The role of coronary microvascular disease induced by estrogen level changes in the pathogenesis of heart failure with preserved ejection fraction
-
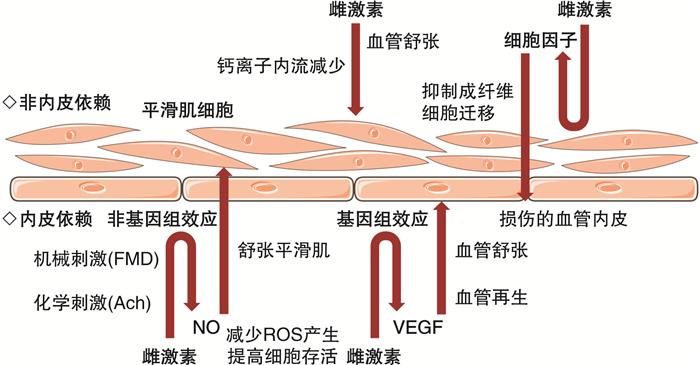
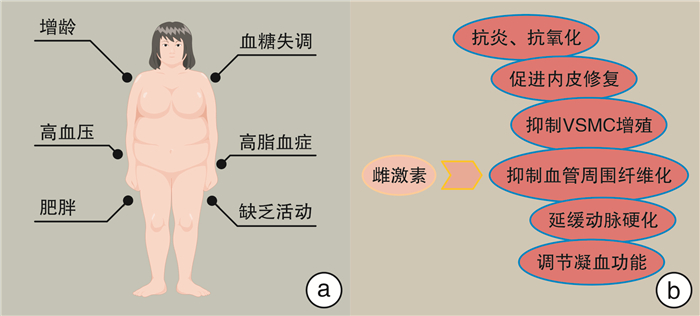
摘要: 心力衰竭(心衰)是一种严重的心脏疾病,其发病率和病死率高,目前的治疗方法效果有限。射血分数保留型心衰(HFpEF)是心衰的常见类型之一,主要表现为左心室舒张功能障碍,其中绝经后的女性是易患人群。绝经后雌激素水平的变化在HFpEF发病中可能起重要作用。本综述旨在综合分析与雌激素水平变化相关的冠状动脉微血管病变在HFpEF发生发展中的可能作用,并为进一步的病理生理机制研究以及HFpEF和微血管病变中与雌激素相关的预防和治疗研究提供基础。
-
关键词:
- 心力衰竭,射血分数保留型 /
- 微循环 /
- 雌激素 /
- 绝经期
Abstract: Heart failure(HF) is a severe cardiovascular disease with high morbidity and mortality, and currently lacks effective treatment options. Heart failure with preserved ejection fraction(HFpEF) is a common subtype of HF, characterized by impaired left ventricular diastolic function, with postmenopausal women being the predominant affected population. Fluctuations in estrogen levels are believed to play a significant role in the pathogenesis of HFpEF. This review aims to comprehensively analyze the impact of coronary microvascular disease induced by changes in estrogen levels on the development of HFpEF, and provide a foundation for further research on the underlying pathological and physiological mechanisms, as well as the prevention and treatment strategies related to estrogen in HFpEF and microvascular diseases.-
Key words:
- heart failure with preserved ejection fraction /
- microcirculation /
- estrogen /
- menopause
-

-
[1] 中华医学会心血管病学分会, 中国医师协会心血管内科医师分会, 中国医师协会心力衰竭专业委员会, 等. 中国心力衰竭诊断和治疗指南2024[J]. 中华心血管病杂志, 2024, 52(3): 235-275. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202406002.htm
[2] 射血分数保留的心力衰竭诊断与治疗中国专家共识制定工作组. 射血分数保留的心力衰竭诊断与治疗中国专家共识2023[J]. 中国循环杂志, 2023, 38(4): 375-393. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202304014.htm
[3] McDonagh TA, Metra M, Adamo M, et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2023, 44(37): 3627-3639. doi: 10.1093/eurheartj/ehad195
[4] da Silva JD, Montagnoli T, de Sá MPL, et al. Heart failure in menopause: treatment and new approaches[J]. Intern J Mol Sci, 2022, 23(23): 15140. doi: 10.3390/ijms232315140
[5] Qian CY, Liu JJ, Liu HD. Targeting estrogen receptor signaling for treating heart failure[J]. Heart Fail Rev, 2024, 29(1): 125-131.
[6] Adekunle AO, Adzika GK, Mprah R, et al. Predominance of heart failure with preserved ejection fraction in postmenopausal women: intra-and extra-cardiomyocyte maladaptive alterations scaffolded by estrogen deficiency[J]. Front Cell Dev Biol, 2021, 9: 685996. doi: 10.3389/fcell.2021.685996
[7] Sickinghe AA, Korporaal SJA, den Ruijter HM, et al. Estrogen contributions to microvascular dysfunction evolving to heart failure with preserved ejection fraction[J]. Front Endocrinol, 2019, 10: 442. doi: 10.3389/fendo.2019.00442
[8] Smilowitz NR, Toleva O, Chieffo A, et al. Coronary microvascular disease in contemporary clinical practice[J]. Circ Cardiovasc Interv, 2023, 16(6): e012568.
[9] Dryer K, Gajjar M, Narang N, et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction[J]. Am J Physiol Heart Circ Physiol, 2018, 314(5): H1033-H1042. doi: 10.1152/ajpheart.00680.2017
[10] Mohammed AQ, Abdu FA, Su Y, et al. Prognostic significance of coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction[J]. Can J Cardiol, 2023, 39(7): 971-980. doi: 10.1016/j.cjca.2023.04.011
[11] Shah SJ, Lam CSP, Svedlund S, et al. Prevalence and correlates of coronary microvasculardysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF[J]. Eur Heart J, 2018, 39(37): 3439-3450. doi: 10.1093/eurheartj/ehy531
[12] Hage C, Svedlund S, Saraste A, et al. Association of coronary microvascular dysfunction with heart failure hospitalizations and mortality in heart failure with preserved ejection fraction: a follow-up in the PROMIS-HFpEF study[J]. J Card Fail, 2020, 26(11): 1016-1021. doi: 10.1016/j.cardfail.2020.08.010
[13] Taqueti VR, Solomon SD, Shah AM, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction[J]. Eur Heart J, 2018, 39(10): 840-849. doi: 10.1093/eurheartj/ehx721
[14] Wang Y, Zhang J, Wang Z, et al. Endothelial-cell-mediated mechanism of coronary microvascular dysfunction leading to heart failure with preserved ejection fraction[J]. Heart Fail Rev, 2023, 28(1): 169-178.
[15] Fopiano KA, Jalnapurkar S, Davila AC, et al. Coronary Microvascular Dysfunction and Heart Failure with Preserved Ejection Fraction-implications for Chronic Inflammatory Mechanisms[J]. Curr Cardiol Rev, 2022, 18(2): e310821195986. doi: 10.2174/1573403X17666210831144651
[16] 黄鈺婷, 张恺, 苏菁, 等. 射血分数保留型心力衰竭与微血管内皮炎症[J]. 临床心血管病杂志, 2021, 37(6): 512-515. doi: 10.13201/j.issn.1001-1439.2021.06.004
[17] Sinha A, Rahman H, Perera D. Coronary microvascular dysfunction and heart failure with preserved ejection fraction: what are the mechanistic links?[J]. Curr Opin Cardiol, 2023, 38(6): 521-526. doi: 10.1097/HCO.0000000000001082
[18] Tona F, Montisci R, Iop L, et al. Role of coronary microvascular dysfunction in heart failure with preserved ejection fraction[J]. Rev Cardiovasc Med, 2021, 22(1): 97-104. doi: 10.31083/j.rcm.2021.01.277
[19] Mohammed SF, Hussain S, Mirzoyev SA, et al. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction[J]. Circulation, 2015, 131(6): 550-559. doi: 10.1161/CIRCULATIONAHA.114.009625
[20] Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium: the role of antiangiogenic factors and implications for later cardiovascular disease[J]. Circulation, 2011, 123(24): 2856-2869. doi: 10.1161/CIRCULATIONAHA.109.853127
[21] Ganz P, Hsue PY. Assessment of structural disease in the coronary microvasculature[J]. Circulation, 2009, 120(16): 1555-1557. doi: 10.1161/CIRCULATIONAHA.109.899336
[22] Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction comorbidities drive myocardial dysfunction and remodeling through coronary microvascularendothelial inflammation[J]. J Am Coll Cardiol, 2013, 62(4): 263-271. doi: 10.1016/j.jacc.2013.02.092
[23] Goligorsky MS. Microvascular rarefaction: the decline and fall of blood vessels[J]. Organogenesis, 2010, 6(1): 1-10. doi: 10.4161/org.6.1.10427
[24] Nelson MD, Wei J, Bairey Merz CN. Coronary microvascular dysfunction and heart failure with preserved ejection fraction as female-pattern cardiovascular disease: the chicken or the egg?[J]. Eur Heart J, 2018, 39(10): 850-852. doi: 10.1093/eurheartj/ehx818
[25] Franssen C, Chen S, Unger A, et al. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction[J]. JACC Heart Fail, 2016, 4(4): 312-324. doi: 10.1016/j.jchf.2015.10.007
[26] Chandramouli C, Ting TW, Tromp J, et al. Sex differences in proteomic correlates of coronary microvascular dysfunction among patients with heart failure and preserved ejection fraction[J]. Eur J Heart Fail, 2022, 24(4): 681-684. doi: 10.1002/ejhf.2435
[27] Tunc E, Eve AA, Madak-Erdogan Z. Coronary microvascular dysfunction and estrogen receptor signaling[J]. Trends Endocrinol Metab, 2020, 31(3): 228-238. doi: 10.1016/j.tem.2019.11.001
[28] Pei J, Harakalova M, den Ruijter H, et al. Cardiorenal disease connection during post-menopause: The protective role of estrogen in uremic toxins induced microvascular dysfunction[J]. Int J Cardiol, 2017, 238: 22-30. doi: 10.1016/j.ijcard.2017.03.050
[29] Fuentes N, Silveyra P. Estrogen receptor signaling mechanisms[J]. Adv Protein Chem Struct Biol, 2019, 116: 135-170.
[30] Nevzati E, Shafighi M, Bakhtian KD, et al. Estrogen induces nitric oxide production via nitric oxide synthase activation in endothelial cells[J]. Acta Neurochir Suppl, 2015, 120: 141-145.
[31] Gourdy P, Guillaume M, Fontaine C, et al. Estrogen receptor subcellular localization and cardiometabolism[J]. Mol Metab, 2018, 15: 56-69. doi: 10.1016/j.molmet.2018.05.009
[32] Stirone C, Duckles SP, Krause DN, et al. Estrogen increases mitochondrial efficiency and reduces oxidative stress in cerebral blood vessels[J]. Mol Pharmacol, 2005, 68(4): 959-965. doi: 10.1124/mol.105.014662
[33] Wang H, Sun X, Lin MS, et al. G protein-coupled estrogen receptor(GPER)deficiency induces cardiac remodeling through oxidative stress[J]. Transl Res, 2018, 199: 39-51. doi: 10.1016/j.trsl.2018.04.005
[34] Debortoli AR, Rouver WDN, Delgado NTB, et al. GPER modulates tone and coronary vascular reactivity in male and female rats[J]. J Mol Endocrinol, 2017, 59(2): 171-180. doi: 10.1530/JME-16-0117
[35] Tarhouni K, Guihot AL, Vessieres E, et al. Estrogens are needed for the improvement in endothelium-mediated dilation induced by a chronic increase in blood flow in rat mesentericarteries[J]. Vascul Pharmacol, 2016, 80: 35-42. doi: 10.1016/j.vph.2015.10.004
[36] Li G, Chen YF, Kelpke SS, et al. Estrogen attenuates integrin-beta(3)-dependent adventitial fibroblast migration after inhibition of osteopontin production in vascular smooth muscle cells[J]. Circulation, 2000, 101(25): 2949-2955. doi: 10.1161/01.CIR.101.25.2949
[37] Mazzuca MQ, Mata KM, Li W, et al. Estrogen receptor subtypes mediate distinct microvascular dilation and reduction in[Ca2+]I in mesenteric microvessels of female rat[J]. J Pharmacol Exp Ther, 2015, 352(2): 291-304. doi: 10.1124/jpet.114.219865
[38] Hill BJF, Dalton RJ, Joseph BK, et al. 17β-estradiol reduces Cav1.2 channel abundance and attenuates Ca2+-dependent contractions in coronary arteries[J]. Pharmacol Res Perspect, 2017, 5(5): e00358.
[39] Thijssen DH, Black MA, Pyke KE, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline[J]. Am J Physiol Heart Circ Physiol, 2011, 300(1): H2-12. doi: 10.1152/ajpheart.00471.2010
[40] Usselman CW, Stachenfeld NS, Bender JR. The molecular actions of oestrogen in the regulation of vascular health[J]. Exp Physiol, 2016, 101(3): 356-361.
[41] Skaug EA, Aspenes ST, Oldervoll L, et al. Age and gender differences of endothelial function in 4739 healthy adults: the HUNT3 Fitness Study[J]. Eur J Prev Cardiol, 2013, 20(4): 531-540.
[42] Yim SF, Lau TK, Sahota DS, et al. Prospective randomized study of the effect of"add-back"hormone replacement on vascular function during treatment with gonadotropin-releasing hormone agonists[J]. Circulation, 1998, 98(16): 1631-1635.
[43] Lambert J, Stehouwer CD. Modulation of endothelium-dependent, flow-mediated dilatation of the brachial artery by sex and menstrual cycle[J]. Circulation, 1996, 94(9): 2319-2320.
[44] Williams MRI, Westerman RA, Kingwell BA, et al. Variations in endothelial function and arterial compliance during the menstrual cycle[J]. J Clin Endocrinol Metab, 2001, 86(11): 5389-5395.
[45] Sudhir K, Chou TM, Messina LM, et al. Endothelial dysfunction in a man with disruptive mutation in oestrogen-receptor gene[J]. Lancet, 1997, 349(9059): 1146-1147.
[46] Meendering JR, Torgrimson BN, Miller NP, et al. Estrogen, medroxyprogesterone acetate, endothelial function, and biomarkers of cardiovascular risk in young women[J]. Am J Physiol Heart Circ Physiol, 2008, 294(4): H1630-H1637.
[47] Lieberman EH, Gerhard MD, Uehata A, et al. Estrogen improves endothelium-dependent, flow-mediated vasodilation in postmenopausal women[J]. Ann Intern Med, 1994, 121(12): 936-941.
[48] Gilligan DM, Badar DM, Panza JA, et al. Acute vascular effects of estrogen in postmenopausal women[J]. Circulation, 1994, 90(2): 786-791.
[49] Chen ZQ, Wu CM, Huang ZQ. Association between estrogen replacement therapy and heart failure in postmenopausal women: a systematic review and meta-analysis[J]. Prev Med, 2024, 181: 107909.
-




 下载:
下载: