Chinese expert consensus for the diagnosis and management of diuretic resistance in patients with heart failure
-
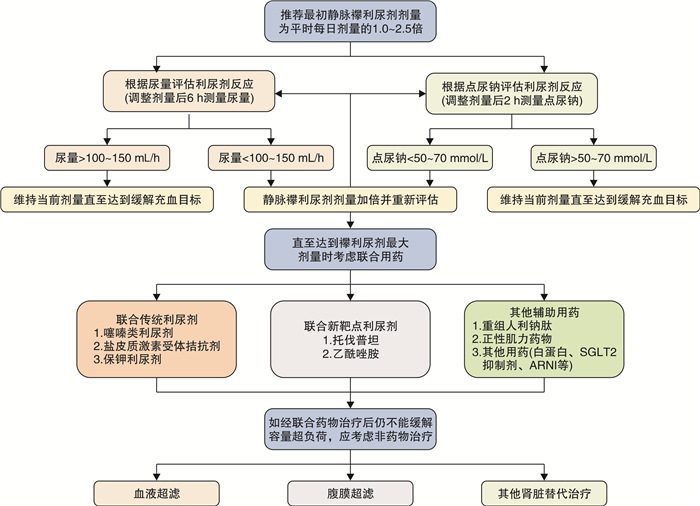
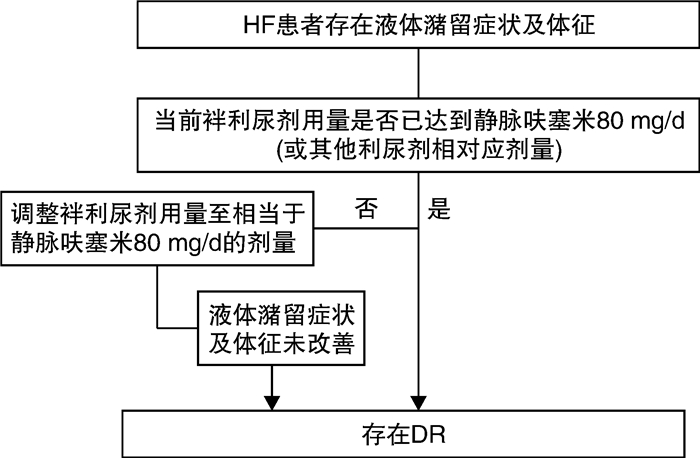
摘要: 利尿剂是住院心力衰竭(heart failure,HF)特别是急性失代偿心力衰竭(acute decompensated heart failure,ADHF)患者容量管理的基石。利尿剂抵抗(diuretic resistance,DR)表现为对利尿剂的反应减低甚至完全失效,不仅导致住院时间延长,还使病死率和再住院率增加。目前国内外尚缺乏对HF患者DR诊断和管理的共识。本共识梳理DR的定义、机制、诊断和管理等方面内容,并基于临床研究结果和专家经验,提出相应的处理建议,旨在提高临床医师对DR的认识,并规范DR治疗。Abstract: Diuretics play a crucial role in volume management for hospitalized patients with heart failure (HF), particularly those with acute decompensated HF (ADHF). Diuretic resistance (DR), manifested as a diminished response or even a failure to diuretics, which not only prolongs in-hospital stay but also increases mortality and rehospitalization. There is not yet a consensus regarding the diagnosis and management of DR in heart failure patients. Therefore, this consensus focuses on elucidating the definition, mechanisms, diagnosis, and management of DR. Based on clinical research findings and expert experiences, it offers recommendations for treatment, aiming to enhance physicians' awareness and standardize the management.
-
Key words:
- heart failure /
- diuretic resistance /
- volume management
-

-
药物 起始剂量 每日最大剂量 常用剂量 襻利尿剂 呋塞米 20~40 mg,1次/d
20~40 mg,1~2次/d(AHA指南)120~160 mg
600 mg(AHA指南)20~80 mg
40~240 mg(ESC指南)托拉塞米 10 mg,1次/d
5~10 mg,1次/d(ESC指南)
10~20 mg,1次/d(AHA指南)100 mg
200 mg(AHA指南)10~40 mg
10~20 mg(ESC指南)布美他尼 0.5~1 mg,1次/d
0.5~1 mg,1~2次/d(AHA指南)6~8 mg
10 mg(AHA指南)1~4 mg
1~5 mg(ESC指南)噻嗪类利尿剂 氢氯噻嗪 12.5~25 mg,1~2次/d
25 mg,1次/d(ESC指南)
25 mg,1~2次/d(AHA指南)100 mg
200 mg(AHA指南)25~50 mg
12.5~100 mg(ESC指南)吲达帕胺 2.5 mg,1次/d 5 mg 2.5~5 mg 美托拉宗 2.5 mg,1次/d 20 mg 2.5~10 mg 醛固酮受体拮抗剂 螺内酯 10~20 mg,1次/d
25 mg,1次/d(ESC指南)20~40 mg
50 mg(ESC指南)依普利酮 25 mg,1次/d 50 mg 保钾利尿剂 阿米洛利 2.5 mga/5 mgb,1次/d 20 mg 5~10 mga/10~20 mgb 氨苯蝶啶 25 mga/50 mgb,1次/d 200 mg 100 mga/200 mgb 血管升压素V2受体拮抗剂 托伐普坦 7.5~15 mg,1次/d 30 mg 15 mg 碳酸酐酶抑制剂 乙酰唑胺 500 mg,1次/d,3 d 注:a与血管紧张素转换酶抑制剂(ACEI)或血管紧张素Ⅱ受体阻滞剂(ARB)合用时的剂量;b不与ACEI或ARB合用时的剂量。 -
[1] 崔炜. 心力衰竭患者利尿剂抵抗的处理策略[J]. 中国心血管杂志, 2015, 20(1): 1-3. doi: 10.3969/j.issn.1007-5410.2015.01.001
[2] Ellison DH. Diuretic therapy and resistance in congestive heart failure[J]. Cardiology, 2001, 96(3-4): 132-143. doi: 10.1159/000047397
[3] Trullàs JC, Casado J, Morales-Rull JL, et al. Prevalence and outcome of diuretic resistance in heart failure[J]. Intern Emerg Med, 2019, 14(4): 529-537. doi: 10.1007/s11739-018-02019-7
[4] Neuberg GW, Miller AB, O'Connor CM, et al. Diuretic resistance predicts mortality in patients with advanced heart failure[J]. Am Heart J, 2002, 144(1): 31-38. doi: 10.1067/mhj.2002.123144
[5] 中国老年医学学会心电及心功能分会, 中国医师协会心血管内科分会, 中国心衰中心联盟专家委员会. 慢性心力衰竭加重患者的综合管理中国专家共识2022[J]. 中国循环杂志, 2022, 37(3): 215-225. doi: 10.3969/j.issn.1000-3614.2022.03.003
[6] Reed BN, Devabhakthuni S. Diuretic resistance in acute decompensated heart failure: a challenging clinical conundrum[J]. Crit Care Nurs Q, 2017, 40(4): 363-373. doi: 10.1097/CNQ.0000000000000173
[7] Doering A, Jenkins CA, Storrow AB, et al. Markers of diuretic resistance in emergency department patients with acute heart failure[J]. Int J Emerg Med, 2017, 10(1): 17. doi: 10.1186/s12245-017-0143-x
[8] Ellison DH, Felker GM. Diuretic Treatment in heart failure[J]. N Engl J Med, 2017, 377(20): 1964-1975. doi: 10.1056/NEJMra1703100
[9] Honda S, Nagai T, Nishimura K, et al. Long-term prognostic significance of urinary sodium concentration in patients with acute heart failure[J]. Int J Cardiol, 2018, 254: 189-194. doi: 10.1016/j.ijcard.2017.08.053
[10] Testani JM, Cappola TP, Brensinger CM, et al. Interaction between loop diuretic-associated mortality and blood urea nitrogen concentration in chronic heart failure[J]. J Am Coll Cardiol, 2011, 58(4): 375-382. doi: 10.1016/j.jacc.2011.01.052
[11] Mullens W, Damman K, Harjola VP, et al. The use of diuretics in heart failure with congestion-a position statement from the Heart Failure Association of the European Society of Cardiology[J]. Eur J Heart Fail, 2019, 21(2): 137-155. doi: 10.1002/ejhf.1369
[12] Kitsios GD, Mascari P, Ettunsi R, et al. Co-administration of furosemide with albumin for overcoming diuretic resistance in patients with hypoalbuminemia: a meta-analysis[J]. J Crit Care, 2014, 29(2): 253-259. doi: 10.1016/j.jcrc.2013.10.004
[13] Rahman R, Paz P, Elmassry M, et al. Diuretic resistance in heart failure[J]. Cardiol Rev, 2021, 29(2): 73-81. doi: 10.1097/CRD.0000000000000310
[14] Agrawal A, Naranjo M, Kanjanahattakij N, et al. Cardiorenal syndrome in heart failure with preserved ejection fraction-an under-recognized clinical entity[J]. Heart Fail Rev, 2019, 24(4): 421-437. doi: 10.1007/s10741-018-09768-9
[15] Guazzi M, Gatto P, Giusti G, et al. Pathophysiology of cardiorenal syndrome in decompensated heart failure: role of lung-right heart-kidney interaction[J]. Int J Cardiol, 2013, 169(6): 379-384. doi: 10.1016/j.ijcard.2013.09.014
[16] Cox ZL, Testani JM. Loop diuretic resistance complicating acute heart failure[J]. Heart Fail Rev, 2020, 25(1): 133-145. doi: 10.1007/s10741-019-09851-9
[17] Rao VS, Ivey-Miranda JB, Cox ZL, et al. Natriuretic equation to predict loop diuretic response in patients with heart failure[J]. J Am Coll Cardiol, 2021, 77(6): 695-708. doi: 10.1016/j.jacc.2020.12.022
[18] Tsutsui H, Isobe M, Ito H, et al. JCS 2017/JHFS 2017 Guideline on diagnosis and treatment of acute and chronic heart failure-digest version[J]. Circ J, 2019, 83(10): 2084-2184. doi: 10.1253/circj.CJ-19-0342
[19] Raco J, Peterson B, Muallem S. Assessment of volume status in hospitalized patients with chronic heart failure[J]. Cardiol Res, 2023, 14(1): 2-11. doi: 10.14740/cr1434
[20] Thibodeau JT, Drazner MH. The role of the clinical examination in patients with heart failure[J]. JACC Heart Fail, 2018, 6(7): 543-551. doi: 10.1016/j.jchf.2018.04.005
[21] Mentz RJ, Kjeldsen K, Rossi GP, et al. Decongestion in acute heart failure[J]. Eur J Heart Fail, 2014, 16(5): 471-482. doi: 10.1002/ejhf.74
[22] Boorsma EM, Ter Maaten JM, Damman K, et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment[J]. Nat Rev Cardiol, 2020, 17(10): 641-655. doi: 10.1038/s41569-020-0379-7
[23] Ter Maaten JM, Kremer D, Demissei BG, et al. Bio-adrenomedullin as a marker of congestion in patients with new-onset and worsening heart failure[J]. Eur J Heart Fail, 2019, 21(6): 732-743. doi: 10.1002/ejhf.1437
[24] Aleksova A, Paldino A, Beltrami AP, et al. Cardiac biomarkers in the emergency department: the role of soluble ST2(sST2) in acute heart failure and acute coronary syndrome-there is meat on the bone[J]. J Clin Med, 2019, 8(2): 110.
[25] Girerd N, Seronde MF, Coiro S, et al. Integrative assessment of congestion in heart failure throughout the patient journey[J]. JACC Heart Fail, 2018, 6(4): 273-285. doi: 10.1016/j.jchf.2017.09.023
[26] Brisco MA, Coca SG, Chen J, et al. Blood urea nitrogen/creatinine ratio identifies a high-risk but potentially reversible form of renal dysfunction in patients with decompensated heart failure[J]. Circ Heart Fail, 2013, 6(2): 233-239. doi: 10.1161/CIRCHEARTFAILURE.112.968230
[27] McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[28] Stolz L, Orban M, Karam N, et al. Cardio-hepatic syndrome in patients undergoing mitral valve transcatheter edge-to-edge repair[J]. Eur J Heart Fail, 2023, 25(6): 872-884. doi: 10.1002/ejhf.2842
[29] Collins SP, Lindsell CJ, Storrow AB, et al. Prevalence of negative chest radiography results in the emergency department patient with decompensated heart failure[J]. Ann Emerg Med, 2006, 47(1): 13-18. doi: 10.1016/j.annemergmed.2005.04.003
[30] Kostuk W, Barr JW, Simon AL, et al. Correlations between the chest film and hemodynamics in acute myocardial infarction[J]. Circulation, 1973, 48(3): 624-632. doi: 10.1161/01.CIR.48.3.624
[31] De Backer D, Aissaoui N, Cecconi M, et al. How can assessing hemodynamics help to assess volume status?[J]. Intensive Care Med, 2022, 48(10): 1482-1494. doi: 10.1007/s00134-022-06808-9
[32] Gheorghiade M, Follath F, Ponikowski P, et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine[J]. Eur J Heart Fail, 2010, 12(5): 423-433. doi: 10.1093/eurjhf/hfq045
[33] Gargani L, Girerd N, Platz E, et al. Lung ultrasound in acute and chronic heart failure: a clinical consensus statement of the European Association of Cardiovascular Imaging(EACVI)[J]. Eur Heart J Cardiovasc Imaging, 2023, 24(12): 1569-1582. doi: 10.1093/ehjci/jead169
[34] Wang L, Harrison J, Dranow E, et al. Accuracy of Ultrasound Jugular Venous Pressure Height in Predicting Central Venous Congestion[J]. Ann Intern Med, 2022, 175(3): 344-351. doi: 10.7326/M21-2781
[35] Bano S, Qadeer A, Akhtar A, et al. Measurement of internal jugular vein and common carotid artery diameter ratio by ultrasound to estimate central venous pressure[J]. Cureus, 2018, 10(3): e2277.
[36] Qian X, Zhen J, Meng Q, et al. Intrarenal Doppler approaches in hemodynamics: A major application in critical care[J]. Front Physiol, 2022, 13: 951307. doi: 10.3389/fphys.2022.951307
[37] Pellicori P, Platz E, Dauw J, et al. Ultrasound imaging of congestion in heart failure: examinations beyond the heart[J]. Eur J Heart Fail, 2021, 23(5): 703-712. doi: 10.1002/ejhf.2032
[38] López-Azor JC, de la Torre N, García-Cosío Carmena MD, et al. Clinical utility of heartlogic, a multiparametric telemonitoring system, in heart failure[J]. Card Fail Rev, 2022, 8: e13. doi: 10.15420/cfr.2021.35
[39] Enghard P, Rademacher S, Nee J, et al. Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients[J]. Crit Care, 2015, 19(1): 36. doi: 10.1186/s13054-015-0756-5
[40] 中华医学会心血管病学分会心力衰竭学组和中国医师协会心力衰竭专业委员会中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004
[41] Cobo-Marcos M, Zegri-Reiriz I, Remior-Perez P, et al. Usefulness of natriuresis to predict in-hospital diuretic resistance[J]. Am J Cardiovasc Dis, 2020, 10(4): 350-355.
[42] Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary[J]. J Am Coll Cardiol, 2022, 79(17): 1757-1780. doi: 10.1016/j.jacc.2021.12.011
[43] Felker GM, Ellison DH, Mullens W, et al. Diuretic therapy for patients with heart failure: JACC state-of-the-art review[J]. J Am Coll Cardiol, 2020, 75(10): 1178-1195. doi: 10.1016/j.jacc.2019.12.059
[44] Testani JM, Hanberg JS, Cheng S, et al. Rapid and highly accurate prediction of poor loop diuretic natriuretic response in patients with heart failure[J]. Circ Heart Fail, 2016, 9(1): e002370.
[45] Rosenberg J, Gustafsson F, Galatius S, et al. Combination therapy with metolazone and loop diuretics in outpatients with refractory heart failure: an observational study and review of the literature[J]. Cardiovasc Drugs Ther, 2005, 19(4): 301-306. doi: 10.1007/s10557-005-3350-2
[46] Butler J, Anstrom KJ, Felker GM, et al. Efficacy and safety of spironolactone in acute heart failure: the ATHENA-HF randomized clinical trial[J]. JAMA Cardiol, 2017, 2(9): 950-958. doi: 10.1001/jamacardio.2017.2198
[47] 中国医师协会心力衰竭专业委员会和中华心力衰竭和心肌病杂志编辑委员会. 心力衰竭容量管理中国专家建议[J]. 中华心力衰竭和心肌病杂志(中英文), 2018, 2(1): 8-16.
[48] Jujo K, Saito K, Ishida I, et al. Randomized pilot trial comparing tolvaptan with furosemide on renal and neurohumoral effects in acute heart failure[J]. ESC Heart Fail, 2016, 3(3): 177-188. doi: 10.1002/ehf2.12088
[49] Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia[J]. N Engl J Med, 2006, 355(20): 2099-2112. doi: 10.1056/NEJMoa065181
[50] Shirakabe A, Hata N, Yamamoto M, et al. Immediate administration of tolvaptan prevents the exacerbation of acute kidney injury and improves the mid-term prognosis of patients with severely decompensated acute heart failure[J]. Circ J, 2014, 78(4): 911-921. doi: 10.1253/circj.CJ-13-1255
[51] Verbrugge FH, Martens P, Ameloot K, et al. Acetazolamide to increase natriuresis in congestive heart failure at high risk for diuretic resistance[J]. Eur J Heart Fail, 2019, 21(11): 1415-1422. doi: 10.1002/ejhf.1478
[52] Mullens W, Dauw J, Martens P, et al. Acetazolamide in acute decompensated heart failure with volume overload[J]. N Engl J Med, 2022, 387(13): 1185-1195. doi: 10.1056/NEJMoa2203094
[53] Xiangli S, Lan L, Libiya Z, et al. Effect of levosimendan combined with recombinant human brain natriuretic peptide on diuretic resistance[J]. Libyan J Med, 2021, 16(1): 1973762. doi: 10.1080/19932820.2021.1973762
[54] Kuwahara K, Nakagawa Y, Nishikimi T. Cutting edge of brain natriuretic peptide(BNP)research-the diversity of BNP immunoreactivity and its clinical relevance[J]. Circ J, 2018, 82(10): 2455-2461. doi: 10.1253/circj.CJ-18-0824
[55] Wan SH, Stevens SR, Borlaug BA, et al. Differential response to low-dose dopamine or low-dose nesiritide in acute heart failure with reduced or preserved ejection fraction: results from the ROSE AHF Trial(Renal Optimization Strategies Evaluation in Acute Heart Failure)[J]. Circ Heart Fail, 2016, 9(8): 110.
[56] Keating GM, Goa KL. Nesiritide: a review of its use in acute decompensated heart failure[J]. Drugs, 2003, 63(1): 47-70. doi: 10.2165/00003495-200363010-00004
[57] O'Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure[J]. N Engl J Med, 2011, 365(1): 32-43. doi: 10.1056/NEJMoa1100171
[58] Lytvyn Y, Bjornstad P, Udell JA, et al. Sodium glucose cotransporter-2 inhibition in heart failure: potential mechanisms, clinical applications, and summary of clinical trials[J]. Circulation, 2017, 136(17): 1643-1658. doi: 10.1161/CIRCULATIONAHA.117.030012
[59] Hallow KM, Helmlinger G, Greasley PJ, et al. Why do SGLT2 inhibitors reduce heart failure hospitalization? A differential volume regulation hypothesis[J]. Diabetes Obes Metab, 2018, 20(3): 479-487. doi: 10.1111/dom.13126
[60] Greene SJ, Bauersachs J, Brugts JJ, et al. Management of worsening heart failure with reduced ejection fraction: JACC Focus Seminar 3/3[J]. J Am Coll Cardiol, 2023, 82(6): 559-571. doi: 10.1016/j.jacc.2023.04.057
[61] Martens P, Testani J, Damman K. Prevention and treatment of diuretic resistance in acute heart failure: when to use which combination of diuretics?[J]. Eur Heart J, 2023, 44(31): 2978-2981. doi: 10.1093/eurheartj/ehad463
[62] McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure[J]. N Engl J Med, 2014, 371(11): 993-1004. doi: 10.1056/NEJMoa1409077
[63] Vardeny O, Claggett B, Kachadourian J, et al. Reduced loop diuretic use in patients taking sacubitril/valsartan compared with enalapril: the PARADIGM-HF trial[J]. Eur J Heart Fail, 2019, 21(3): 337-341. doi: 10.1002/ejhf.1402
[64] Khan J, Graham FJ, Masini G, et al. Congestion and use of diuretics in heart failure and cardiomyopathies: a practical guide[J]. Curr Cardiol Rep, 2023, 25(5): 411-420. doi: 10.1007/s11886-023-01865-y
[65] Wobbe B, Wagner J, Szabó DK, et al. Ultrafiltration is better than diuretic therapy for volume-overloaded acute heart failure patients: a meta-analysis[J]. Heart Fail Rev, 2021, 26(3): 577-585. doi: 10.1007/s10741-020-10057-7
[66] Costanzo MR, Ronco C, Abraham WT, et al. Extracorporeal ultrafiltration for fluid overload in heart failure: current status and prospects for further research[J]. J Am Coll Cardiol, 2017, 69(19): 2428-2445.
[67] Kazory A, Sgarabotto L, Ronco C. Extracorporeal ultrafiltration for acute heart failure[J]. Cardiorenal Med, 2023, 13(1): 1-8. doi: 10.1159/000527204
[68] Costanzo MR, Negoianu D, Jaski BE, et al. Aquapheresis versus intravenous diuretics and hospitalizations for heart failure[J]. JACC Heart Fail, 2016, 4(2): 95-105. doi: 10.1016/j.jchf.2015.08.005
[69] Hu J, Wan Q, Zhang Y, et al. Efficacy and safety of early ultrafiltration in patients with acute decompensated heart failure with volume overload: a prospective, randomized, controlled clinical trial[J]. BMC Cardiovasc Disord, 2020, 20(1): 447. doi: 10.1186/s12872-020-01733-5
[70] 心力衰竭超滤治疗专家组. 心力衰竭超滤治疗建议[J]. 中华心血管病杂志, 2016, 44(6): 477-482. doi: 10.3760/cma.j.issn.0253-3758.2016.06.005
-




 下载:
下载: