Transesophageal echocardiography evaluates the residual mitral regurgitation and its influencing factors in patients with HOCM after myocardial resection
-
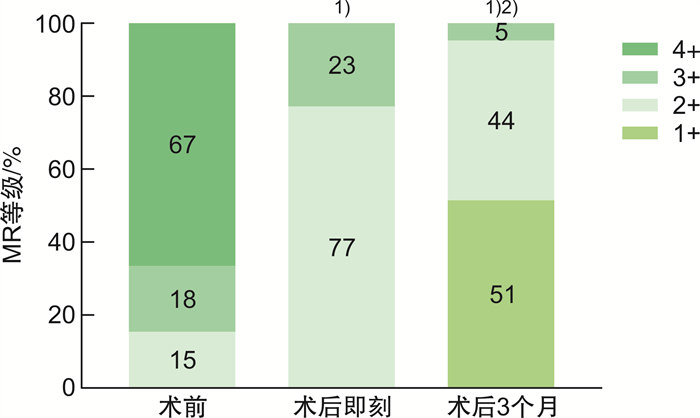
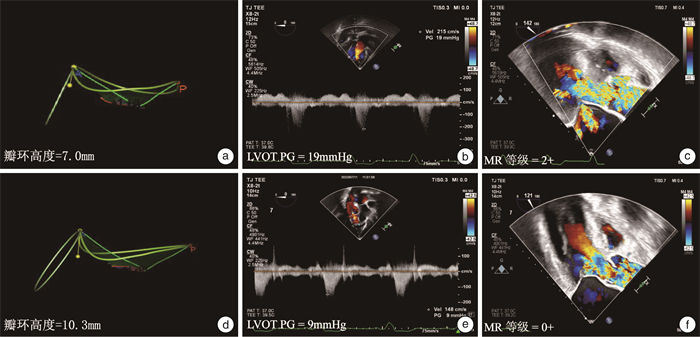
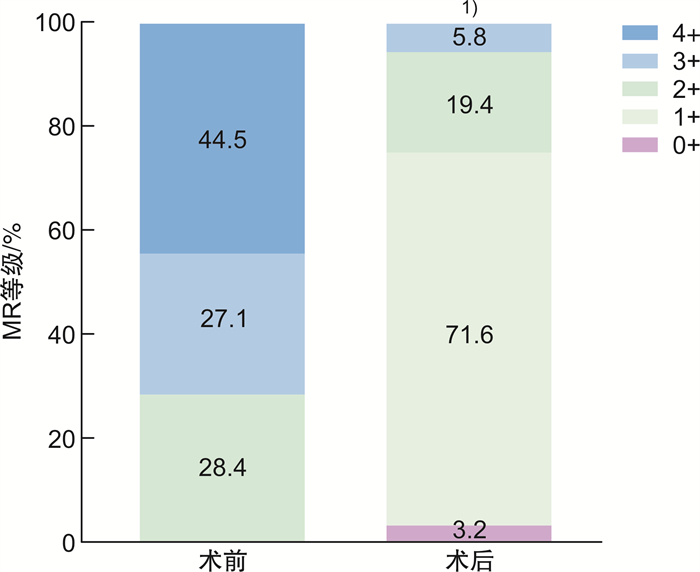
摘要: 目的 评估肥厚型梗阻性心肌病(HOCM)患者经心尖不停跳室间隔心肌切除(TA-BSM)术后残余二尖瓣反流(MR)及其影响因素,随访其术后转归,为临床处置决策提供客观依据。方法 前瞻性纳入2023年5月—2023年12月在我院确诊为HOCM且接受TA-BSM的患者155例,术中全程采用经食管超声心动图(TEE)实时监测与导航,在心肌切除术前、术后:①评估最大室间隔厚度、左室流出道峰值压差(LVOT-PG)、SAM等级、MR程度;②测量二尖瓣(MV)二维结构特征,包括前、后叶长度、残余瓣叶长度、前后叶对合高度;③获取MV三维(3D)容积图像,采用Tomtec工作站分析瓣叶面积、帐篷高度、帐篷面积、帐篷容积以及瓣环内径、周长、面积与高度。以心肌切除术后即刻是否仍存在MR≥2+分为残余组与无残余组,比较两组间术前MV各结构参数有无差异。采用单因素及多因素二元logistic回归探讨影响心肌切除术后残余MR的MV结构特征指标。术后3个月采用经胸超声心动图(TTE)随访梗阻和MR改善情况。结果 TA-BSM术中,与心肌切除前相比,心肌切除术后前、后室间隔基底段及中间段室壁厚度均显著减小(均P < 0.01),LVOT-PG明显降低(P < 0 01);术后即刻MR≥3+的患者由111例(71.6%)减少至9例(5.8%)(均P < 0 01);术后即刻MR≥2+的残余组患者39例(25.2%),无残余组116例(74.8%)。经过两组间比较、单因素分析和多因素二元logistic回归分析显示,年龄、MV钙化、MV增厚≥5 mm、MV环高度 < 10.0 mm是术后即刻残余MR反流的独立影响因素(均P < 0.05)。术后3个月随访,51%的残余组患者MR程度改善至2+以下(P < 0.01)。结论 TA-BSM单纯心肌切除能够有效改善HOCM相关性MR,年龄、MV钙化或增厚以及瓣环高度是影响术后即刻残余MR≥2+的主要因素,51%的术中残余反流能够在随访中得以改善,不需要术中手术处理。Abstract: Objective To evaluate the residual mitral regurgitation(MR) and its influencing factors in patients with hypertrophic obstructive cardiomyopathy(HOCM) after transapical Beating-Heart Septal Myectomy(TA-BSM), and to follow up the postoperative outcome, so as to provide an objective basis for clinical management decisions.Methods A total of 155 patients diagnosed with HOCM and receiving TA-BSM in our hospital from May 2023 to December 2023 were prospectively enrolled. Transesophageal echocardiography(TEE) was used for real-time monitoring and navigation throughout the operation. 1) The maximum ventricular septal thickness, left ventricular outflow tract peak pressure difference(LVOT-PG), SAM grade and MR Degree were evaluated. 2) The two-dimensional structural characteristics of the mitral valve(MV) were measured, including the length of the anterior and posterior leaflets, the length of the residual leaflets, and the involutional height of the anterior and posterior leaflets. 3) Three-dimensional(3D) MV volume images were obtained, and Tomtec workstation was used to analyze the valve leaf area, tent height, tent area, tent volume, and inner diameter, perimeter, area and height of the valve ring. According to whether there was MR≥2+ immediately after myectomy, the patients were divided into residual group and non-residual group, and the differences of MV structural parameters between the two groups were compared. Univariate and multivariate binary logistic regression were used to explore the structural characteristics of MV that affected residual MR After myocardial resection. Transthoracic echocardiography(TTE) was used to follow up obstruction and MR Improvement 3 months after operation.Results During TA-BSM, the wall thickness of the basal and middle segments of the anterior and posterior ventricular septum was significantly decreased(all P < 0.01), and the LVOT-PG was significantly decreased(P < 0.01). The number of patients with MR≥3+ immediately after surgery decreased from 111 cases(71.6%) to 9 cases(5.8%)(all P < 0.01). There were 39 patients(25.2%) in residual group and 116 patients(74.8%) in non-residual group with MR≥2+ immediately after operation. Univariate analysis and multivariate binary Logistic regression analysis showed that age, MV calcification, MV thickening ≥5 mm and MV ring height < 10.0 mm were independent influencing factors of postoperative residual MR Reflux(all P < 0.05). At the follow-up of 3 months after operation, 51% of the residual group had MR Degree improved to less than 2+(P < 0.01).Conclusion Age, MV calcification or thickening, and annulus height are the main factors affecting the immediate postoperative residual MR≥2+. The 51% of intraoperative residual reflux can be improved during follow-up, and intraoperative surgical treatment is not required.
-

-
表 1 研究人群基线临床资料
Table 1. General data
例(%), X±S, M(P25, P75) 项目 数值 男性 101(65.2) 年龄/岁 50±13 体表面积/m2 1.8±0.2 NYHA分级 Ⅰ级 0 Ⅱ级 101(65.2) Ⅲ~Ⅳ级 54(34.8) 糖尿病 10(6.5) 高血压 40(25.8) 冠心病 17(11.0) NT-proBNP/(pg/mL) 961.7(352.4,1 910.0) cTnI/(pg/mL) 17.3(7.4,69.4) β-受体阻滞剂 96(61.9) 钙通道阻滞剂 29(18.7) 酒精消融术 4(2.6) 射频消融术 2(1.3) 表 2 TA-BSM术后即刻残余组与无残余组术前术后各参数比较
Table 2. TA-BSM parameters post operation
例(%), X±S, M(P25, P75) 参数 残余组(39例) 无残余组(116例) P 女性 17(43.6) 37(31.9) 0.185 年龄/岁 60(52,67) 45(38,58) <0.001 体表面积/m2 1.8±0.2 1.8±0.2 0.540 NYHA分级≥Ⅲ 20(51.3) 40(34.5) 0.062 心房颤动 3(7.7) 2(1.7) 0.193 高血压 15(38.5) 27(23.3) 0.065 糖尿病 2(5.1) 8(6.9) 0.990 冠心病 6(15.4) 11(9.5) 0.308 术前 最大室间隔厚度/mm 20.0(17.0,23.0) 22.0(19.0,26.0) 0.070 LVOT-PG/mmHg 79.0(62.0,103.0) 78.0(64.0,100.0) 0.817 SAM等级≥2 38(97.4) 116(100.0) 0.566 MR等级≥2 39(100.0) 116(100.0) 1.000 LAD/mm 45(41,50) 41(38,47) 0.008 左心室舒张末期直径/mm 46.0(43.0,48.0) 45.0(42.0,48.0) 0.355 左心室射血分数/% 71.0(66.0,75.0) 73.0(68.0,75.8) 0.150 LAVi max/(mL/m2) 45.6(39.4,65.8) 43.1(35.8,53.2) 0.035 左心室收缩末期容积指数/(mL/m2) 10.7(8.3,16.8) 13.7(10.3,18.8) 0.106 左心室舒张末期容积指数/(mL/m2) 54.5±12.0 55.6±13.6 0.664 E/e’ 16.3(13.6,20.9) 13.8(10.8,17.5) 0.027 二尖瓣钙化 20(51.3) 24(20.7) <0.001 二尖瓣瓣叶厚度≥5mm 10(25.6) 8(6.9) 0.002 术后 LVOT-PG/mmHg 13.0(10.0,20.0) 11.5(8.0,16.8) 0.064 SAM等级≥2 4(10.3) 9(7.8) 0.878 切缘长度/mm 33.0(29.0,40.0) 38.0(31.0,41.0) 0.177 切缘宽度/mm 37.0(30.0,40.0) 38.0(28.3,45.0) 0.521 切缘厚度/mm 7.0(6.0,8.0) 8.0(7.0,9.0) 0.143 切缘角度/° 101.1(89.0,118.5) 105.9(89.1,117.0) 0.797 切除刀数/刀 6(4,7) 5(4,7) 0.820 切除的心肌重量/g 3.9(2.7,5.5) 4.6(3.2,6.0) 0.271 表 3 TA-BSM术后即刻残余组与无残余组二尖瓣结构的比较
Table 3. Mitral valve structure after TA-BSM surgery
例(%), X±S, M(P25, P75) 参数 残余组(39例) 无残余组(116例) 术前 术后 术前 术后 二尖瓣叶 前叶长度/mm 30.0(26.0,34.0) 30(25.0,34.0) 后叶长度/mm 15.0(15.0,20.0) 18.0(16.0,20.0)2) 残余瓣叶长度/mm 9.0(7.0,11.0) 9.0(6.0,10.0)1) 10.0(7.0,13.0) 8.0(6.0,10.0)1) 前后叶对合高度/mm 4.0(4.0,5.0) 7.0(6.0,8.0)1) 5.5(4.0,7.0)2) 8.0(7.0,9.0)1)3) 前叶面积/cm2 8.5(7.4,9.4) 8.7(7.8,9.7) 后叶面积/cm2 6.8(6.0,8.0) 6.9(6.0,7.9) 帐篷高度/mm 7.1(4.1,9.2) 7.0(4.0,10.0) 6.1(4.5,9.3) 5.4(3.2,8.6)1)3) 帐篷面积/cm2 1.0(0.5,1.6) 0.8(0.4,1.3)1) 1.0(0.5,1.5) 0.7(0.4,1.0)1) 帐篷容积/mL 1.8(1.3,2.7) 1.5(0.9,2.3)1) 1.8(1.2,2.7) 1.5(1.0,2.5)1) 二尖瓣环 前-后径/mm 38.3±4.2 36.7±3.21) 36.1±4.02) 34.5±3.51)3) 前外-后内侧间径/mm 38.5(36.5,40.6) 36.0(33.6,38.0)1) 35.3(32.1,38.1)2) 34.2(30.8,37.5)1)3) 周长/mm 126.8(119.6,137.0) 122.5(119.5,131.0)1) 122.4(113.0,129.2)2) 118.1(110.1,129.1)1)3) 面积/mm2 1 212.0
(1 111.0,1 331.0)1 121.0
(1 032.0,1 261.0)1)1 073.5.0
(949.8,1 192.0)2)1 010.0
(899.3,1 166.8)1)3)高度/mm 8.4±1.7 9.6(8.0,10.9)1) 10.9±2.12) 11.3(10.1,12.8)1)3) 与同组术前比较,1)P < 0.05;与残余组术前比较,2)P < 0.05;与残余组术后比较,3)P < 0.05。 表 4 TA-BSM术后即刻产生MR≥2+影响因素的单因素和多因素二元logistic回归分析
Table 4. Single factor and multiple factor binary logistic regression analysis
变量 单因素分析 多因素分析 P OR 95%CI P OR 95%CI 年龄 <0.001 1.077 1.040~1.115 0.018 1.082 1.014~1.155 LAD 0.007 1.081 1.021~1.145 LAVi max 0.040 1.024 1.001~1.047 E/e’ 0.098 1.048 0.992~1.107 二尖瓣钙化 <0.001 4.498 2.060~9.820 0.040 4.353 1.069~17.722 二尖瓣瓣叶厚度≥5 mm 0.008 4.050 1.439~11.398 0.022 7.699 1.336~44.368 术前 后叶长度 0.022 0.859 0.755~0.978 前后叶对合高度 0.017 0.777 0.632~0.955 前-后径 0.005 1.144 1.042~1.256 前外-后内侧间径 <0.001 1.222 1.111~1.343 周长 0.001 1.052 1.020~1.084 面积 <0.001 1.003 1.002~1.005 高度 <0.001 0.516 0.402~0.661 <0.001 0.487 0.341~0.696 -
[1] 国家心血管病中心心肌病专科联盟. 中国成人肥厚型心肌病诊断与治疗指南2023[J]. 中国循环杂志, 2023, 38(1): 1-33.
[2] 朱英, 汪慧, 周玮, 等. 经食管三维超声心动图导航经心尖不停跳室间隔切除术治疗肥厚型梗阻性心肌病[J]. 中华超声影像学杂志, 2023, 32(12): 1030-1038.
[3] Panza JA, Maris TJ, Maron BJ. Development and determinants of dynamic obstruction to left ventricular outflow in young patients with hypertrophic cardiomyopathy[J]. Circulation, 1992, 85(4): 1398-1405. doi: 10.1161/01.CIR.85.4.1398
[4] Bonow RO, O'Gara PT, Adams DH, et al. 2020 focused update of the 2017 ACC expert consensus decision pathway on the management of mitral regurgitation: a report of the American college of cardiology solution set oversight committee[J]. J Am Coll Cardiol, 2020, 75(17): 2236-2270. doi: 10.1016/j.jacc.2020.02.005
[5] Nagueh SF, Phelan D, Abraham T, et al. Recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: an update from the American society of echocardiography, in collaboration with the American society of nuclear cardiology, the society for cardiovascular magnetic resonance, and the society of cardiovascular computed tomography[J]. J Am Soc Echocardiogr, 2022, 35(6): 533-569. doi: 10.1016/j.echo.2022.03.012
[6] Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American society of echocardiography and the society of cardiovascular anesthesiologists[J]. J Am Soc Echocardiogr, 2013, 26(9): 921-964. doi: 10.1016/j.echo.2013.07.009
[7] Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation A report from the American society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance[J]. J Am Soc Echocardiogr, 2017, 30(4): 303-371. doi: 10.1016/j.echo.2017.01.007
[8] Hong JH, Schaff HV, Nishimura RA, et al. Mitral regurgitation in patients with hypertrophic obstructive cardiomyopathy: implications for concomitant valve procedures [J]. J Am Coll Cardiol, 2016, 68(14): 1497-1504. doi: 10.1016/j.jacc.2016.07.735
[9] Sun DK, Schaff HV, Nishimura RA, et al. Transapical septal myectomy for hypertrophic cardiomyopathy with midventricular obstruction[J]. Ann Thorac Surg, 2021, 111(3): 836-844. doi: 10.1016/j.athoracsur.2020.05.182
[10] Sherrid MV, Balaram S, Kim B, et al. The mitral valve in obstructive hypertrophic cardiomyopathy: a test in context [J]. J Am Coll Cardiol, 2016, 67(15): 1846-1858. doi: 10.1016/j.jacc.2016.01.071
[11] 于子翔, 程琦, 李晓梅, 等. 新疆地区二尖瓣反流发病情况和临床特征: 单中心10年超声资料分析[J]. 临床心血管病杂志, 2024, 40(4): 329-334. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2024.04.015
[12] Pressman GS, Movva R, Topilsky Y, et al. Mitral annular dynamics in mitral annular calcification: a three-dimensional imaging study[J]. J Am Soc Echocardiogr, 2015, 28(7): 786-794. doi: 10.1016/j.echo.2015.03.002
-




 下载:
下载: