Clinical study of coronary microcirculation resistance in predicting the prognosis of PCI patients with acute ST-segment elevation myocardial infarction
-
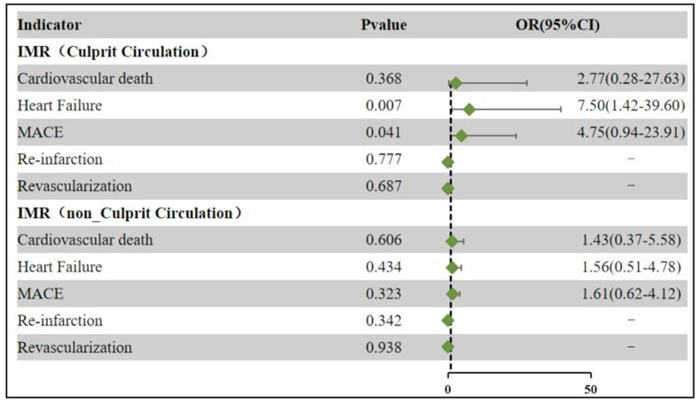
摘要: 目的 探讨冠状动脉(冠脉)微循环阻力评估急性ST段抬高型心肌梗死(STEMI)患者预后的价值。 方法 本研究是一项前瞻性、观察性、单中心研究,纳入140例成功接受急诊经皮冠脉介入(PCI)治疗的STEMI患者,使用造影微循环阻力指数(CaIMR)分析罪犯血管和非罪犯血管的微循环阻力,其中诊断冠脉微血管功能障碍(CMD)61例(CMD组),诊断非CMD 79例(非CMD组)。随访12个月,观察患者主要不良心血管事件(MACE,包括全因死亡、再次心肌梗死、因心衰住院及再次血运重建的复合结局)发生情况。采用Cox回归分析PCI术后1年MACE发生的预测因子。 结果 CMD组MACE发生率显著高于非CMD组(10.13% vs 24.60%,P<0.05)。多因素Cox回归分析显示,术后CaIMR(HR=5.887,95%CI:1.966~17.631,P<0.002)、呋塞米使用(HR=4.38,95%CI:1.595~12.026,P=0.004)、肌钙蛋白(第7天)(HR=1.011,95%CI:1.003~1.018,P=0.004)以及Killip分级(HR=1.878,95%CI:1.28~2.756,P=0.001)是STEMI患者PCI术后1年内MACE发生的独立预测因子。罪犯血管CMD与心血管性死亡、心衰发作以及主要不良事件发生率相关,非罪犯血管与各主要不良事件发生率无显著相关性。 结论 STEMI患者PCI术后的CaIMR对临床预后具有很好的预测作用。
-
关键词:
- 冠脉微循环阻力指数 /
- 主要心血管不良事件 /
- 冠状动脉微循环功能障碍 /
- 急性ST段抬高型心肌梗死
Abstract: Objective To explore the value of coronary microcirculation resistance in evaluating the prognosis of patients with acute ST-segment elevation myocardial infarction(STEMI). Methods The study was a prospective, observational, single-center study involving 140 STEMI patients who successfully received emergency percutaneous coronary intervention(PCI) treatment. The contrast microcirculatory resistance index(CaIMR) was used to analyze the microcirculation resistance of culprit and non-culprit vessels, with 61 cases diagnosed with coronary microvascular dysfunction(CMD group) and 79 cases diagnosed with non-CMD(non-CMD group). Patients were followed up for 12 months to observe the occurrence of major adverse cardiovascular events(MACE, including all-cause mortality, myocardial infarction recurrence, hospitalization due to heart failure, and revascularization). The Cox regression model was used to analyze the predictors for MACE one year after PCI. Results The incidence of MACE was significantly higher in the CMD group than in the non-CMD group(10.13% vs 24.60%, P < 0.05). Multivariate Cox regression analysis showed that postoperative CaIMR(HR=5.887, 95%CI: 1.966-17.631, P < 0.002), furosemide usage(HR=4.38, 95%CI: 1.595-12.026, P=0.004), troponin(on the 7th day)(HR=1.011, 95%CI: 1.003-1.018, P=0.004), and Killip grade(HR=1.878, 95%CI: 1.28-2.756, P=0.001) were independent predictors of MACE occurrence in one year after PCI in STEMI patients. Criminal vascular disease CMD was associated with cardiovascular death, heart failure attacks, and the incidence of major adverse events, while non-criminal blood vessels CMD was not significantly correlated with the incidence of major adverse events. Conclusion CaIMR after PCI has a good predictive effect on the clinical prognosis in patients with acute STEMI. -

-
表 1 患者基线特征
Table 1. Baseline characteristics
例(%), M(P25, P75) 项目 总体(140例) 非CMD组(79例) CMD组(61例) P 年龄/岁 64.5(57.0,70.0) 65.0(57.5,71.5) 64.5(56.0,68.0) 0.624 男性 114(81.43) 64(81.00) 50(82.00) 0.885 绝经期女性 24(17.14) 13(16.46) 11(18.03) 0.806 高血压 69(49.29) 38(48.10) 31(50.80) 0.750 糖尿病 37(26.43) 21(26.60) 16(26.20) 0.963 高脂血症 6(4.29) 5(6.30) 1(1.60) 0.348 慢性肾病 2(1.43) 1(1.30) 1(1.60) 1.000 PCI史 9(6.43) 4(5.10) 5(8.20) 0.688 当前吸烟 70(50.00) 39(49.40) 31(50.80) 0.865 冠脉旁路移植术史 1(0.71) 1(1.30) 0 0.564 Killip分级 Ⅰ 128(91.43) 72(91.10) 56(91.80) 0.889 Ⅱ 3(2.14) 2(2.50) 1(1.60) 0.597 Ⅲ 2(1.43) 2(2.50) 0 0.317 Ⅳ 7(5.00) 3(3.80) 4(6.60) 0.359 临床用药 阿司匹林 140(100.00) 79(100.00) 61(100.00) 1.000 P2Y12抑制剂 140(100.00) 79(100.00) 61(100.00) 1.000 他汀类 140(100.00) 79(100.00) 61(100.00) 1.000 β受体阻滞剂 101(72.14) 56(70.90) 45(73.80) 0.706 ACEI/ARB/ARNI 86(61.43) 49(620) 37(60.70) 0.869 螺内酯 46(32.86) 27(34.20) 19(31.10) 0.705 呋塞米 46(32.86) 28(35.40) 18(29.50) 0.458 实验室检查 BNP(首次)/(pg/mL) 81.3(28.2,293.3) 71.0(29.5,178.5) 127.5(25.0,381.0) 0.598 cTn(首次)/(ng/mL) 29.98(4.27,97.37) 32.66(2.27,100.00) 49.64(8.08,83.74) 0.287 CK-MB(首次)/(ng/mL) 43.31(4.26,209.42) 47.01(15.75,100.00) 100.00(49.64,179.72) 0.020 BNP(峰值)/(pg/mL) 632.0(342.9,998.5) 556.0(346.8,994.5) 655.5(319.0,996.0) 0.646 cTn(峰值)/(ng/mL) 58.61(21.69,132.76) 24.70(3.19,161.18) 132.51(29.71,280.06) 0.030 CK-MB(峰值)/(ng/mL) 161.18(55.48,300.00) 131.41(55.16,290.11) 200.86(66.77,300.00) 0.072 BNP(第7天)/(pg/mL) 276.41(115.72,570.50) 229.37(127.26,490.00) 320.00(115.72,642.50) 0.124 cTn(第7天)/(ng/mL) 1.86(0.39,6.06) 1.84(0.48,5.05) 3.37(0.45,6.22) 0.761 CK-MB(第7天)/(ng/mL) 2.29(1.51,3.98) 2.19(1.62,3.72) 2.50(1.55,4.61) 0.517 表 2 患者血管造影和PCI特征
Table 2. Angiography and PCI data
例(%), M(P25, P75) 项目 总体(140例) 非CMD组(79例) CMD组(61例) P 罪犯血管 左前降支 84(60.00) 50(63.30) 34(55.70) 0.366 左回旋支 14(10.00) 7(8.90) 7(11.50) 0.609 右冠脉 42(30.00) 22(27.80) 20(32.80) 0.527 多支病变 102(75.00) 61(79.20) 41(69.50) 0.194 症状发作至再通时间/h 3.32(2.20,6.43) 3.50(2.31,6.33) 3.88(2.47,7.37) 0.820 入院至血管开通时间/min 74(63,87) 79(65,88) 70.5(63,87) 0.215 糖蛋白Ⅱb/Ⅲa抑制剂使用 94(67.14) 54(68.40) 40(65.60) 0.728 血栓抽吸 48(34.29) 24(30.40) 24(39.30) 0.268 平均植入支架/枚 1 1 1 0.177 支架直径/mm 3.00(2.69,3.11) 3.00(2.75,3.00) 3.00(2.68,3.38) 0.718 支架总长度/mm 30(22,43) 30(23,46) 26(22,34) 0.067 PCI后TIMI分级 2 1(0.71) 0 1(1.6) 0.436 3 139(99.29) 79(100) 61(100) 1.000 表 3 单因素Cox回归分析结果
Table 3. Univariate Cox regression analysis results
变量 HR(95%CI) P 术后IMR 3.351(1.287~8.724) 0.013 cTn(第7天) 1.012(1.006~1.019) <0.001 呋塞米 5.205(1.999~13.551) <0.001 螺内酯 4.031(1.608~10.107) 0.003 CRP 1.010(1.001~1.018) 0.022 心率 1.025(1.001~1.049) 0.04 LVEF 0.958(0.919~0.999) 0.043 糖尿病史 2.445(1.013~5.902) 0.047 BNP(峰值) 1.000(1.000~1.001) 0.048 Killip分级 2.255(1.600~3.179) <0.001 表 4 多因素Cox回归分析
Table 4. Multivariate Cox regression analysis results
变量 HR(95%CI) P cTn(第7天) 1.011(1.003~1.018) 0.004 呋塞米 4.380(1.595~12.026) 0.004 killips分级 1.878(1.280~2.756) <0.001 术后IMR 5.887(1.966~17.631) 0.002 表 5 随访期间MACE发生情况
Table 5. MACE during follow-up
例(%) 项目 总体(140例) 非CMD组(79例) CMD组(61例) 全因死亡 8(5.71) 3(3.8) 5(8.2) 再次心肌梗死 1(1.3) 1(1.3) 0 心衰住院 15(10.71) 5(6.3) 10(16.4) 再次血运重建 2(1.43) 1(1.3) 1(1.64) 总MACE 23(16.43) 8(10.13) 15(24.60) -
[1] Zahler D, Rozenfeld KL, Pasternak Y, et al. Relation of Pain-to-Balloon Time and Mortality in Patients With ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention[J]. Am J Cardiol, 2022, 163: 38-42. doi: 10.1016/j.amjcard.2021.09.039
[2] Kalarus Z, Svendsen JH, Capodanno D, et al. Cardiac arrhythmias in the emergency settings of acute coronary syndrome and revascularization: an European Heart Rhythm Association(EHRA)consensus documen, endorsed by the European Association of Percutaneous Cardiovascular Interventions(EAPCI), and European Acute Cardiovascular Care Association(ACCA)[J]. Europace, 2019, 21(10): 1603-1604. doi: 10.1093/europace/euz163
[3] Milasinovic D, Nedeljkovic O, Maksimovic R, et al. Coronary Microcirculation: The Next Frontier in the Management of STEMI[J]. J Clin Med, 2023, 12(4): 1602. doi: 10.3390/jcm12041602
[4] Husser O, Monmeneu JV, Sanchis J, et al. Cardiovascular Magnetic Resonance-Derived Intramyocardial Hemorrhage after STEMI: Influence on Long-Term Prognosis, Adverse Left Ventricular Remodeling and Relationship with Microvascular Obstruction[J]. Int J Cardiol, 2013, 167(5): 2047-2054. doi: 10.1016/j.ijcard.2012.05.055
[5] Carrick D, Haig C, Ahmed N, et al. Comparative Prognostic Utility of Indexes of Microvascular Function Alone or in Combination in Patients with an Acute St-Segment-Elevation Myocardial Infarction[J]. Circulation, 2016, 134(23): 1833-1847. doi: 10.1161/CIRCULATIONAHA.116.022603
[6] Demirkiran A, Robbers LFHJ, van der Hoeven NW, et al. The Dynamic Relationship Between Invasive Microvascular Function and Microvascular Injury Indicators, and Their Association With Left Ventricular Function and Infarct Size at 1-Month After Reperfused ST-Segment-Elevation Myocardial Infarction[J]. Circ Cardiovasc Interv, 2022, 15(11): 892-902. doi: 10.1161/CIRCINTERVENTIONS.122.012081
[7] Silva M, Paiva L, Teixeira R, et al. Microcirculation function assessment in acute myocardial infarction: A systematic review of microcirculatory resistance indices[J]. Front Cardiovasc Med, 2022, 9: 1041444. doi: 10.3389/fcvm.2022.1041444
[8] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. Glob Heart, 2018, 13(4): 305-338. doi: 10.1016/j.gheart.2018.08.004
[9] Ai H, Feng Y, Gong Y, et al. Coronary Angiography-Derived Index of Microvascular Resistance[J]. Front Physiol, 2020, 11: 605356. doi: 10.3389/fphys.2020.605356
[10] Li J, Gong Y, Wang W, et al. Accuracy of computational pressure-fluid dynamics applied to coronary angiography to derive fractional flow reserve: FLASH FFR[J]. Cardiovascular Research, 2020, 116(7): 1349-1356. doi: 10.1093/cvr/cvz289
[11] Choi KH, Dai N, Li Y, et al. Functional Coronary Angiography-Derived Index of Microcirculatory Resistance in Patients with St-Segment Elevation Myocardial Infarction[J]. JACC Cardiovasc Interv, 2021, 14: 1670-1684. doi: 10.1016/j.jcin.2021.05.027
[12] Zhang W, Singh S, Liu L, et al. Prognostic value of coronary microvascular dysfunction assessed by coronary angiography-derived index of microcirculatory resistance in diabetic patients with chronic coronary syndrome[J]. Cardiovasc Diabetol, 2022, 21(1): 222. doi: 10.1186/s12933-022-01653-y
[13] Bhatt DL, Lopes RD, Harrington RA. Diagnosis and Treatment of Acute Coronary Syndromes: A Review[J]. JAMA, 2022, 327(7): 662-675. doi: 10.1001/jama.2022.0358
[14] 王凤华, 魏茂提, 徐宁, 等. 不同来院方式急性ST段抬高心肌梗死患者再灌注时间及院内死亡危险因素分析[J]. 临床心血管病杂志, 2022, 38(4): 298-303. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.04.009
[15] Konijnenberg LSF, Damman P, Duncker DJ, et al. Pathophysiology and diagnosis of coronary microvascular dysfunction in ST-elevation myocardial infarction[J]. Cardiovasc Res, 2020, 116(4): 787-805. doi: 10.1093/cvr/cvz301
[16] Díez-Delhoyo F, Gutiérrez-Ibañes E, Sanz-Ruiz R, et al. Prevalence of microvascular and endothelial dysfunction in the nonculprit territory in patients with acute myocardial infarction: the FISIOIAM study[J]. Circ Cardiovasc Int, 2019, 12(2): e007257. doi: 10.1161/CIRCINTERVENTIONS.118.007257
[17] van der Hoeven NW, Janssens GN, de Waard GA, et al. Temporal changes in coronary hyperemic and resting hemodynamic indices in nonculprit vessels of patients with ST-segment elevation myocardial infarction[J]. JAMA Cardiol, 2019, 4(8): 736. doi: 10.1001/jamacardio.2019.2138
[18] Elbaz M, Carrié D, Baudeux JL, et al. High frequency of endothelial vasomotor dysfunction after acute coronary syndromes in non-culprit and angiographically normal coronary arteries: a reversible phenomenon[J]. Atherosclerosis, 2005, 181(2): 311-319. doi: 10.1016/j.atherosclerosis.2005.01.007
[19] Ito H. No-reflow phenomenon in patients with acute myocardial infarction: its pathophysiology and clinical implications[J]. Acta Med Okayama, 2009, 63(4): 161-168.
[20] Dai N, Che W, Liu L, et al. Diagnostic Value of angiography-derived IMR for coronary microcirculation and its prognostic implication after PCI[J]. Front Cardiovasc Med, 2021, 8: 735743. doi: 10.3389/fcvm.2021.735743
[21] Shin D, Kim J, Choi KH, et al. Functional angiography-derived index of microcirculatory resistance validated with microvascular obstruction in cardiac magnetic resonance after STEMI[J]. Rev Esp Cardiol(Engl Ed), 2022, 75(10): 786-796.
[22] Abdu FA, Liu L, Mohammed AQ, et al. Prognostic impact of coronary microvascular dysfunction in patients with myocardial infarction with non-obstructive coronary arteries[J]. Eur J Intern Med, 2021, 92: 79-85. doi: 10.1016/j.ejim.2021.05.027
[23] Zhang W, Singh S, Liu L, et al. Prognostic value of coronary microvascular dysfunction assessed by coronary angiography-derived index of microcirculatory resistance in diabetic patients with chronic coronary syndrome[J]. Cardiovasc Diabetol, 2022, 21(1): 222. doi: 10.1186/s12933-022-01653-y
[24] Huang D, Gong Y, Fan Y, et al. Coronary angiography-derived index for assessing microcirculatory resistance in patients with non-obstructed vessels: The FLASH IMR study[J]. Am Heart J, 2023, 263: 56-63. doi: 10.1016/j.ahj.2023.03.016
[25] Li W, Takahashi T, Rios SA, et al. Diagnostic performance and prognostic impact of coronary angiography-based Index of Microcirculatory Resistance assessment: A systematic review and meta-analysis[J]. Catheter Cardiovasc Interv., 2022, 99(2): 286-292. doi: 10.1002/ccd.30076
[26] Feng C, Abdu FA, Mohammed AQ, et al. Prognostic impact of coronary microvascular dysfunction assessed by CaIMR in overweight with chronic coronary syndrome patients[J]. Front Endocrinol(Lausanne), 2022, 13: 922264. doi: 10.3389/fendo.2022.922264
[27] 李威亚, 马欢, 耿庆山. 冠状动脉微循环障碍危险因素及机制研究进展[J]. 心血管病学进展, 2021, 42(12): 1064-1068, 1080. https://www.cnki.com.cn/Article/CJFDTOTAL-XXGB202112003.htm
[28] 亓俊杰, 李世勋, 周凡, 等. 急性ST段抬高型心肌梗死患者经皮冠状动脉介入治疗后冠状动脉微循环障碍的危险因素分析[J]. 中华实用诊断与治疗杂志, 2023, 37(11): 1152-1156. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202311015.htm
[29] Pijls NH, Fearon WF, Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME(fractional flow reserve versus angiography for multivessel evaluation)study[J]. J Am Coll Cardiol, 2010, 56(3): 177-184. doi: 10.1016/j.jacc.2010.04.012
[30] Taqueti VR, Everett BM, Murthy VL, et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease[J]. Circulation, 2015, 131(6): 528-535. doi: 10.1161/CIRCULATIONAHA.114.009716
[31] 陈冬生, 栾献亭, 杨进刚, 等. 中国急性心肌梗死不同Killip分级患者的临床特征、治疗和预后情况分析[J]. 中国循环杂志, 2016, 31(9): 849-853. doi: 10.3969/j.issn.1000-3614.2016.09.005
[32] Wang Y, Wang XD, Yao JW, et al. The Impact of the Duration of Cardiac Troponin I Elevation on the Clinical Prognosis as Well as Incidence of New-Onset Atrial Fibrillation Respectively in Elderly Non-ST-Elevation Acute Myocardial Infarction Patients without PCI[J]. J Inflamm Res, 2021, 14: 6907-6916. doi: 10.2147/JIR.S345576
[33] Flores CH, Díez-Delhoyo F, Sanz-Ruiz R, et al. Microvascular dysfunction of the non-culprit circulation predicts poor prognosis in patients with ST-segment elevation myocardial infarction[J]. Int J Cardiol Heart Vasc, 2022, 39: 100997.
[34] de Waard GA, Hollander MR, Teunissen PF, et al. Changes in coronary blood flow after acute myocardial infarction: insights from a patient study and an experimental porcine model[J]. JACC Cardiovasc Int, 2016, 9(6): 602-613. doi: 10.1016/j.jcin.2016.01.001
-




 下载:
下载: