Causes of early paraplegia following Sun's procedure in patients with stanford type A aortic dissection
-
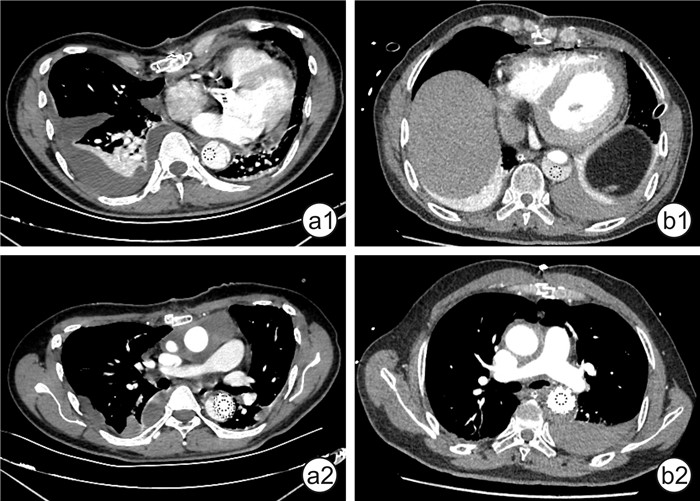
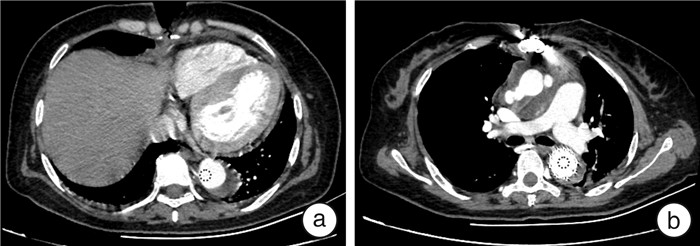
摘要: 目的 回顾性分析Stanford A型主动脉夹层患者接受孙氏手术后出现早期截瘫的围术期危险因素。方法 收集2021年1月—12月因Stanford A型主动脉夹层收治于华中科技大学同济医学院附属同济医院心脏大血管外科并行孙氏手术的178例患者的临床资料,其中男性140例、女性38例,平均年龄为(51.5±10.7)岁,术后截瘫患者7例(3.9%)。统计分析截瘫组与非截瘫组患者围术期临床数据。测量并记录患者术后CTA影像肋间动脉开口位置以及开放程度,探究术后截瘫的原因以及危险因素。结果 非截瘫组和截瘫组患者性别、身高、体重、心血管病史、主动脉阻断时间、中低温停循环时间以及肛温差异均无统计学意义。两组患者术前低血压事件与年龄均差异有统计学意义(均P < 0.05),截瘫组患者CTA影像Th7~Th11肋间动脉的起始处与肺动脉分叉水平主动脉CT值比值(Hounsfield ratio,HUR)显著低于非截瘫组患者(P < 0.05)。多因素logistic回归分析提示,术前低血压事件(OR=33.80,P < 0.05)、支架覆盖的肋间动脉数量≥8支(OR=35.00,P < 0.05)与假腔供血肋间动脉数量≥10支(OR=36.71,P < 0.05)均增加术后截瘫风险。结论 Stanford A型主动脉夹层术前低血压事件、支架覆盖肋间动脉≥8支和假腔供血肋间动脉≥10支是术后截瘫的危险因素;HUR有望对残余肋间动脉供血状况进行评估,有一定的临床指导价值。
-
关键词:
- Stanford A型主动脉夹层 /
- 截瘫 /
- 脊髓缺血 /
- 亨氏单位比值
Abstract: Objective To retrospectively analyse perioperative risk factors of early paraplegia in patients with Stanford type A aortic dissection undergoing Sun's procedure.Methods All patients who underwent Sun's procedure from January to December 2021 in Tongji Hospital were retrospectively analysed. There were 178 patients with 140 males and 38 females at a mean age of (51.5±10.7) years, and 7 patients(3.9%) of them developed postoperative paraplegia. We performed a statistical analysis of perioperative clinical data between the paraplegia and non-paraplegia groups. The locations of the Th7-Th12 intercostal arteries'origin and blood supply were also recorded to investigate the cause of early paraplegia.Results Among the 178 patients, there were no statistical differences in gender, height, weight, history, aortic crossclamping time, moderate hypothermic circulatory arrest time(antegrade cerebral perfusion) and anal temperature between the paraplegia group and non-paraplegia group. Preoperative hypotension events and age had statistically significant differences between the two groups(both P < 0.05). Hounsfield ratio(HUR) from Th7 to Th11 showed statistical differences between the two groups(P < 0.05). Logistic regression analysis suggested that preoperative hypotension(OR=33.80, P < 0.05), the number of stent-covered intercostal arteries ≥8(OR=35.00, P < 0.05), and the number of intercostal arteries from false lumen ≥10(OR=36.71, P < 0.05) increased the risk of postoperative paraplegia.Conclusion Preoperative hypotension, covered intercostal artery ≥8, and intercostal arteries from false lumen ≥10 may be risk factors for postoperative paraplegia in Stanford type A aortic dissection. HUR has a certain guiding significance in evaluating the blood supply of the residual intercostal artery.-
Key words:
- Stanford type A aortic dissection /
- paraplegia /
- spinal cord ischemia /
- Hounsfield ratio
-

-
表 1 非截瘫组和截瘫组患者术前临床资料比较
Table 1. Preoperative clinical data
例(%), X ± S, M(P25, P75) 项目 非截瘫组(171例) 截瘫组(7例) P 年龄 51.81±10.50 42.71±12.11 0.027 男性 133(77.8) 7(100.0) 0.350 身高/cm 170.00(165.00,175.00) 169.50(167.25,170.00) 0.649 体重/kg 74.00(65.00,80.00) 80.00(72.50,90.00) 0.211 高血压 118(69.0) 3(42.9) 0.300 糖尿病 5(2.9) 1(14.3) 0.220 高血脂 29(17.0) 1(14.3) 1.000 冠心病 6(3.5) 0 1.000 吸烟 66(38.6) 3(42.9) 1.000 既往卒中/TIA 7(4.1) 1(14.3) 0.280 术前检验 肾小球滤过率/(mL/min) 83.93±22.69 76.77±38.88 0.645 肌酐/(μmol/L) 85.00(70.00,105.00) 137.00(66.00,153.00) 0.205 血红蛋白/(g/L) 132.00(122.00,143.00) 139.00(130.00,143.00) 0.257 术前不良事件 心力衰竭 71(41.5) 3(42.9) 1.000 下肢灌注不良 13(7.6) 1(14.3) 0.420 低血压/休克 2(1.2) 2(28.6) 0.008 TIA:短暂性脑缺血发作。 表 2 非截瘫组和截瘫组患者术中临床资料比较
Table 2. Surgical data
例(%), X ± S, M(P25, P75) 项目 非截瘫组(171例) 截瘫组(7例) P 更换主动脉瓣膜 54(31.6) 3(42.9) 0.830 CABG 9(5.3) 0 1.000 股动脉插管 120(70.2) 4(57.1) 0.751 CPB时间/min 241.00(210.00,294.00) 274.00(227.00,336.00) 0.197 主动脉阻断时间/min 120.00(101.00,143.50) 117.00(98.00,140.00) 0.988 停循环时间/min 25.35±13.71 22.43±13.50 0.581 肛温/℃ 25.0(24.0,26.0) 21.0(12.0,35.0) 0.734 术中输血 红细胞/U 4.5(0.0,8.0) 8.0(4.0,8.0) 0.197 血浆/mL 800.0(525.0,1 000.0) 900.00(700.0,1 300.0) 0.368 血小板/U 3.0(3.0,3.0) 3.0(3.0,3.0) 0.891 表 3 非截瘫组和截瘫组患者术后资料比较
Table 3. Postoperative clinical data
例(%), M(P25, P75) 项目 非截瘫组(171例) 截瘫组(7例) P 术后出血 10(5.8) 2(28.6) 0.070 恶性心律失常 14(8.2) 1(14.3) 0.471 肺部感染 36(21.1) 3(42.9) 0.368 脑卒中 19(11.1) 1(14.3) 0.571 肾功能不全 73(42.9) 5(71.4) 0.271 术后3 d内低血压/休克 6(3.5) 1(14.3) 0.251 重症监护时间/d 8(5,14) 22(14,30) 0.001 再次通气 49(28.7) 6(85.7) 0.004 住院天数/d 21(15,28) 32(23,38) 0.030 表 4 非截瘫组和截瘫组患者多因素logistic回归分析
Table 4. Multivariable logistic regression analysis
变量 OR 95%CI P 年龄 0.88 0.801~0.972 0.011 术前休克/严重低血压 33.80 3.928~290.842 0.003 阻断时间 1.00 0.968~1.024 0.768 停循环时间 0.98 0.911~1.060 0.651 肛温 0.90 0.581~1.400 0.645 术后3 d内低血压 0.10 0.001~6.865 0.277 表 5 非截瘫组和截瘫组患者CTA资料比较
Table 5. CT angiography data
M(P25, P75) 变量 非截瘫组(82例) 截瘫组(7例) P 支架末端锚定位置(椎体) 7(6,7) 7(7,8) 0.150 血栓形成范围(椎体) 9(8,11) 10(8,11) 0.720 假腔供血的肋间动脉数量 4(2,8) 10(6,12) 0.090 支架覆盖肋间动脉数量 6(6,8) 8(8,10) 0.020 表 6 CTA影像资料logistic回归分析
Table 6. Logistic regression analysis of CTA data
变量 OR 95%CI P 血栓形成范围超过2个椎体 0.78 0.094~6.407 0.813 假腔供血肋间动脉≥10支 36.71 4.177~322.568 0.001 支架覆盖肋间动脉≥8支 35.00 2.189~558.985 0.012 表 7 非截瘫组和截瘫组患者术后HUR的资料比较
Table 7. Comparison of HUR
M(P25, P75) 变量 非截瘫组(82例) 截瘫组(7例) P Th7左侧 0.92(0.69,0.99) 0.50(0.35,0.60) 0.002 Th7右侧 0.95(0.89,0.99) 0.57(0.36,0.90) 0.002 Th8左侧 0.90(0.72,0.95) 0.44(0.26,0.49) 0.001 Th8右侧 0.92(0.88,0.97) 0.49(0.40,0.66) 0.001 Th9左侧 0.95(0.79,1.00) 0.51(0.37,0.55) 0.001 Th9右侧 0.94(0.82,0.99) 0.51(0.37,0.55) 0.001 Th10左侧 0.93(0.76,0.99) 0.45(0.42,0.60) 0.001 Th10右侧 0.94(0.86,1.01) 0.49(0.44,0.60) 0.001 Th11左侧 0.94(0.75,0.99) 0.55(0.50,0.76) 0.002 Th11右侧 0.95(0.84,1.00) 0.71(0.54,0.89) 0.015 Th12左侧 0.90(0.76,0.98) 0.81(0.65,0.88) 0.161 Th12右侧 0.90(0.80,0.98) 0.85(0.76,0.98) 0.293 -
[1] LeMaire SA, Russell L. Epidemiology of thoracic aortic dissection[J]. Nat Rev Cardiol, 2011, 8: 103-113. doi: 10.1038/nrcardio.2010.187
[2] Mészáros I, Mórocz J, Szlávi J, et al. Epidemiology and clinicopathology of aortic dissection[J]. Chest, 2000, 117(5): 1271-1278. doi: 10.1378/chest.117.5.1271
[3] Ma WG, Zhu JM, Zheng J, et al. Sun's procedure for complex aortic arch repair: total arch replacement using a tetrafurcate graft with stented elephant trunk implantation[J]. Ann Cardiothorac Surg, 2013, 2(5): 642-648.
[4] Shrestha M, Kaufeld T, Beckmann E, et al. Total aortic arch replacement with a novel 4-branched frozen elephant trunk prosthesis: Single-center results of the first 100 patients[J]. J Thorac Cardiovasc Surg, 2016, 152(1): 148-159. e1. doi: 10.1016/j.jtcvs.2016.02.077
[5] Dohle DS, Tsagakis K, Janosi RA, et al. Aortic remodelling in aortic dissection after frozen elephant trunk[J]. Eur J Cardiothorac Surg, 2016, 49(1): 111-117. doi: 10.1093/ejcts/ezv045
[6] Celmeta B, Harky A, Miceli A. Editorial: Frozen elephant trunk surgery in aortic dissection[J]. Front Cardiovasc Med, 2023, 10: 1154375. doi: 10.3389/fcvm.2023.1154375
[7] Chakos A, Jbara D, Yan TD, et al. Long-term survival and related outcomes for hybrid versus traditional arch repair-a meta-analysis[J]. Ann Cardiothorac Surg, 2018, 7(3): 319-327. doi: 10.21037/acs.2018.05.07
[8] Sun LZ, Qi RD, Chang Q, et al. Surgery for acute type A dissection using total arch replacement combined with stented elephant trunk implantation: experience with 107 patients[J]. J Thorac Cardiovasc Surg, 2009, 138(6): 1358-1362. doi: 10.1016/j.jtcvs.2009.04.017
[9] Sun LZ, Qi RD, Zhu JM, et al. Repair of acute type A dissection: our experiences and results[J]. Ann Thorac Surg, 2011, 91(4): 1147-1152. doi: 10.1016/j.athoracsur.2010.12.005
[10] Li J, Zhao CY, Li BH, et al. Aortic root reinforcement combined with vascular grafts eversion and built-in procedure(XJ-procedure)for acute type A aortic dissection surgery[J]. Adv Ther, 2023, 40(12): 5354-5365. doi: 10.1007/s12325-023-02655-2
[11] 余明寰, 刘志刚, 刘晓程. 中/浅低温停循环在主动脉手术中的应用进展[J]. 临床心血管病杂志, 2022, 38(9): 699-705. doi: 10.13201/j.issn.1001-1439.2022.09.004
[12] 唐婷婷, 廖玉华. 2023 ESC急性和慢性心力衰竭诊断和治疗指南更新要点解读[J]. 临床心血管病杂志, 2023, 39(10): 749-752. doi: 10.13201/j.issn.1001-1439.2023.10.003
[13] Katayama K, Uchida N, Katayama A, et al. Multiple factors predict the risk of spinal cord injury after the frozen elephant trunk technique for extended thoracic aortic disease[J]. Eur J Cardiothorac Surg, 2015, 47(4): 616-620. doi: 10.1093/ejcts/ezu243
[14] Tan L, Xiao J, Zhou XM, et al. Untreated distal intimal tears may be associated with paraplegia after total arch replacement and frozen elephant trunk treatment of acute Stanford type A aortic dissection[J]. J Thorac Cardiovasc Surg, 2019, 158(2): 343-350. e1. doi: 10.1016/j.jtcvs.2018.08.111
[15] Afifi RO, Sandhu HK, Zaidi ST, et al. Intercostal artery management in thoracoabdominal aortic surgery: To reattach or not to reattach?[J]. J Thorac Cardiovasc Surg, 2018, 155(4): 1372-1378. e1. doi: 10.1016/j.jtcvs.2017.11.072
[16] Spanos K, Kölbel T, Kubitz JC, et al. Risk of spinal cord ischemia after fenestrated or branched endovascular repair of complex aortic aneurysms[J]. J Vasc Surg, 2019, 69(2): 357-366. doi: 10.1016/j.jvs.2018.05.216
[17] Svensson LG. Commentary: Three reasons for paralysis after elephant trunk procedures[J]. J Thorac Cardiovasc Surg, 2019, 158(2): 351-352. doi: 10.1016/j.jtcvs.2019.05.017
[18] Cuellar FL, Oberhuber A, Martens S, et al. Analysis of spinal ischemia after frozen elephant trunk for acute aortic dissection: an observational, single-center study[J]. Diagnostics(Basel), 2022, 12(11): 2781.
[19] Preventza O, Liao JL, Olive JK, et al. Neurologic complications after the frozen elephant trunk procedure: a meta-analysis of more than 3000 patients[J]. J Thorac Cardiovasc Surg, 2020, 160(1): 20-33. e4. doi: 10.1016/j.jtcvs.2019.10.031
[20] 周宏艳, 王冀, 袁素, 等. 规范化综合性脊髓保护措施能够降低主动脉手术患者围手术期脊髓损伤发生率: 8年回顾性分析[J]. 中华危重病急救医学, 2019, 31(5): 633-636.
[21] Hur J, Kim YJ, Lee HJ, et al. Left atrial appendage thrombi in stroke patients: detection with two-phase cardiac CT angiography versus transesophageal echocardiography[J]. Radiology, 2009, 251(3): 683-690. doi: 10.1148/radiol.2513090794
[22] DeCarlo C, Feldman Z, Sumpio B, et al. Differences in aortic intramural hematoma contrast attenuation on multi-phase CTA predict long-term aortic morphologic change[J]. Ann Vasc Surg, 2022, 87: 87-94. doi: 10.1016/j.avsg.2022.05.012
[23] Banno H, Kawai Y, Sato T, et al. Low-density vulnerable thrombus/plaque volume on preoperative computed tomography predicts for spinal cord ischemia after endovascular repair for thoracic aortic aneurysm[J]. J Vasc Surg, 2021, 73(5): 1557-1565. e1. doi: 10.1016/j.jvs.2020.09.026
-




 下载:
下载: