The correlation between serum CTRP5 level and the degree of coronary artery lesion and myocardial fibrosis in patients with acute coronary syndrome
-
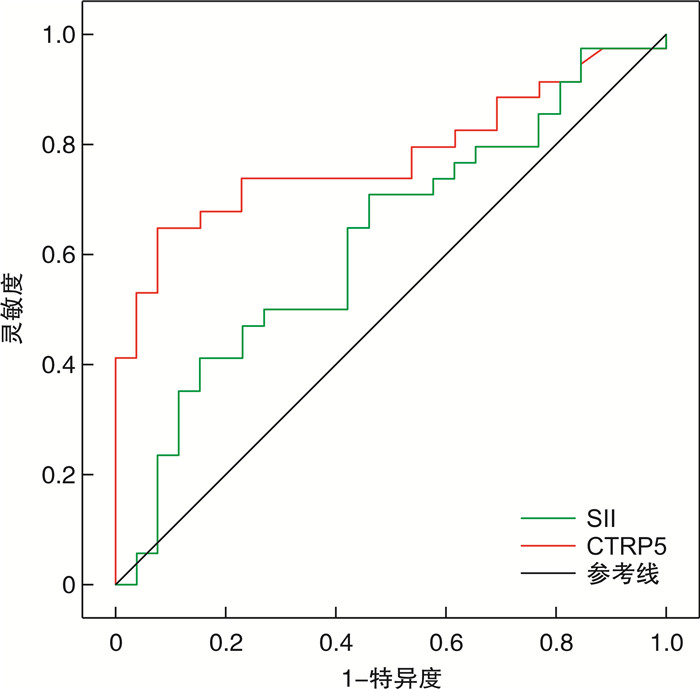
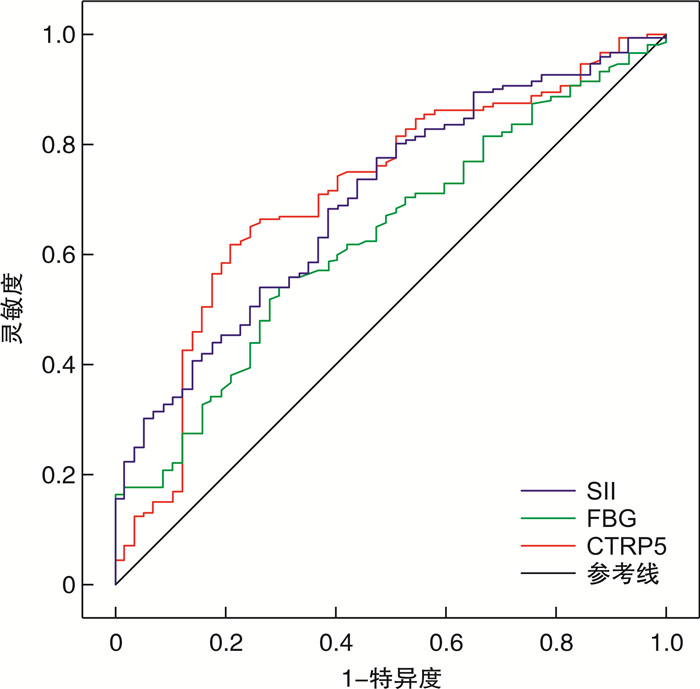
摘要: 目的 检测急性冠脉综合征(ACS)患者血清补体C1q/肿瘤坏死因子相关蛋白-5(CTRP5)水平,并分析其与冠状动脉病变程度和心肌纤维化的关系。方法 选择2022年10月—2023年10月在衡水市人民医院心血管内科住院的ACS患者210例,根据临床诊断标准分为不稳定型心绞痛(UA)亚组、非ST段抬高型心肌梗死(NSTEMI)亚组和ST段抬高型心肌梗死(STEMI)亚组;根据冠状动脉造影血管病变支数分为单支病变亚组、双支病变亚组和3支病变亚组;根据Gensini评分分为高评分亚组(>60分)、中评分亚组(31~60分)和低评分亚组(0~30分)。其中的60例ACS患者术后1个月行心脏磁共振检查,根据心血管磁共振-延迟钆增强(CMR-LGE)分为LGE阳性组和LGE阴性组。另选择同期行冠状动脉造影无明显阻塞性狭窄病变的100例患者作为对照组。比较各组全身免疫炎症指数(SII)和血清CTRP5水平。采用logistic回归分析影响冠状动脉病变程度的因素。绘制受试者工作特征(ROC)曲线,分析血清CTRP5水平对冠状动脉病变程度与心肌纤维化的预测价值。结果 与对照组患者比较,UA亚组、NSTEMI亚组和STEMI亚组患者血清CTRP5和SII水平明显升高(均P < 0.05),但NSTEMI亚组与STEMI亚组上述指标差异无统计学意义。随着冠状动脉病变支数和Gensini评分的增加,CTRP5与SII水平呈升高趋势(均P < 0.05)。LGE阳性组患者入院后CTRP5与SII水平均高于LGE阴性组(均P < 0.05)。Logistic回归分析显示,空腹血糖(FBG,OR=1.267,95%CI:1.041~1.544,P=0.019)、SII(OR=1.001,95%CI:1.000~1002,P=0.044)和CTRP5(OR=1.127,95%CI:1.036~1.226,P=0.005)是冠状动脉多支病变的危险因素。ROC曲线显示,血清CTRP5预测冠状动脉多支病变的曲线下面积(AUC)为0.708,灵敏度为81.4%,特异度为78.9%,截断值为10.31 ng/mL;预测心肌纤维化的AUC为0.775,灵敏度为64.7%,特异度为92.3%,截断值为11.10 ng/mL。结论 ACS患者血清CTRP5水平升高,其水平对冠状动脉病变程度尤其是多支病变及心肌纤维化均具有较好的预测价值。
-
关键词:
- 急性冠脉综合征 /
- 补体C1q/肿瘤坏死因子相关蛋白-5 /
- 冠状动脉病变 /
- 心肌纤维化 /
- Gensini评分
Abstract: Objective To analyze the relationship between serum complement C1q/tumor necrosis factor-related protein 5(CTRP5) level and the severity of coronary artery disease and myocardial fibrosis in patients with acute coronary syndrome(ACS).Methods A total of 210 patients with ACS hospitalized in the Department of Cardiology, Hengshui People's Hospital from October 2022 to October 2023 were selected. All patients were divided into the unstable angina pectoris(UA) subgroup, the non ST-segment elevation myocardial infarction(NSTEMI) subgroup, and the ST-segment elevation myocardial infarction(STEMI) subgroup according to clinical diagnostic criteria. Patients were divided into the single-vessel disease subgroup, double-vessel disease subgroup, and three-vessel disease subgroup based on the number of coronary artery lesions. Patients were divided into the high-score subgroup(>60 points), middle-score subgroup(31-60 points), and low-score subgroup(0-30 points) according to gensini score. Sixty ACS patients underwent cardiac magnetic resonance examination one month after operation, and were divided into the LGE positive group and LGE negative group according to cardiovascular magnetic resonance-delayed gadolinium enhancement(CMR-LGE). Another 100 patients without obvious obstructive stenosis by coronary angiography were selected as the control group. The systemic immune inflammation index(SII) and serum CTRP5 levels were compared among the groups. Logistic regression analysis was used to analyze the factors affecting the degree of coronary artery disease. The receiver operating characteristic(ROC) curve was drawn to analyze the predictive value of serum CTRP5 on the degree of coronary artery disease and myocardial fibrosis.Results The levels of serum CTRP5 and SII in the UA subgroup, NSTEMI subgroup, and STEMI group were higher than those in the control group(all P < 0.05), but there was no significant difference in CTRP5 and SII levels between the NSTEMI subgroup and the STEMI subgroup. With the increase of coronary artery lesions and Gensini score, CTRP5 and SII levels showed an increasing trend(both P < 0.05). CTRP5 and SII levels in the LGE positive group were higher than those in the LGE negative group(both P < 0.05). Logistic regression analysis showed that fasting blood glucose(FBG, OR=1.267, 95%CI: 1.041-1.544, P=0.019), SII(OR=1.001, 95%CI: 1.000-1002, P=0.044), and CTRP5(OR=1.127, 95%CI: 1.036-1.226, P=0.005) were risk factors affecting the severity of coronary artery disease. ROC analysis showed that the area under the curve(AUC) of CTRP5 in predicting multi-vessel disease was 0.708, the sensitivity was 81.4%, the specificity was 78.9%, and the cut-off value was 10.31 ng/mL. The AUC of CTRP5 in predicting myocardial fibrosis was 0.775, the sensitivity was 64.7%, the specificity was 92.3%, and the cut-off value was 11.10 ng/mL.Conclusion The level of serum CTRP5 in ACS patients is increased and its level has a good predictive value for the degree of coronary artery disease especially for multivessel disease and myocardial fibrosis. -

-
表 1 对照组、UA亚组、NSTEMI亚组和STEMI亚组一般临床资料比较
Table 1. Comparison of baseline data among control group, UA subgroup, NSTEMI subgroup, and STEMI subgroup
例(%), X ± S, M(P25, P75) 项目 对照组(100例) UA亚组(79例) NSTEMI亚组(54例) STEMI亚组(77例) F/χ/H2 P 年龄/岁 58.04±9.85 59.48±10.13 60.81±9.22 59.86±11.29 0.980 0.398 男性 61(61.00) 56(67.09) 43(79.63) 58(75.32) 7.341 0.062 吸烟 35(35.00) 38(48.10) 33(61.11) 38(49.35) 6.582 0.086 BMI/(kg/m2) 26.22±3.08 26.22±3.02 26.16±2.85 26.00±3.61 0.086 0.968 高血压 56(56.00) 55(69.62) 41(75.93) 52(67.53) 7.344 0.062 糖尿病 13(13.00) 9(11.39) 11(20.37) 14(18.18) 2.921 0.404 TC/(mmol/L) 4.64±1.08 4.71±1.11 4.78±1.09 4.96±1.07 1.320 0.268 TG/(mmol/L) 1.58(1.09,2.42) 1.78(1.11,2.40) 1.72(1.11,2.45) 1.70(1.15,2.57) 2.797 0.424 LDL-C/(mmol/L) 2.56±0.95 2.68±0.96 2.72±0.88 2.74±0.74 0.732 0.534 FBG/(mmol/L) 6.13±2.21 6.31±2.41 6.96±2.22 8.27±3.84 10.189 < 0.001 HbA1c/% 5.2(4.4,5.7) 5.2(4.6,5.9) 5.1(4.6,6.1) 5.3(4.7,5.9) 0.945 0.815 BUN/(mmol/L) 5.65(4.90,6.61) 5.50(4.86,6.27) 6.19(4.71,6.70) 5.90(4.82,7.36) 3.551 0.314 SCr/(μmol/L) 69.02±12.11 69.49±13.47 70.29±17.22 73.54±17.51 1.532 0.206 NC/(×109/L) 3.58(2.73,4.66) 3.83(3.14,5.06) 5.47(3.91,7.03) 5.92(3.87,7.88) 53.371 < 0.001 LC/(×109/L) 1.57(1.32,1.93) 1.69(1.32,2.20) 1.60(1.10,1.95) 1.54(1.23,2.26) 1.854 0.603 PLT/(×109/L) 236.00(195.00,282.75) 230.00(193.00,266.00) 235.00(192.00,288.50) 246.50(189.50,289.75) 4.999 0.172 SII 494.64(367.50,749.50) 533.25(358.40,802.02) 789.84(552.21,1 164.45) 767.34(454.27,1 520.03) 28.218 < 0.001 hs-cTnI/(ng/mL) 0.03(0.02,0.23) 0.03(0.02,0.04) 1.55(0.52,6.88) 5.26(0.63,26.92) 205.882 < 0.001 CK-MB/(ng/mL) 4.24(1.36,8.60) 1.64(0.88,4.24) 35.68(14.85,80.25) 79.75(10.24,162.92) 169.539 < 0.001 NT-proBNP/(ng/L) 75.20(38.90,224.60) 131.50(58.60,217.50) 343.65(121.35,1233.60) 257.20(71.58,1261.05) 69.887 < 0.001 CTRP5/(ng/mL) 8.34±3.66 10.95±4.32 12.65±5.03 12.91±5.30 18.424 < 0.001 表 2 单支病变亚组、双支病变亚组与3支病变亚组患者CTRP5与SII水平比较
Table 2. Comparison of CTRP5 and SII levels among the single-vessel, double-vessel, and three-vessel disease groups
X ± S, M(P25, P75) 组别 CTRP5/(ng/mL) SII 单支病变亚组(57例) 9.67±4.17 620.10(440.59,935.34) 双支病变亚组(75例) 11.32±4.741) 790.28(523.16,1 254.28)1) 3支病变亚组(78例) 15.22±7.451)2) 894.24(694.88,1 318.40)1)2) F/H 16.990 24.678 P < 0.001 < 0.001 与单支病变亚组比较,1)P < 0.05;与双支病变亚组比较,2)P < 0.05。 表 3 低评分亚组、中评分亚组与高评分亚组患者CTRP5和SII水平比较
Table 3. Comparison of CTRP5 and SII levels among the low, middle, and high-score groups
X ± S, M(P25, P75) 组别 CTRP5/(ng/mL) SII 低评分亚组(74例) 10.22±4.32 559.24(393.60,986.23) 中评分亚组(86例) 12.47±6.89 699.85(524.38,1 141.81) 高评分亚组(50例) 13.97±8.921)2) 967.87(715.69,1 685.10)1)2) F/H 4.989 19.902 P 0.008 < 0.001 与低评分亚组比较,1)P < 0.05;与中评分亚组比较,2)P < 0.05。 表 4 LGE阳性组与LGE阴性组CTRP5和SII水平比较
Table 4. Comparison of CTRP5 and SII levels between LGE positive group and negative group
X ± S, M(P25, P75) 组别 CTRP5/(ng/mL) SII FBG/(mmol/L) LGE阴性组(26例) 9.19±2.25 641.83(438.39,945.72) 6.79±2.54 LGE阳性组(34例) 14.99±7.18 915.78(693.47,1 195.21) 7.53±2.25 t/Z 3.964 -2.193 0.988 P < 0.001 0.028 0.327 表 5 冠脉多支病变影响因素的logistic回归分析结果
Table 5. Multivariate logistic regression analysis for influencing factors of coronary artery multi-vessel disease
参数 B SE Wald χ2 P OR(95%CI) FBG 0.237 0.101 5.545 0.019 1.267(1.041~1.544) NC 0.061 0.108 0.326 0.568 1.063(0.861~1.313) hs-cTnI 0.015 0.011 1.844 0.175 0.985(0.963~1.007) CK-MB 0.002 0.003 0.588 0.443 1.002(0.997~1.008) NT-proBNP < 0.001 < 0.001 0.008 0.927 1.000(0.998~1.014) SII 0.001 0.001 4.041 0.044 1.001(1.000~1.002) CTRP5 0.119 0.043 7.716 0.005 1.127(1.036~1.226) 常数项 -3.228 0.862 14.015 < 0.001 表 6 FBG、SII和CTRP5预测冠脉多支病变的ROC分析结果
Table 6. ROC results for predicting multi-vessel coronary artery disease using FBG, SII, and CTRP5
指标 AUC 95%CI 截断值 灵敏度/% 特异度/% P FBG 0.627 0.546~0.708 6.28 mmol/L 55.6 68.4 < 0.001 SII 0.695 0.619~0.772 632.14 77.1 52.6 < 0.001 CTRP5 0.708 0.628~0.788 10.31 ng/mL 81.4 78.9 < 0.001 表 7 SII和CTRP5预测心肌纤维化的ROC分析结果
Table 7. ROC results for predicting myocardial fibrosis using SII and CTRP5
指标 AUC 95%CI 截断值 灵敏度/% 特异度/% P SII 0.655 0.514~0.796 673.05 76.5 53.8 0.041 CTRP5 0.775 0.656~0.895 11.10 ng/mL 64.7 92.3 < 0.001 -
[1] Frangogiannis NG. Cardiac fibrosis[J]. Cardiovasc Res, 2021, 117(6): 1450-1488. doi: 10.1093/cvr/cvaa324
[2] Yin XY, Yin XX, Pan X, et al. Post-myocardial infarction fibrosis: pathophysiology, examination, and intervention[J]. Front Pharmacol, 2023, 14(3): 1070973.
[3] Cederström S, Lundman P, Alfredsson J, et al. Association between high-sensitivity C-reactive protein and coronary atherosclerosis in a general middle-aged population[J]. Sci Rep, 2023, 13(1): 12171. doi: 10.1038/s41598-023-39051-3
[4] Li CY, Ying SZ, Wu XL, et al. CTRP1 aggravates cardiac fibrosis by regulating the NOX2/P38 pathway in macrophages[J]. Cell J, 2022, 24(12): 732-740.
[5] Li CY, Ying SZ, Wu XL, et al. CTRP1 aggravates cardiac fibrosis by regulating the NOX2/P38 pathway in macrophages[J]. Cell J, 2022, 24(12): 732-740.
[6] 中国医师协会急诊医师分会, 国家卫健委能力建设与继续教育中心急诊学专家委员会, 中国医疗保健国际交流促进会急诊急救分会. 急性冠脉综合征急诊快速诊治指南(2019)[J]. 临床急诊杂志, 2019, 20(4): 253-262.
[7] Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease[J]. Am J Cardiol, 1983, 51(3): 606. doi: 10.1016/S0002-9149(83)80105-2
[8] Bemelli C, Campo G, Pasquale GD, et al. Percutaneous revascularization in non-ST-elevation acute coronary syndromes: complete or incomplete?[J]. G Ital Cardiol(Rome), 2024, 25(1): 26-35.
[9] Luo JY, He ZW, Li QW, et al. Adipokines in atherosclerosis: unraveling complex roles[J]. Front Cardiovasc Med, 2023, 10(8): 1235953.
[10] 王康, 智丽霞, 石姣姣, 等. 冠心病患者血浆白脂素和分泌型卷曲相关蛋白5与冠状动脉病变程度的相关性[J]. 临床心血管病杂志, 2022, 38(6): 455-460. doi: 10.13201/j.issn.1001-1439.2022.06.006
[11] 周琦, 柯玲, 阮科, 等. 系统炎症因子预测老年冠心病PCI术后主要不良心脑血管事件的价值[J]. 临床心血管病杂志, 2022, 38(2): 118-123. doi: 10.13201/j.issn.1001-1439.2022.02.008
[12] Peng M, Liu Y, Zhang XQ, et al. CTRP5-overexpression attenuated ischemia-reperfusion associated heart injuries and improved infarction induced heart failure[J]. Front Pharmacol, 2020, 11(12): 603322.
[13] Libby P. The changing landscape of atherosclerosis[J]. Nature, 2021, 592(7855): 524-533. doi: 10.1038/s41586-021-03392-8
[14] Xie XL, Meng ZJ, Gao J, et al. C1q complement/tumor necrosis factor-associated proteins in cardiovascular disease and COVID-19[J]. Proteomes, 2021, 9(1): 12. doi: 10.3390/proteomes9010012
[15] Guo SN, Mao XH, Liu J, et al. Multi-faceted roles of C1q/TNF-related proteins family in atherosclerosis[J]. Front Immunol, 2023, 14(10): 1253433.
[16] Zhang Y, Liu C, Liu J, et al. Implications of C1q/TNF-related protein superfamily in patients with coronary artery disease[J]. Sci Rep, 2020, 10(1): 878. doi: 10.1038/s41598-020-57877-z
[17] Liu YX, Chen W, Ding ZJ, et al. Role of serum C1q/TNF-related protein family levels in patients with acute coronary syndrome[J]. Front Cardiovasc Med, 2022, 9(8): 967918.
[18] Tudurachi BS, Anghel L, Tudurachi A, et al. Assessment of inflammatory hematological ratios(NLR, PLR, MLR, LMR and monocyte/HDL-cholesterol ratio)in acute myocardial infarction and particularities in young patients[J]. Int J Mol Sci, 2023, 2(18): 14378.
[19] Xie F, Yu ZZ, Xiong YR, et al. Systemic immune-inflammation index and in-stent restenosis in patients with acute coronary syndrome: a single-center retrospective study[J]. Eur J Med Res, 2024, 29(1): 145. doi: 10.1186/s40001-024-01736-4
[20] Altunova M, Karakayalı M, Kahraman S, et al. Systemic immune-inflammatory index is associated with residual SYNTAX Score in patients with ST-segment elevation myocardial infarction[J]. Anatol J Cardiol, 2023, 27(8): 472-478.
[21] Wei X, Zhang ZP, Wei J, et al. Association of systemic immune inflammation index and system inflammation response index with clinical risk of acute myocardial infarction[J]. Front Cardiovasc Med, 2023, 10(8): 1248655.
[22] Babapour B, Piralaei K, Doustkami H, et al. Correlation of serum adipolin with epicardial fat thickness and severity of coronary artery diseases in acute myocardial infarction and stable angina pectoris patients[J]. Med Princ Pract, 2021, 30(1): 52-61. doi: 10.1159/000508834
[23] Ho AB, Tran QB. The role of N-terminal pro-B-type natriuretic peptide(NT-proBNP)and high-sensitivity troponin T(hs-troponin T)in the evaluation of the syntax score in patients with acute coronary syndrome[J]. Cureus, 2024, 16(3): e55653.
[24] Zhang H, Zhang-sun ZY, Xue CX, et al. CTRP family in diseases associated with inflammation and metabolism: molecular mechanisms and clinical implication[J]. Acta Pharmacol Sin, 2023, 44(4): 710-725.
[25] Zhao Q, Zhang CL, Xiang RL, et al. CTRP15 derived from cardiac myocytes attenuates TGFβ1-induced fibrotic response in cardiac fibroblasts[J]. Cardiovasc Drugs Ther, 2020, 34(5): 591-604.
[26] Chen L, Duan HZ, Zhang C, et al. Serum complement C1q level is associated with left ventricular hypertrophy induced by coarctation of the aorta: a retrospective observational study[J]. BMC Cardiovasc Disord, 2022, 22(1): 367.
[27] Antar SA, Ashour NA, Marawan ME, et al. Fibrosis: types, effects, markers, mechanisms for disease progression, and its relation with oxidative stress, immunity, and inflammation[J]. Int J Mol Sci, 2023, 24(4): 4004. doi: 10.3390/ijms24044004
[28] Maruyama K, Yoshida KI. The pathogenesis of cardiac fibrosis: a review of recent progress[J]. Int J Mol Sci, 2022, 23(5): 2617.
-




 下载:
下载: