The predictive effect of systemic inflammatory index on adverse cardiovascular events in stable angina pectoris patients with hemodynamic disturbances
-
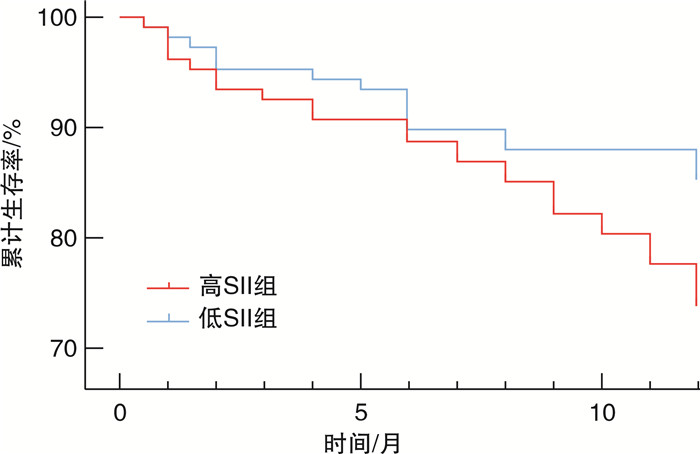
摘要: 目的 探究系统免疫炎症指数(SII)对血流动力学紊乱的稳定型心绞痛患者主要不良心血管事件(MACE)的预测作用。方法 连续入选2018年6月—2020年12月因稳定型心绞痛就诊于新疆医科大学第一附属医院心脏中心行血流储备分数(FFR)检查的215例患者,收集患者临床信息及入院检查结果,根据血常规检查计算SII。根据随访期间是否发生MACE,将患者分为MACE组(44例)和非MACE组(171例)。根据SII中位数(434),将患者分为低SII组(108例)和高SII组(107例)。采用Cox回归分析评估SII对血流动力学紊乱的稳定型心绞痛患者预后的影响。采用Kaplan-Meier法绘制生存曲线,运用log-rank检验比较不同SII水平患者的生存率。结果 与非MACE组比较,MACE组患者SII水平显著升高[393.66(286.42,602.08) vs 473.80(301.40,941.98),P=0.037]。多因素Cox回归分析显示,SII与血流紊乱稳定型心绞痛患者MACE独立相关(HR=1.001,95%CI:1.000~1.002,P=0.002)。Kaplan-Meier生存分析表明,高SII组患者生存率明显降低(P=0.04)。结论 SII是血流动力学紊乱的稳定型心绞痛患者MACE的独立预测因子。Abstract: Objective To explore the predictive effect of systemic immune inflammatory index(SII) on major adverse cardiovascular events(MACE) in stable angina pectoris patients with hemodynamic disturbances.Methods A total of 215 patients who underwent fractional flow reserve(FFR) examination due to stable angina pectoris at the Heart Center of the First Affiliated Hospital of Xinjiang Medical University from June 2018 to December 2020 were selected consecutively. Clinical information and admission examination results were collected, and SII was calculated based on blood routine examination. Patients were divided into the MACE group(n=44) and non-MACE group(n=171) according to whether MACE occurred during the follow-up period. According to the median SII(434), patients were divided into the low-SII group(n=108) and high-SII group(n=107). Cox regression analysis was used to evaluate the effect of SII on the prognosis of stable angina patients with hemodynamic disturbances. Kaplan Meier method was used to plot survival curves, and log-rank analysis was used to compare the differences in the survival rate among patients with different SII levels.Results Compared with the non-MACE group, patients in the MACE group had significantly higher levels of SII[393.66(286.42, 602.08) vs 473.80(301.40, 941.98), P=0.037]. Multivariate Cox regression analysis showed that SII was independently associated with MACE in stable angina pectoris patients with hemodynamic disturbances(HR=1.001, 95%CI: 1.000-1.002, P=0.002). Kaplan-Meier survival analysis showed that the high-SII group had significantly lower survival rate(P=0.04).Conclusion SII is an independent predictor of MACE in stable angina pectoris patients with hemodynamic disturbances.
-

-
表 1 非MACE组和MACE组基线特征比较
Table 1. Comparison of baseline characteristics between the MACE and non-MACE groups
例(%), X ± S, M(P25, P75) 项目 非MACE组(171例) MACE组(44例) P 年龄/岁 59±9 59±10 0.955 男性 132(77.2) 34(77.3) 0.991 吸烟 99(57.9) 24(54.5) 0.689 糖尿病 45(26.3) 13(25.9) 0.667 高血压 115(67.3) 28(63.6) 0.650 PCI史 47(27.5) 14(31.8) 0.570 LVEF/% 62±5 62±4 0.564 血红蛋白/(g/L) 142.63±13.38 147.00±13.62 0.015 尿酸/(μmol/L) 333.40±90.58 329.26±90.70 0.781 白蛋白/(g/L) 41.60±3.90 42.70±5.14 0.110 BMI/(kg/m2) 26.55±3.32 25.18±3.51 0.013 血小板/(×109/L) 220.95±50.41 227.10±58.14 0.473 血糖/(mmol/L) 5.28(4.65,6.61) 5.38(4.42,6.93) 0.985 白细胞/(×109/L) 6.72(5.75,8.11) 6.68(5.87,8.02) 0.641 甘油三酯/(mmol/L) 1.60(1.10,2.40) 1.43(0.89,2.01) 0.072 TC/(mmol/L) 3.45(2.85,4.29) 2.98(2.59,3.51) 0.012 HDL-C/(mmol/L) 0.99(0.84,1.18) 0.95(0.81,1.14) 0.206 LDL-C/(mmol/L) 1.98(1.63,2.74) 1.79(1.44,2.24) 0.030 中性粒细胞/(×109/L) 3.81(2.99,4.98) 4.07(3.39,5.67) 0.126 淋巴细胞/(×109/L) 1.99(1.59,2.52) 1.75(1.41,2.21) 0.053 Gensini评分 16(12,25) 12(16,24) 0.671 FFR/% 0.74±0.06 0.72±0.05 0.257 SII 393.66(286.42,602.08) 473.80(301.40,941.98) 0.037 表 2 低SII组和高SII组基线特征比较
Table 2. Comparison of baseline characteristics between the low and high SII groups
例(%), X ± S, M(P25, P75) 项目 低SII组(108例) 高SII组(107例) P 年龄/岁 59±10 59±10 0.969 男性 80(74.1) 86(80.4) 0.271 吸烟 58(53.7) 65(60.7) 0.297 糖尿病 27(25.0) 31(29.0) 0.512 高血压 64(59.3) 79(73.8) 0.024 PCI史 58(53.7) 54(50.5) 0.635 LVEF/% 62±4 62±5 0.446 血红蛋白/(g/L) 142.28±13.44 144.62±13.83 0.202 尿酸/(μmol/L) 337.53±92.05 328.49±88.71 0.541 白蛋白/(g/L) 41.99±4.71 41.61±3.69 0.886 BMI/(kg/m2) 26.17±3.32 26.31±3.50 0.590 血小板/(×109/L) 201.63±40.99 243.12±54.75 < 0.001 血糖/(mmol/L) 5.11(4.55,6.60) 5.41(4.68,6.61) 0.282 白细胞/(×109/L) 6.21(5.48,7.28) 7.58(6.08,8.76) < 0.001 甘油三酯/(mmol/L) 1.52(1.01,2.20) 1.57(1.11,2.24) 0.539 TC/(mmol/L) 3.22(2.66,4.32) 3.37(2.86,4.04) 0.518 HDL-C/(mmol/L) 1.00(0.85,1.19) 0.96(0.82,1.16) 0.212 LDL-C/(mmol/L) 1.19(1.49,2.72) 1.98(1.63,2.49) 0.628 中性粒细胞/(×109/L) 3.28(2.70,3.85) 4.99(4.02,6.21) < 0.001 淋巴细胞/(×109/L) 2.19(1.86,2.69) 1.73(1.33,2.09) < 0.001 Gensini评分 16(11,24) 16(12,23) 0.667 FFR/% 73±6 74±6 0.661 SII 296.31(240.92,345.80) 652.97(516.75,940.01) < 0.001 表 3 单因素及多因素Cox回归分析
Table 3. Univariate and multivariate Cox regression analysis
变量 单因素 多因素 HR(95%CI) P HR(95%CI) P BMI 0.881(0.800~0.971) 0.010 0.910(0.825~1.004) 0.059 甘油三酯 0.741(0.539~1.020) 0.066 LDL-C 0.664(0.444~0.994) 0.047 0.639(0.418~0.978 0.039 FFR 0.081(0.001~6.832) 0.267 SII 1.003(1.002~1.006) 0.001 1.001(1.000~1.002) 0.002 -
[1] Kumar A. Hemodynamically complicated ST-segment elevation myocardial infarction: presentation and treatment[J]. Future Cardiol, 2010, 6(5): 591-602. doi: 10.2217/fca.10.83
[2] Malota Z, Glowacki J, Sadowski W, et al. Numerical analysis of the impact of flow rate, heart rate, vessel geometry, and degree of stenosis on coronary hemodynamic indices[J]. BMC Cardiovasc Disord, 2018, 18(1): 132. doi: 10.1186/s12872-018-0865-6
[3] Joshi PH, de Lemos JA. Diagnosis and Management of Stable Angina: A Review[J]. JAMA, 2021, 325(17): 1765-1778. doi: 10.1001/jama.2021.1527
[4] Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation[J]. J Am Coll Cardiol, 2010, 55(25): 2816-2821. doi: 10.1016/j.jacc.2009.11.096
[5] Berry C, Layland J, Sood A, et al. Fractional flow reserve versus angiography in guiding management to optimize outcomes in non-ST-elevation myocardial infarction(FAMOUS-NSTEMI): rationale and design of a randomized controlled clinical trial[J]. Am Heart J, 2013, 166(4): 662-668. e3. doi: 10.1016/j.ahj.2013.07.011
[6] Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes[J]. Eur Heart J, 2020, 41(3): 407-477. doi: 10.1093/eurheartj/ehz425
[7] Incalcaterra E, Accardi G, Balistreri CR, et al. Pro-inflammatory genetic markers of atherosclerosis[J]. Curr Atheroscler Rep, 2013, 15(6): 329. doi: 10.1007/s11883-013-0329-5
[8] Li Q, Ma X, Shao Q, et al. Prognostic Impact of Multiple Lymphocyte-Based Inflammatory Indices in Acute Coronary Syndrome Patients[J]. Front Cardiovasc Med, 2022, 9: 811790. doi: 10.3389/fcvm.2022.811790
[9] Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index(SⅡ)predicted clinical outcome in patients with coronary artery disease[J]. Eur J Clin Invest, 2020, 50(5): e13230. doi: 10.1111/eci.13230
[10] Akyel A, Yayla Ç, Erat M, et al. Neutrophil-to-lymphocyte ratio predicts hemodynamic significance of coronary artery stenosis[J]. Anatol J Cardiol, 2015, 15(12): 1002-1007. doi: 10.5152/akd.2015.5909
[11] Hotamisligil GS. Inflammation and metabolic disorders[J]. Nature, 2006, 444(7121): 860-867. doi: 10.1038/nature05485
[12] Saylik F, Akbulut T. Systemic Immune-Inflammation Index Predicts Major Cardiovascular Adverse Events in Patients with ST-Segment Elevated Myocardial Infarction[J]. Arq Bras Cardiol, 2022, 119(1): 14-22.
[13] 马媛, 董蕴, 汪京嘉, 等. 系统性免疫炎症指数与2型糖尿病患者异常心电图的相关性及其预测价值[J]. 临床心血管病杂志, 2023, 39(11): 850-854. doi: 10.13201/j.issn.1001-1439.2023.11.007
[14] 高蓉蓉, 徐芳, 祝绪, 等. 全血细胞衍生的炎症标志物对急性心力衰竭患者的长期预后价值[J]. 临床心血管病杂志, 2022, 38(12): 980-987. doi: 10.13201/j.issn.1001-1439.2022.12.010
[15] Naidu SS, Rao SV, Blankenship J, et al. Clinical expert consensus statement on best practices in the cardiac catheterization laboratory: Society for Cardiovascular Angiography and Interventions[J]. Catheter Cardiovasc Interv, 2012, 80(3): 456-464. doi: 10.1002/ccd.24311
[16] Li X, Yu C, Liu X, et al. A Prediction Model Based on Systemic Immune-Inflammatory Index Combined with Other Predictors for Major Adverse Cardiovascular Events in Acute Myocardial Infarction Patients[J]. J Inflamm Res, 2024, 17: 1211-1225. doi: 10.2147/JIR.S443153
[17] Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond[J]. J Am Coll Cardiol, 2019, 74(20): 2529-2532. doi: 10.1016/j.jacc.2019.10.009
[18] Prabhakaran D, Jeemon P, Roy A. Cardiovascular Diseases in India: Current Epidemiology and Future Directions[J]. Circulation, 2016, 133(16): 1605-1620. doi: 10.1161/CIRCULATIONAHA.114.008729
[19] Wasilewski J, Mirota K, Hawranek M, et al. Invasive and non-invasive fractional flow reserve index in validation of hemodynamic severity of intracoronary lesions[J]. Postepy Kardiol Interwencyjnej, 2013, 9(2): 160-169.
[20] Kochar M, Min JK. Physiologic assessment of coronary artery disease by cardiac computed tomography[J]. Korean Circ J, 2013, 43(7): 435-442. doi: 10.4070/kcj.2013.43.7.435
[21] Vogel RA. Assessing stenosis significance by coronary arteriography: are the best variables good enough[J]. J Am Coll Cardiol, 1988, 12(3): 692-693. doi: 10.1016/S0735-1097(88)80058-5
[22] Hoole SP, Bambrough P. Recent advances in percutaneous coronary intervention[J]. Heart, 2020, 106(18): 1380-1386. doi: 10.1136/heartjnl-2019-315707
[23] Jeremias A, Davies JE, Maehara A, et al. Blinded Physiological Assessment of Residual Ischemia After Successful Angiographic Percutaneous Coronary Intervention: The DEFINE PCI Study[J]. JACC Cardiovasc Interv, 2019, 12(20): 1991-2001. doi: 10.1016/j.jcin.2019.05.054
[24] Biswas S, Dinh D, Lucas M, et al. Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention[J]. J Clin Med, 2020, 9(10): E3242. doi: 10.3390/jcm9103242
[25] Libby P. Current concepts of the pathogenesis of the acute coronary syndromes[J]. Circulation, 2001, 104(3): 365-372. doi: 10.1161/01.CIR.104.3.365
[26] Hamirani YS, Katz R, Nasir K, et al. Association between inflammatory markers and liver fat: The Multi-Ethnic Study of Atherosclerosis[J]. J Clin Exp Cardiol, 2014, 5: 1000344.
[27] Massberg S, Brand K, Grüner S, et al. A critical role of platelet adhesion in the initiation of atherosclerotic lesion formation[J]. J Exp Med, 2002, 196(7): 887-896. doi: 10.1084/jem.20012044
[28] Pfeiler S, Stark K, Massberg S, et al. Propagation of thrombosis by neutrophils and extracellular nucleosome networks[J]. Haematologica, 2017, 102(2): 206-213. doi: 10.3324/haematol.2016.142471
[29] Candemir M, Kiziltunç E, Nurkoç S, et al. Relationship Between Systemic Immune-Inflammation Index(SⅡ)and the Severity of Stable Coronary Artery Disease[J]. Angiology, 2021, 72(6): 575-581. doi: 10.1177/0003319720987743
[30] Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma[J]. Clin Cancer Res, 2014, 20(23): 6212-6222. doi: 10.1158/1078-0432.CCR-14-0442
[31] Ridker PM, Bhatt DL, Pradhan AD, et al. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials[J]. Lancet, 2023, 401(10384): 1293-1301. doi: 10.1016/S0140-6736(23)00215-5
[32] Gori E, Pierini A, Pasquini A, et al. The erythrocyte sedimentation rate(ESR)in canine inflammation[J]. Vet J, 2023, 294: 105949. doi: 10.1016/j.tvjl.2022.105949
-




 下载:
下载: