸及其同类物 烟酸缓释片 0.375~1.000 g,1次/d 颜面潮红、皮肤瘙痒、皮疹、肝脏损害、高尿酸血症、高血糖、棘皮症和消化道不适等 阿昔莫司 0.25~0.50 g,2次/d 注:IPE:二十碳五烯酸乙酯;EPA:二十碳五烯酸;DHA:二十二碳六烯酸。 表 7 降脂药物的联合应用策略
Table 7. Combination of lipid-lowering drugs
联合应用策略a) 适用情况 安全性关注点 他汀类药物+胆固醇吸收抑制剂 单药治疗后LDL-C不达标 常规监测 他汀类药物+PCSK9抑制剂 单药治疗后LDL-C不达标 常规监测 他汀类药物+胆固醇吸收抑制剂+PCSK9抑制剂 双联用药后LDL-C不达标 常规监测 他汀类药物+ω-3脂肪酸(IPE、EPA+DHA)或非诺贝特 LDL-C达标、TG 2.3~5.7 mmol/L 心房颤动、出血、肾功能 贝特类药物+ω-3脂肪酸(IPE、EPA+DHA) 单药治疗后TG≥5.7 mmol/L 常规监测 注:a)联合应用策略中的他汀类药物均指中等强度他汀类药物(具体药物和剂量见表 5)。 表 8 糖尿病患者血脂目标值建议
Table 8. Recommendation of target values of blood lipids in patients with diabetes
推荐建议 糖尿病合并ASCVD患者:LDL-C<1.4 mmol/L[10, 21, 26],且降低幅度>50% ASCVD风险为高危的糖尿病患者a):LDL-C<1.8 mmol/L[27],且降低幅度>50% ASCVD风险为低、中危的糖尿病患者:LDL-C<2.6 mmol/L[17] 糖尿病患者以非HDL-C为次要目标,目标值为相应的LDL-C目标值+0.8 mmol/L 注:a)指年龄≥40岁的糖尿病患者,或者20~39岁糖尿病患者有≥3个危险因素(高血压、血脂异常、吸烟、肥胖、早发冠心病家族史)或合并靶器官损害(蛋白尿、肾功能损害、左心室肥厚或视网膜病变)或1型糖尿病病程≥20年。 表 9 脑卒中患者的降脂治疗建议
Table 9. Recommendation of lipid-lowering treatment for stroke patients
-
[1] 国家心血管病中心. 中国心血管健康与疾病报告2021[M]. 北京: 科学出版社. 2022.
[2] Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel[J]. Eur Heart J, 2017, 38(32): 2459-2472. DOI: 10.1093/eurheartj/ehx144.
[3] 国家卫生健康委员会疾病预防控制局. 中国居民营养与慢性病状况报告2015[M]. 北京: 人民卫生出版社. 2015.
[4] 中国血脂管理指南修订联合专家委员会. 中国血脂管理指南(2023年)[J]. 中国循环杂志. 2023, 38(3): 237-271. DOI: 10.3969/j.issn.1000-3614.2023.03.001.
[5] Cholesterol Treatment Trialists Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials[J]. Lancet, 2012, 380(9841): 581-590. DOI: 10.1016/S0140-6736(12)60367-5.
[6] Cholesterol Treatment Trialists Collaboration. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174, 000 participants in 27 randomised trials[J]. Lancet, 2015, 385(9976): 1397-1405. DOI: 10.1016/S0140-6736(14)61368-4.
[7] Yusuf S, Bosch J, Dagenais G, et al. Cholesterol Lowering in Intermediate-Risk Persons without Cardiovascular Disease[J]. N Engl J Med, 2016, 374(21): 2021-2031. DOI: 10.1056/NEJMoa1600176.
[8] Ridker PM, Mora S, Rose L, et al. Percent reduction in LDL cholesterol following high-intensity statin therapy: potential implications for guidelines and for the prescription of emerging lipid-lowering agents[J]. Eur Heart J, 2016, 37(17): 1373-1379. DOI: 10.1093/eurheartj/ehw046.
[9] Bangalore S, Fayyad R, Kastelein JJ, et al. 2013 Cholesterol Guidelines Revisited: Percent LDL Cholesterol Reduction or Attained LDL Cholesterol Level or Both for Prognosis?[J]. Am J Med, 2016, 129(4): 384-391. DOI: 10.1016/j.amjmed.2015.10.024.
[10] Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome[J]. N Engl J Med, 2018, 379(22): 2097-2107. DOI: 10.1056/NEJMoa1801174.
[11] Zhong VW, Van Horn L, Cornelis MC, et al. Associations of Dietary Cholesterol or Egg Consumption With Incident Cardiovascular Disease and Mortality[J]. JAMA, 2019, 321(11): 1081-1095. DOI: 10.1001/jama.2019.1572.
[12] Ginsberg HN, Karmally W, Siddiqui M, et al. A dose-response study of the effects of dietary cholesterol on fasting and postprandial lipid and lipoprotein metabolism in healthy young men[J]. Arterioscler Thromb, 1994, 14(4): 576-586. DOI: 10.1161/01.atv.14.4.576.
[13] Ginsberg HN, Karmally W, Siddiqui M, et al. Increases in dietary cholesterol are associated with modest increases in both LDL and HDL cholesterol in healthy young women[J]. Arterioscler Thromb Vasc Biol, 1995, 15(2): 169-178. DOI: 10.1161/01.atv.15.2.169.
[14] Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials[J]. PLoS Med, 2010, 7(3): e1000252. DOI: 10.1371/journal.pmed.1000252.
[15] Kim BK, Hong SJ, Lee YJ, et al. Long-term efficacy and safety of moderate-intensity statin with ezetimibe combination therapy versus high-intensity statin monotherapy in patients with atherosclerotic cardiovascular disease(RACING): a randomised, open-label, non-inferiority trial[J]. Lancet, 2022, 400(10349): 380-390. DOI: 10.1016/S0140-6736(22)00916-3.
[16] Christian JB, Arondekar B, Buysman EK, et al. Clinical and economic benefits observed when follow-up triglyceride levels are less than 500 mg/dL in patients with severe hypertriglyceridemia[J]. J Clin Lipidol, 2012, 6(5): 450-461. DOI: 10.1016/j.jacl.2012.08.007.
[17] Bhatt DL, Steg PG, Miller M, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia[J]. N Engl J Med, 2019, 380(1): 11-22. DOI: 10.1056/NEJMoa1812792.
[18] Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients(JELIS): a randomised open-label, blinded endpoint analysis[J]. Lancet, 2007, 369(9567): 1090-1098. DOI: 10.1016/S0140-6736(07)60527-3.
[19] Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus(the FIELD study): randomised controlled trial[J]. Lancet, 2005, 366(9500): 1849-1861. DOI: 10.1016/S0140-6736(05)67667-2.
[20] Accord Study Group. Effects of combination lipid therapy in type 2 diabetes mellitus[J]. N Engl J Med, 2010, 362(17): 1563-1574. DOI: 10.1056/NEJMoa1001282.
[21] Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes[J]. N Engl J Med, 2015, 372(25): 2387-2397. DOI: 10.1056/NEJMoa1410489.
[22] Liao J, Wang X, Li Z, et al. Pharmacokinetic study of oral (14)C-Radiolabeled Hyzetimibe, a new cholesterol absorption inhibitor[J]. Front Pharmacol, 2021, 12: 665372. DOI: 10.3389/fphar.2021.665372.
[23] O'Donoghue ML, Giugliano RP, Wiviott SD, et al. Long-Term Evolocumab in Patients With Established Atherosclerotic Cardiovascular Disease[J]. Circulation, 2022, 146(15): 1109-1119. DOI: 10.1161/CIRCULATIONAHA.122.061620.
[24] Qi L, Liu D, Qu Y, et al. Tafolecimab in Chinese Patients With Hypercholesterolemia (CREDIT-4): A randomized, double-blind, placebo-controlled phase 3 trial[J]. JACC Asia, 2023, 3(4): 636-645. DOI: 10.1016/j.jacasi.2023.04.011.
[25] Fitzgerald K, White S, Borodovsky A, et al. A highly durable RNAi therapeutic inhibitor of PCSK9[J]. N Engl J Med, 2017, 376(1): 41-51. DOI: 10.1056/NEJMoa1609243.
[26] Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease[J]. N Engl J Med, 2017, 376(18): 1713-1722. DOI: 10.1056/NEJMoa1615664.
[27] Cholesterol Treatment Trialists Collaborators. Efficacy of cholesterol-lowering therapy in 18, 686 people with diabetes in 14 randomised trials of statins: a meta-analysis[J]. Lancet, 2008, 371(9607): 117-125. DOI: 10.1016/S0140-6736(08)60104-X.
[28] Cholesterol Treatment Trialists Collaboration. Impact of renal function on the effects of LDL cholesterol lowering with statin-based regimens: a meta-analysis of individual participant data from 28 randomised trials[J]. Lancet Diabetes Endocrinol, 2016, 4(10): 829-839. DOI: 10.1016/S2213-8587(16)30156-5.
[29] Wanner C, Krane V, Marz W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis[J]. N Engl J Med, 2005, 353(3): 238-248. DOI: 10.1056/NEJMoa043545.
[30] Fellstrom BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis[J]. N Engl J Med, 2009, 360(14): 1395-1407. DOI: 10.1056/NEJMoa0810177.
[31] Mychaleckyj JC, Craven T, Nayak U, et al. Reversibility of fenofibrate therapy-induced renal function impairment in ACCORD type 2 diabetic participants[J]. Diabetes Care, 2012, 35(5): 1008-1014. DOI: 10.2337/dc11-1811.
[32] Linz PE, Lovato LC, Byington RP, et al. Paradoxical reduction in HDL-C with fenofibrate and thiazolidinedione therapy in type 2 diabetes: the ACCORD Lipid Trial[J]. Diabetes Care, 2014, 37(3): 686-693. DOI: 10.2337/dc13-0790.
[33] Amarenco P, Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention[J]. Lancet Neurol, 2009, 8(5): 453-463. DOI: 10.1016/S1474-4422(09)70058-4.
[34] Amarenco P, Bogousslavsky J, Callahan A, 3rd, et al. High-dose atorvastatin after stroke or transient ischemic attack[J]. N Engl J Med, 2006, 355(6): 549-559. DOI:10.1056/NEJMoa061894.
-




 下载:
下载: