The release mechanisms and clinical significance of elevated cardiac troponin in non-cardiac diseases
-
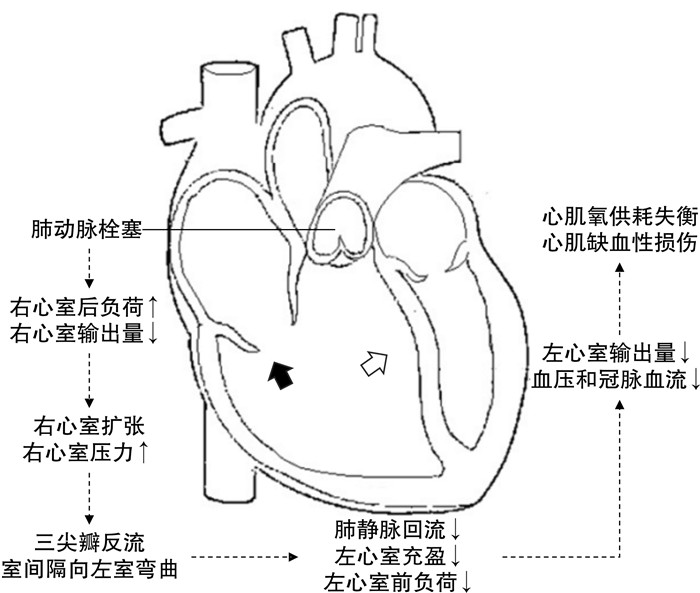
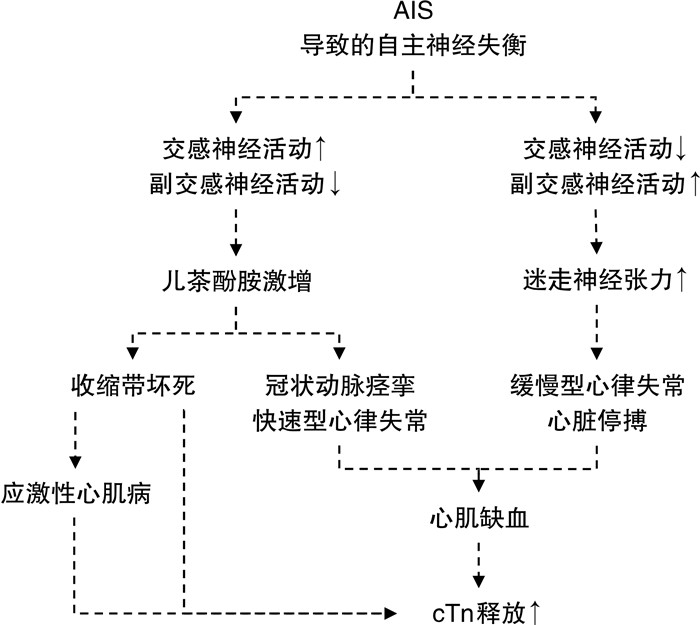
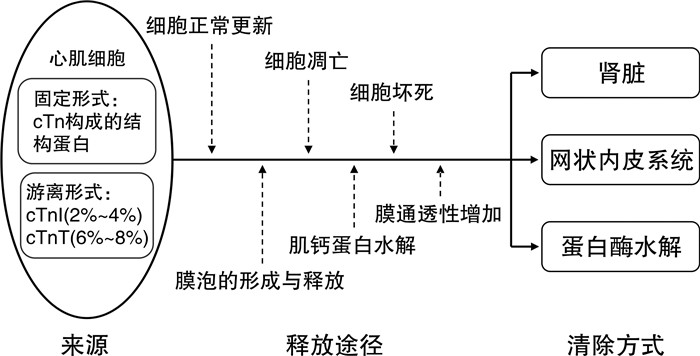
摘要: 心肌肌钙蛋白(cardiac troponin,cTn)是一种存在于心肌细胞内的特异性标志物。当心肌出现可逆或不可逆性损伤时,cTn被释放入循环。除造成心肌损伤的常见心脏疾病外,临床中也能观察到非心脏疾病患者cTn升高。为能正确理解这种升高的意义,本文在介绍cTn来源、释放方式和清除途径的基础上,着重探讨非心脏疾病中cTn升高的机制及其临床价值。Abstract: Cardiac troponin (cTn) is a specific biomarker present within myocardial cells. When the myocardium undergoes reversible or irreversible damage, cTn is released into circulation. While elevated levels of cTn are commonly associated with cardiac diseases, they can also be observed in patients with non-cardiac conditions. To accurately comprehend the significance of cTn elevation, our review explores the mechanisms and clinical implications of elevated cTn in non-cardiac diseases, building upon the introduction of the origin, release mechanisms, and clearance pathways.
-
Key words:
- cardiac troponin /
- non-cardiac diseases /
- myocardial injury /
- prognosis
-

-
[1] Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes[J]. Eur Heart J Acute Cardiovasc Care, 2024, 13(1): 55-161. doi: 10.1093/ehjacc/zuad107
[2] 杨昕宇, 吴倩芸, 吴奕霖, 等. 暴发性心肌炎短期死亡的危险因素及其列线图预测模型的建立及验证: 回顾性分析[J]. 临床心血管病杂志, 2023, 39(3): 225-230. doi: 10.13201/j.issn.1001-1439.2023.03.013
[3] Chaulin AM. Some common causes of false positive increases in serum levels of cardiac troponins[J]. Curr Cardiol Rev, 2022, 18(6): e130422203527. doi: 10.2174/1573403X18666220413124038
[4] Mair J, Lindahl B, Hammarsten O, et al. How is cardiac troponin released from injured myocardium?[J]. Eur Heart J Acute Cardiovasc Care, 2018, 7(6): 553-560. doi: 10.1177/2048872617748553
[5] Park KC, Gaze DC, Collinson PO, et al. Cardiac troponins: from myocardial infarction to chronic disease[J]. Cardiovasc Res, 2017, 113(14): 1708-1718. doi: 10.1093/cvr/cvx183
[6] Stark M, Kerndt CC, Sharma S. Troponin[M]. In: StatPearls. Treasure Island(FL): StatPearls Publishing. Copyright© 2023, StatPearls Publishing LLC.; 2023.
[7] Hickman PE, Potter JM, Aroney C, et al. Cardiac troponin may be released by ischemia alone, without necrosis[J]. Clin Chim Acta, 2010, 411(5-6): 318-323. doi: 10.1016/j.cca.2009.12.009
[8] Starnberg K, Jeppsson A, Lindahl B, et al. Revision of the troponin T release mechanism from damaged human myocardium[J]. Clin Chem, 2014, 60(8): 1098-1104. doi: 10.1373/clinchem.2013.217943
[9] Eggers KM, Lindahl B. Application of cardiac troponin in cardiovascular diseases other than acute coronary syndrome[J]. Clin Chem, 2017, 63(1): 223-235. doi: 10.1373/clinchem.2016.261495
[10] Amgalan D, Pekson R, Kitsis RN. Troponin release following brief myocardial ischemia: apoptosis versus necrosis[J]. JACC Basic Transl Sci, 2017, 2(2): 118-121. doi: 10.1016/j.jacbts.2017.03.008
[11] Dunn ME, Coluccio D, Hirkaler G, et al. The complete pharmacokinetic profile of serum cardiac troponin I in the rat and the dog[J]. Toxicol Sci, 2011, 123(2): 368-373. doi: 10.1093/toxsci/kfr190
[12] Fridén V, Starnberg K, Muslimovic A, et al. Clearance of cardiac troponin T with and without kidney function[J]. Clin Biochem, 2017, 50(9): 468-474. doi: 10.1016/j.clinbiochem.2017.02.007
[13] Müller-Bardorff M, Weidtmann B, Giannitsis E, et al. Release kinetics of cardiac troponin T in survivors of confirmed severe pulmonary embolism[J]. Clin Chem, 2002, 48(4): 673-675. doi: 10.1093/clinchem/48.4.673
[14] Kim JY, Kim KH, Cho JY, et al. D-dimer/troponin ratio in the differential diagnosis of acute pulmonary embolism from non-ST elevation myocardial infarction[J]. Korean J Intern Med, 2019, 34(6): 1263-1271. doi: 10.3904/kjim.2018.153
[15] Bryce YC, Perez-Johnston R, Bryce EB, et al. Pathophysiology of right ventricular failure in acute pulmonary embolism and chronic thromboembolic pulmonary hypertension: a pictorial essay for the interventional radiologist[J]. Insights Imaging, 2019, 10(1): 18. doi: 10.1186/s13244-019-0695-9
[16] Giannitsis E, Müller-Bardorff M, Kurowski V, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism[J]. Circulation, 2000, 102(2): 211-217. doi: 10.1161/01.CIR.102.2.211
[17] Ross C, Kumar R, Pelland-Marcotte MC, et al. Acute management of high-risk and intermediate-risk pulmonary embolism in children: a review[J]. Chest, 2022, 161(3): 791-802. doi: 10.1016/j.chest.2021.09.019
[18] Bělohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part Ⅰ: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism[J]. Exp Clin Cardiol, 2013, 18(2): 129-138.
[19] Becattini C, Vedovati MC, Agnelli G. Prognostic value of troponins in acute pulmonary embolism: a meta-analysis[J]. Circulation, 2007, 116(4): 427-433. doi: 10.1161/CIRCULATIONAHA.106.680421
[20] Bikdeli B, Muriel A, Rodríguez C, et al. High-sensitivity vs conventional troponin cutoffs for risk stratification in patients with acute pulmonary embolism[J]. JAMA Cardiol, 2024, 9(1): 64-70. doi: 10.1001/jamacardio.2023.4356
[21] Dubin RF, Li Y, He J, et al. Predictors of high sensitivity cardiac troponin T in chronic kidney disease patients: a cross-sectional study in the chronic renal insufficiency cohort(CRIC)[J]. BMC Nephrol, 2013, 14: 229. doi: 10.1186/1471-2369-14-229
[22] Long B, Belcher CN, Koyfman A, et al. Interpreting troponin in renal disease: a narrative review for emergency clinicians[J]. Am J Emerg Med, 2020, 38(5): 990-997. doi: 10.1016/j.ajem.2019.11.041
[23] Junho CVC, Frisch J, Soppert J, et al. Cardiomyopathy in chronic kidney disease: clinical features, biomarkers and the contribution of murine models in understanding pathophysiology[J]. Clin Kidney J, 2023, 16(11): 1786-1803. doi: 10.1093/ckj/sfad085
[24] Cozzolino M, Galassi A, Pivari F, et al. The cardiovascular burden in end-stage renal disease[J]. Contrib Nephrol, 2017, 191: 44-57.
[25] Khan NA, Hemmelgarn BR, Tonelli M, et al. Prognostic value of troponin T and I among asymptomatic patients with end-stage renal disease: a meta-analysis[J]. Circulation, 2005, 112(20): 3088-3096. doi: 10.1161/CIRCULATIONAHA.105.560128
[26] Michos ED, Wilson LM, Yeh HC, et al. Prognostic value of cardiac troponin in patients with chronic kidney disease without suspected acute coronary syndrome: a systematic review and meta-analysis[J]. Ann Intern Med, 2014, 161(7): 491-501. doi: 10.7326/M14-0743
[27] Apple FS, Murakami MM, Pearce LA, et al. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease[J]. Circulation, 2002, 106(23): 2941-2945. doi: 10.1161/01.CIR.0000041254.30637.34
[28] Laveborn E, Lindmark K, Skagerlind M, et al. NT-proBNP and troponin T levels differ after haemodialysis with a low versus high flux membrane[J]. Int J Artif Organs, 2015, 38(2): 69-75. doi: 10.5301/ijao.5000387
[29] Sommerer C, Heckele S, Schwenger V, et al. Cardiac biomarkers are influenced by dialysis characteristics[J]. Clin Nephrol, 2007, 68(6): 392-400.
[30] Sandoval Y, Herzog CA, Love SA, et al. Prognostic value of serial changes in high-sensitivity cardiac troponin I and T over 3 months using reference change values in hemodialysis patients[J]. Clin Chem, 2016, 62(4): 631-638. doi: 10.1373/clinchem.2015.251835
[31] Scheitz JF, Nolte CH, Doehner W, et al. Stroke-heart syndrome: clinical presentation and underlying mechanisms[J]. Lancet Neurol, 2018, 17(12): 1109-1120. doi: 10.1016/S1474-4422(18)30336-3
[32] Scheitz JF, Stengl H, Nolte CH, et al. Neurological update: use of cardiac troponin in patients with stroke[J]. J Neurol, 2021, 268(6): 2284-2292. doi: 10.1007/s00415-020-10349-w
[33] Scheitz JF, Nolte CH, Laufs U, et al. Application and interpretation of high-sensitivity cardiac troponin assays in patients with acute ischemic stroke[J]. Stroke, 2015, 46(4): 1132-1140. doi: 10.1161/STROKEAHA.114.007858
[34] Osteraas ND, Lee VH. Neurocardiology[J]. Handb Clin Neurol, 2017, 140: 49-65.
[35] Scheitz JF, Mochmann HC, Erdur H, et al. Prognostic relevance of cardiac troponin T levels and their dynamic changes measured with a high-sensitivity assay in acute ischaemic stroke: analyses from the TRELAS cohort[J]. Int J Cardiol, 2014, 177(3): 886-893. doi: 10.1016/j.ijcard.2014.10.036
[36] Esteak T, Hasan M, Atiqur Rahman M, et al. Elevated troponin I as a marker for unfavorable outcomes in acute ischemic stroke[J]. Cureus, 2023, 15(11): e49568.
[37] Hellwig S, Ihl T, Ganeshan R, et al. Cardiac troponin and recurrent major vascular events after minor stroke or transient ischemic attack[J]. Ann Neurol, 2021, 90(6): 901-912. doi: 10.1002/ana.26225
[38] Scheitz JF, Pare G, Pearce LA, et al. High-sensitivity cardiac troponin T for risk stratification in patients with embolic stroke of undetermined source[J]. Stroke, 2020, 51(8): 2386-2394. doi: 10.1161/STROKEAHA.120.029628
[39] Wu AHB. Increased troponin in patients with sepsis and septic shock: myocardial necrosis or reversible myocardial depression?[J]. Intensive Care Med, 2001, 27(6): 959-961. doi: 10.1007/s001340100970
[40] Fernandes CJ Jr, Akamine N, Knobel E. Myocardial depression in sepsis[J]. Shock, 2008, 30(Suppl 1): 14-17.
[41] Røsjø H, Varpula M, Hagve TA, et al. Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome[J]. Intensive Care Med, 2011, 37(1): 77-85. doi: 10.1007/s00134-010-2051-x
[42] Zheng PQ, Wang X, Guo T, et al. Cardiac troponin as a prognosticator of mortality in patients with sepsis: a systematic review and meta-analysis[J]. Immun Inflamm Dis, 2023, 11(9): e1014. doi: 10.1002/iid3.1014
[43] Sheyin O, Davies O, Duan WL, et al. The prognostic significance of troponin elevation in patients with sepsis: a meta-analysis[J]. Heart Lung, 2015, 44(1): 75-81. doi: 10.1016/j.hrtlng.2014.10.002
[44] Xia JD, Hua LW, Kang DW, et al. The association between higher cardiac troponin levels and the development of left ventricular diastolic dysfunction in septic patients with diabetes mellitus[J]. Int J Cardiovasc Imaging, 2024, 40(1): 27-34.
[45] ver Elst KM, Spapen HD, Nguyen DN, et al. Cardiac troponins I and T are biological markers of left ventricular dysfunction in septic shock[J]. Clin Chem, 2000, 46(5): 650-657. doi: 10.1093/clinchem/46.5.650
[46] Hessel MHM, Atsma DE, van der Valk EJM, et al. Release of cardiac troponin I from viable cardiomyocytes is mediated by integrin stimulation[J]. Pflügers Arch Eur J Physiol, 2008, 455(6): 979-986. doi: 10.1007/s00424-007-0354-8
[47] Eijsvogels TM, Fernandez AB, Thompson PD. Are there deleterious cardiac effects of acute and chronic endurance exercise?[J]. Physiol Rev, 2016, 96(1): 99-125. doi: 10.1152/physrev.00029.2014
[48] Aengevaeren VL, Froeling M, Hooijmans MT, et al. Myocardial injury and compromised cardiomyocyte integrity following a marathon Run[J]. JACC Cardiovasc Imaging, 2020, 13(6): 1445-1447. doi: 10.1016/j.jcmg.2019.12.020
[49] Ghekiere O, Herbots L, Peters B, et al. Exercise-induced myocardial T1 increase and right ventricular dysfunction in recreational cyclists: a CMR study[J]. Eur J Appl Physiol, 2023, 123(10): 2107-2117. doi: 10.1007/s00421-023-05259-4ossref.org/guestquery?queryType=xml&restype=unixref&xml=|Appl. Math. Lett.||99||105959|2020|||
[50] Aakre KM, Omland T. Physical activity, exercise and cardiac troponins: Clinical implications[J]. Prog Cardiovasc Dis, 2019, 62(2): 108-115. doi: 10.1016/j.pcad.2019.02.005
[51] Aengevaeren VL, Hopman MTE, Thompson PD, et al. Exercise-induced cardiac troponin I increase and incident mortality and cardiovascular events[J]. Circulation, 2019, 140(10): 804-814. doi: 10.1161/CIRCULATIONAHA.119.041627
[52] Gong FF, Cascino GJ, Murtagh G, et al. Circulating biomarkers for cardiotoxicity risk prediction[J]. Curr Treat Options Oncol, 2021, 22(6): 46. doi: 10.1007/s11864-021-00845-0
[53] McGowan JV, Chung R, Maulik A, et al. Anthracycline chemotherapy and cardiotoxicity[J]. Cardiovasc Drugs Ther, 2017, 31(1): 63-75. doi: 10.1007/s10557-016-6711-0
[54] Touyz RM, Herrmann J. Cardiotoxicity with vascular endothelial growth factor inhibitor therapy[J]. NPJ Precis Oncol, 2018, 2: 13. doi: 10.1038/s41698-018-0056-z
[55] 刘德敏, 路旭阳, 谷国强. 免疫检查点抑制剂致心脏毒性的研究进展[J]. 临床心血管病杂志, 2023, 39(6): 481-486. doi: 10.13201/j.issn.1001-1439.2023.06.014
[56] Cardinale D, Sandri MT, Martinoni A, et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy[J]. J Am Coll Cardiol, 2000, 36(2): 517-522. doi: 10.1016/S0735-1097(00)00748-8
[57] Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy[J]. Circulation, 2004, 109(22): 2749-2754. doi: 10.1161/01.CIR.0000130926.51766.CC
[58] Zardavas D, Suter TM, van Veldhuisen DJ, et al. Role of troponins I and T and N-terminal prohormone of brain natriuretic peptide in monitoring cardiac safety of patients with early-stage human epidermal growth factor receptor 2-positive breast cancer receiving trastuzumab: a herceptin adjuvant study cardiac marker substudy[J]. J Clin Oncol, 2017, 35(8): 878-884. doi: 10.1200/JCO.2015.65.7916
[59] Mahmood SS, Fradley MG, Cohen JV, et al. Myocarditis in patients treated with immune checkpoint inhibitors[J]. J Am Coll Cardiol, 2018, 71(16): 1755-1764. doi: 10.1016/j.jacc.2018.02.037
[60] Xu T, Meng QH, Gilchrist SC, et al. Assessment of prognostic value of high-sensitivity cardiac troponin T for early prediction of chemoradiation therapy-induced cardiotoxicity in patients with non-small cell lung cancer: a secondary analysis of a prospective randomized trial[J]. Int J Radiat Oncol, 2021, 111(4): 907-916. doi: 10.1016/j.ijrobp.2021.07.035
[61] Mir A, Badi Y, Bugazia S, et al. Efficacy and safety of cardioprotective drugs in chemotherapy-induced cardiotoxicity: an updated systematic review & network meta-analysis[J]. Cardiooncology, 2023, 9(1): 10.
-




 下载:
下载: