Correlation between the serum Gla rich protein level and the degree of coronary artery calcification in patients with unstable angina
-
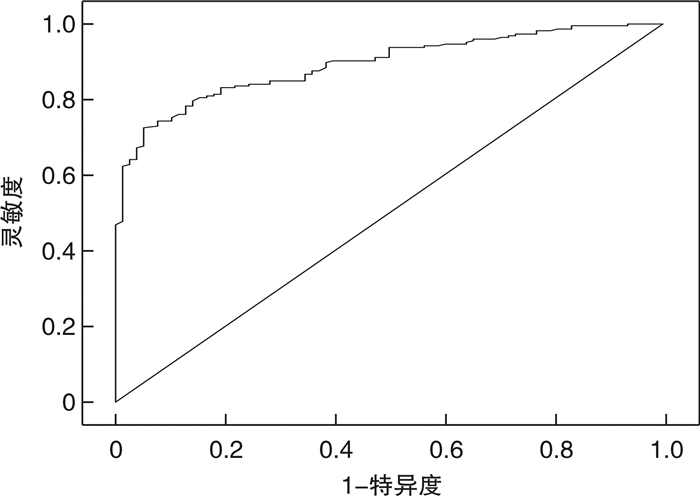
摘要: 目的 探讨不稳定型心绞痛(UA)患者血清富含Gla蛋白水平(GRP)与冠状动脉(冠脉)钙化程度的关系,为冠脉钙化的诊断和评估提供依据。方法 选取衡水市人民医院心血管内科诊断的UA患者304例为研究对象。行冠脉双源CT扫描,采用Agatston修正法计算冠脉钙化积分(CACS)。根据CACS,将患者分为无钙化组(CACS=0,78例)、少量钙化组(1≤CACS≤10,48例)、轻度钙化组(11≤CACS≤100,60例)、中度钙化组(101≤CACS≤399,68例)和重度钙化组(400≤CACS,50例)。比较各组患者血清GRP水平。采用logistic回归分析筛选冠脉钙化的影响因素,采用Spearman相关性分析探讨血清GRP水平与冠脉钙化的相关性,采用ROC分析评估GRP水平诊断冠脉钙化的价值。结果 总体来看,随着冠脉钙化程度的加重,GRP水平有逐渐降低趋势(均P<0.05)。多因素logistic回归分析结果显示,血清GRP水平是冠脉钙化的独立保护因素(OR=0.156,95%CI:0.113~0.217,P<0.05)。Spearman相关性分析显示,血清GRP水平与冠脉钙化程度呈负相关性(r=-0.858,P<0.05)。ROC分析显示,GRP预测冠脉钙化的曲线下面积为0.893(95%CI:0.857~0.928),截点值为22.68 ng/mL,灵敏度为72.6%,特异度为94.9%。结论 UA患者血清GRP水平与冠脉钙化程度呈负相关性,是冠脉钙化的独立保护因素,且对冠脉钙化有一定的诊断价值。Abstract: Objective To investigate the relationship between serum Gla-rich protein level (GRP) and the degree of coronary artery calcification in patients with unstable angina (UA), and to provide evidence for the diagnosis and evaluation of coronary artery calcification.Methods A total of 304 patients diagnosed with UA in the Department of Cardiology at Hengshui People's Hospital were selected as subjects. Coronary double-source CT scan was performed, and coronary vascular calcification scores (CACS) were calculated using Agatston correction method. According to CACS, all patients were divided into the non-calcification group (CACS=0, n=78), small-calcification group (1≤CACS≤10, n=48), mild-calcification group (11≤CACS≤100, n=60), moderate-calcification group (101≤CACS≤399, n=68), and severe-calcification group (400≤CACS, n=50). GRP levels in each group were compared. Logistic regression analysis was used to screen the influencing factors of coronary artery calcification, Spearman correlation analysis was used to explore the correlation between serum GRP levels and coronary artery calcification, ROC analysis was used to evaluate the diagnostic value of GRP levels in coronary artery calcification.Results Generally, the levels of serum GRP decreased gradually with the increase of coronary calcification degree (all P<0.05). Multivariate logistic regression analysis showed that serum GRP level was an independent protective factor for coronary artery calcification (OR=0.156, 95%CI: 0.113-0.217, P<0.05). Spearman correlation analysis showed that serum GRP level was negatively correlated with the degree of coronary artery calcification (r=-0.858, P<0.05). ROC analysis showed that the area under the curve for predicting coronary artery calcification using GRP was 0.893 (95%CI: 0.857-0.928), with a cutoff value of 22.68 ng/mL, sensitivity of 72.6%, and specificity of 94.9%.Conclusion Serum GRP level in UA patients is negatively correlated with the degree of coronary artery calcification. GRP is an independent protective factor for coronary artery calcification and has significant diagnostic value.
-
Key words:
- Gla rich protein /
- coronary artery calcification /
- unstable angina
-

-
表 1 不同钙化组患者临床资料比较
Table 1. Clinical data
例(%), X±S 项目 无钙化组(78例) 少量钙化组(48例) 轻度钙化组(60例) 中度钙化组(68例) 重度钙化组(50例) 男性 49(62.82) 32(66.67) 31(51.67) 36(52.94) 40(80.00) 吸烟 36(46.15) 26(54.17) 22(36.67) 25(36.76) 33(66.00) 高血压 30(38.46) 24(50.00) 35(58.33) 46(67.65) 30(60.00)1) 糖尿病 23(29.49) 30(62.50) 41(68.33) 51(75.00) 42(84.00)1) 年龄/岁 61.55±8.87 61.31±9.34 62.35±9.26 62.51±7.67 65.48±7.25 TG/(mmol/L) 1.34±0.36 1.35±0.48 1.36±0.42 1.40±0.38 1.42±0.401) TC/(mmol/L) 3.66±0.78 3.72±0.85 5.23±0.95 5.67±0.82 6.03±0.881) HDL-C/(mmol/L) 1.32±0.42 1.18±0.46 1.07±0.45 1.03±0.33 0.92±0.37 LDL-C/(mmol/L) 2.75±0.89 3.17±0.76 3.37±0.88 3.74±0.96 3.86±0.84 Lp(a)/(mg/dL) 12.65±2.66 12.81±2.75 12.79±2.68 13.18±2.64 14.44±2.55 hs-CRP/(mg/L) 3.55±1.26 6.08±3.26 6.03±3.17 6.25±2.66 8.27±3.67 CREA/(μmol/L) 59.84±2.67 57.98±2.74 58.66±2.82 61.68±2.62 61.97±2.85 Ca/(mmol/L) 2.32±0.74 2.15±0.85 2.13±0.68 2.25±0.92 2.26±0.72 GRP/(ng/mL) 23.82±0.77 23.57±0.65 22.07±0.681)2) 21.86±0.651)2) 18.26±0.681)2)3)4) 与无钙化组比较,1)P<0.05;与少量钙化组比较,2)P<0.05;与轻度钙化组比较,3)P<0.05;与中度钙化组比较,4)P<0.05。 表 2 冠脉钙化的影响因素
Table 2. The influencing factors of coronary artery calcification
因素 β SE Wald P OR 95%CI TC 0.991 0.152 42.348 <0.05 2.694 1.998~3.630 HDL-C -1.108 0.336 10.867 <0.05 0.330 0.171~0.638 LDL-C 0.399 0.155 6.607 <0.05 1.490 1.099~2.020 hs-CRP 0.193 0.051 14.584 <0.05 1.213 1.098~1.339 GRP -1.856 0.167 123.030 <0.05 0.156 0.113~0.217 CREA 0.163 0.049 10.875 <0.05 1.177 1.068~1.296 Lp(a) 0.131 0.052 6.196 <0.05 1.140 1.028~1.263 高血压(无) -0.778 0.279 7.759 <0.05 0.459 0.265~0.794 糖尿病(无) -1.205 0.289 17.406 <0.05 0.300 0.170~0.528 表 3 血清GRP水平与生化指标及冠脉钙化程度的相关性分析
Table 3. The correlation between serum GRP levels, biochemical indicators, and degree of coronary artery calcification
指标 TG TC LDL-C HDL-C CREA Lp(a) hs-CRP Ca 冠脉钙化程度 GRP r -0.078 -0.580 -0.365 0.259 -0.285 -0.182 -0.412 -0.043 -0.858 P >0.05 <0.05 <0.05 <0.05 <0.05 <0.05 <0.05 >0.05 <0.05 -
[1] 曾秋棠, 彭昱东. 冠状动脉钙化的最新诊断与介入治疗进展[J]. 临床心血管病杂志, 2023, 39(5): 332-336. doi: 10.13201/j.issn.1001-1439.2023.05.002
[2] Onnis C, Virmani R, Kawai K, et al. Coronary artery calcification: current concepts and clinical implications[J]. Circulation, 2024, 149(3): 251-266. doi: 10.1161/CIRCULATIONAHA.123.065657
[3] Whelton SP, Blaha MJ. Coronary artery calcium: from risk prediction to treatment allocation and clinical trials[J]. Heart, 2023, 109(22): 1714-1721. doi: 10.1136/heartjnl-2022-321711
[4] Silva AP, Viegas CS, Mendes F, et al. Gla-rich protein(GRP)as an early and novel marker of vascular calcification and kidney dysfunction in diabetic patients with CKD: a pilot cross-sectional study[J]. J Clin Med, 2020, 9(3): 635. doi: 10.3390/jcm9030635
[5] Zhelyazkova-Savova MD, Yotov YT, Nikolova MN, et al. Statins, vascular calcification, and vitamin K-dependent proteins: Is there a relation?[J]. Kaohsiung J Med Sci, 2021, 37(7): 624-631. doi: 10.1002/kjm2.12373
[6] Düsing P, Zietzer A, Goody PR, et al. Vascular pathologies in chronic kidney disease: pathophysiological mechanisms and novel therapeutic approaches[J]. J Mol Med, 2021, 99(3): 335-348. doi: 10.1007/s00109-021-02037-7
[7] 柯元南, 陈纪林. 不稳定性心绞痛和非ST段抬高心肌梗死诊断与治疗指南[J]. 中华心血管病杂志, 2007, 35(4): 295-304. doi: 10.3760/j.issn:0253-3758.2007.04.003
[8] 张瑞芬, 苏和, 黄新生, 等. 不稳定型心绞痛中医诊疗专家共识[J]. 中医杂志, 2022, 63(7): 695-700. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZYZ202207016.htm
[9] 杨义文, 胡春洪. 冠状动脉钙化积分的临床研究[J]. 中国临床医生杂志, 2023, 51(11): 1269-1271. doi: 10.3969/j.issn.2095-8552.2023.11.003
[10] Rampidis GP, Benetos G, Benz DC, et al. A guide for Gensini Score calculation[J]. Atherosclerosis, 2019, 287: 181-183. doi: 10.1016/j.atherosclerosis.2019.05.012
[11] Rifai MA, Blaha MJ, Patel J, et al. Coronary artery calcification, statin use and long-term risk of atherosclerotic cardiovascular disease events(from the multi-ethnic study of atherosclerosis)[J]. Am J Cardiol, 2020, 125(6): 835-839. doi: 10.1016/j.amjcard.2019.12.031
[12] 王伟民, 霍勇, 葛均波. 冠状动脉钙化病变诊治中国专家共识(2021版)[J]. 中国介入心脏病学杂志, 2021, 29(5): 251-259. doi: 10.3969/j.issn.1004-8812.2021.05.002
[13] 杨敏, 林章宇, 丰雷, 等. 冠状动脉造影评估的靶病变钙化程度对接受经皮冠状动脉介入治疗患者手术即刻成功率和长期预后的影响[J]. 中国循环杂志, 2023, 38(12): 1239-1245. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202312001.htm
[14] Bäck M, Aranyi T, Cancela ML, et al. Endogenous calcification inhibitors in the prevention of vascular calcification: a consensus statement from the COST action EuroSoftCalcNet[J]. Front Cardiovasc Med, 2018, 5: 196.
[15] 吴志茹, 王梦慈, 吴雪平, 等. 血清去磷酸化未羧化基质Gla蛋白和维生素K2水平与慢性肾脏病患者血管钙化相关性研究[J]. 中国血液净化, 2022, 21(4): 253-257. doi: 10.3969/j.issn.1671-4091.2022.04.007
[16] 龚心文, 蔡海军, 李伟, 等. 血清CLU、MGP水平与急性冠状动脉综合征患者炎性反应、糖脂代谢及心功能指标的相关性[J]. 疑难病杂志, 2020, 19(12): 1200-1204. doi: 10.3969/j.issn.1671-6450.2020.12.004
[17] 方向南, 柯瑞琼, 洪世华, 等. 血清去磷酸化未羧化基质gla蛋白水平与2型糖尿病合并冠状动脉粥样硬化性心脏病的相关性研究[J]. 中国糖尿病杂志, 2021, 29(3): 168-172. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGTL202103002.htm
[18] 李勇, 李占虎, 闫小菊, 等. 冠心病患者血清基质Gla蛋白水平与冠状动脉钙化程度相关性研究[J]. 东南大学学报(医学版), 2019, 38(1): 72-76. https://www.cnki.com.cn/Article/CJFDTOTAL-NJTD201901015.htm
[19] Cancela ML, Conceição N, Laizé V. Gla-rich protein, a new player in tissue calcification?[J]. Adv Nutr, 2012, 3(2): 174-181. doi: 10.3945/an.111.001685
[20] Pescatore LA, Gamarra LF, Liberman M. Multifaceted mechanisms of vascular calcification in aging[J]. Arterioscler Thromb Vasc Biol, 2019, 39(7): 1307-1316. doi: 10.1161/ATVBAHA.118.311576
[21] Icer MA, Yıldıran H. Effects of fetuin-a with diverse functions and multiple mechanisms on human health[J]. Clin Biochem, 2021, 88: 1-10. doi: 10.1016/j.clinbiochem.2020.11.004
[22] 梁英权, 段亚君, 韩际宏. 血管钙化分子机制研究进展[J]. 中国动脉硬化杂志, 2020, 28(11): 921-929. doi: 10.3969/j.issn.1007-3949.2020.11.002
[23] Willems BA, Furmanik M, Caron MMJ, et al. Ucma/GRP inhibits phosphate-induced vascular smooth muscle cell calcification via SMAD-dependent BMP signalling[J]. Sci Rep, 2018, 8(1): 4961.
[24] Demirci R, Sevinc C. The relationship between carotid intima media thickness, inflammation and GLA rich protein levels in chronic kidney disease[J]. Int J Gen Med, 2021, 14: 5119-5126.
[25] Viegas CSB, Araújo N, Carreira J, et al. Nanoencapsulation of gla-rich protein(GRP)as a novel approach to target inflammation[J]. Int J Mol Sci, 2022, 23(9): 4813.
[26] Viegas CSB, Simes DC. A dual role for GRP in cardiovascular disease[J]. Aging(Albany NY), 2019, 11(5): 1323-1324.
[27] Viegas CSB, Santos L, Macedo AL, et al. Chronic kidney disease circulating calciprotein particles and extracellular vesicles promote vascular calcification: a role for GRP(gla-rich protein)[J]. Arterioscler Thromb Vasc Biol, 2018, 38(3): 575-587.
[28] Lee SJ, Lee IK, Jeon JH. Vascular calcification-new insights into its mechanism[J]. Int J Mol Sci, 2020, 21(8): E2685.
-




 下载:
下载: