Evaluation of mitral annulus changes in patients with atrial fibrillation by automated software 4D-MVA with three-dimensional transesophageal echocardiography
-
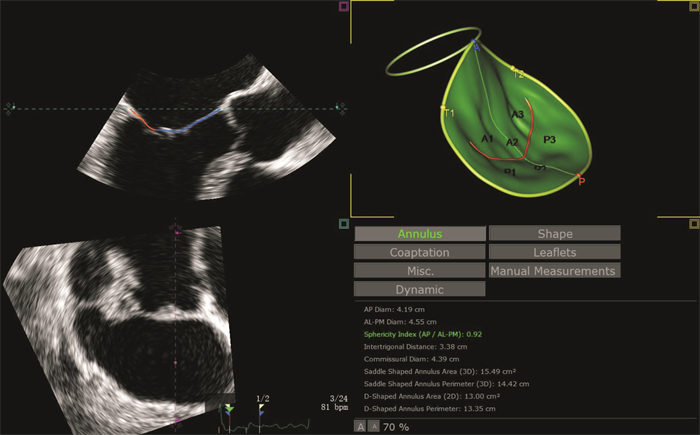
摘要: 目的 通过三维经食管超声(3D-TEE)二尖瓣自动定量技术(4D-MVA)评价心房颤动(AF)患者二尖瓣环的变化。方法 前瞻性纳入AF患者61例,其中轻度及中度二尖瓣反流AF患者24例(AFMR+组)、无二尖瓣反流AF患者(AFMR-组)37例,对照组24例,均行3D-TEE检查,并采用4D-MVA获取二尖瓣环系列参数,进行比较分析。结果 与对照组比较,AF患者二尖瓣环前后径(AP)、瓣环面积(AA)更大,瓣环高度(AH)更低,瓣环圆度(AS)更圆,非平面角度(NPA)更大(均P < 0.05);在AF患者中,AFMR+组舒张末期AS更接近1,收缩末期和舒张末期AA更大,AH更低(均P < 0.05)。此外,AFMR+组AP、AS、AH和AA收缩期变化率较对照组及AFMR—组均减小(P < 0.05),而AFMR—组与对照组AP、AS、AH、AA收缩期变化率无显著差异。结论 AF患者二尖瓣环扩大,趋向圆形、平坦,且合并二尖瓣反流的AF患者二尖瓣环变化更显著,随心动周期动态变化也更显著。
-
关键词:
- 二尖瓣 /
- 自动定量 /
- 心房颤动 /
- 经食管三维超声心动图
Abstract: Objective To evaluate the mitral annulus changes in atrial fibrillation(AF) patients through automated 4D-MVA software with three-dimensional transesophageal echocardiography(3D-TEE).Methods We prospectively enrolled 24 AF patients with mild or moderate mitral regurgitation as AFMR + group, 37 AF patients without mitral regurgitation as AFMR-group, and 37 cases as control group. 3D-TEE was performed to obtain mitral apparatus parameters by 4D-MVA software for analysis.Results The anterior to posterior diameter(AP) and area(AA) of mitral annulus were larger in AFMR-group and AFMR + group, the height of mitral annulus(AH) was lower, the sphericity of mitral annulus(AS) was rounder, and the nonplanarity angle(NPA) was larger, the differences were statistically significant(all P < 0.05). Between the two AF groups, the end-diastolic AS in AFMR + group was rounder, the end-systolic and end-diastolic AA was higher, and the AH was lower, with statistical significance(all P < 0.05). The systolic change rates of AP, AS, AH and AA in AFMR + group were lower than those in control group and AFMR-group(all P < 0.05), but there was no significant difference between control group and AFMR-group.Conclusion In AF patients, the mitral annulus was enlarged and tended to be round and flat. The remodeling of the mitral annulus in patients with AFMR + was more significant than that in patients with AFMR-. Patients with AFMR + had more damage to the dynamic changes of the mitral annulus throughout cardiac cycle. -

-
表 1 各组间一般参数比较
Table 1. General data
例(%), X±S 变量 对照组(24例) AFMR-组(37例) AFMR+组(24例) P值 年龄/岁 62.0±5.3 62.3±7.4 58.5±10.5 0.161 男/(例(%) 11(45) 17(46) 19(79)1)2) < 0.001 BSA/m2 1.62±0.14 1.77±0.171) 1.87±0.171) < 0.001 心率/(次/min) 69±10 72±11 75±12 0.126 收缩压/mmHg△ 117±9 153±241) 147±281) < 0.001 舒张压/mmHg 76.0±7.1 92.0±13.61) 92.0±13.61) < 0.001 持续性AF/% 4(11) 19(79) < 0.001 左心房内径/mm 33.3±3.0 38.1±3.01) 44.4±3.31)2) < 0.001 左心室舒张末容积/mL 79.8±12.5 83.8±15.7 102.9±22.51)2) < 0.001 左心室收缩末容积/mL 28.4±5.8 31.2±8.2 43.1±15.91)2) < 0.001 左心室射血分数/% 64.5±4.2 63.1±4.2 59.0±7.21)2) < 0.001 △1 mmHg=0.133 kPa。与对照组比较,1)P < 0.05;与AFMR-组比较,2)P < 0.05。 表 2 各组二尖瓣环参数比较
Table 2. Comparison of mitral annulus parameters
X±S 二尖瓣环参数 舒张末期 收缩末期 对照组(24例) AFMR-组(37例) AFMR+组(24例) P值 对照组(24例) AFMR-组(37例) AFMR+组(24例) P值 AP/(cm/m2) 2.0±0.2 2.1±0.2 2.1±0.3 0.051 1.8±0.2 2.0±0.21) 2.0±0.21) 0.007 AL-PM/(cm/m2) 2.2±0.2 2.2±0.2 2.2±0.2 0.773 2.0±0.2 2.1±0.2 2.1±0.3 0.673 AS 0.90±0.04 0.95±0.181) 0.96±0.231)2) < 0.001 0.90±0.05 0.95±0.021) 0.96±0.031) < 0.001 AH/(mm/m2) 5.6±0.7 4.6±0.81) 3.4±0.81)2) < 0.001 5.8±.8 4.9±0.91) 3.6±0.81)2) < 0.001 AC/(cm/m2) 6.6±0.7 6.9±0.9 6.5±0.8 0.217 6.3±0.8 6.7±0.8 6.4±0.8 0.219 AA/(cm2/m2) 5.1±0.7 5.7±1.11) 6.3±0.91)2) < 0.001 4.8±0.7 5.4±1.01) 6.1±0.91)2) < 0.001 NPA 139±10 146±101) 150±91) 0.001 135±27 147±91) 152±91) 0.001 与对照组比较,1)P < 0.05;与AFMR-组比较,2)P < 0.05。 表 3 各组二尖瓣环动态参数比较
Table 3. Dynamic parameters of mitral annulus among different groups
%, M(P25, P75) 参数 对照组(24例) AFMR-组(37例) AFMR+组(24例) P值 AP收缩期变化率 6.8(4.5,9.2) 4.8(3.6,6.6) 4.8(2.7,5.7)1) 0.008 AS收缩期变化率 3.1(1.3,5.3) 1.5(0.7,3.2) 1.2(0.6,2.5)1) 0.035 AH收缩期变化率 5.3(2.2,9.6) 6.7(4.0,10.0) 2.0(0.1,6.5)1) 0.004 AA收缩期变化率 5.3(4.0,6.2) 4.9(3.4,6.0) 3.7(2.5,0.4)1) 0.026 与对照组比较,1)P < 0.05。 -
[1] 中华医学会老年医学分会心血管学组, 中国老年保健医学研究会老年心血管病分会. 老年心房颤动诊治中国专家共识(2024)[J]. 中华心律失常学杂志, 2024, 28(2): 103-124.
[2] 王华, 刘宇佳, 杨杰孚. 心力衰竭流行病学[J]. 临床心血管病杂志, 2023, 39(4): 243-247. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.04.001
[3] Gertz ZM, Raina A, Saghy L, et al. Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control[J]. J Am Coll Cardiol, 2011, 58(14): 1474-1481. doi: 10.1016/j.jacc.2011.06.032
[4] Unger P, Galloo X. Atrial functional mitral regurgitation: an electro-mechanical interplay[J]. Eur Heart J Cardiovasc Imaging, 2023, 24(11): 1458-1459. doi: 10.1093/ehjci/jead225
[5] Kagiyama N, Mondillo S, Yoshida K, et al. Subtypes of atrial functional mitral regurgitation: imaging insights into their mechanisms and therapeutic implications[J]. JACC Cardiovasc Imaging, 2020, 13(3): 820-835. doi: 10.1016/j.jcmg.2019.01.040
[6] Chen TE, Ong K, Suri RM, et al. Three-dimensional echocardiographic assessment of mitral annular physiology in patients with degenerative mitral valve regurgitation undergoing surgical repair: comparison between early-and late-stage severe mitral regurgitation[J]. J Am Soc Echocardiogr, 2018, 31(11): 1178-1189. doi: 10.1016/j.echo.2018.07.005
[7] 中华医学会心血管病学分会心血管影像学组, 北京医学会心血管病学会影像学组. 中国成人心脏瓣膜病超声心动图规范化检查专家共识[J]. 中国循环杂志, 2021, 36(2): 109-125.
[8] 中华医学会心血管病学分会, 中国生物医学工程学会心律分会. 心房颤动诊断和治疗中国指南[J]. 中华心血管病杂志, 2023, 51(6): 572-618.
[9] Buckberg G, Hoffman JI, Mahajan A, et al. Cardiac mechanics revisited: the relationship of cardiac architecture to ventricular function[J]. Circulation, 2008, 118(24): 2571-2587. doi: 10.1161/CIRCULATIONAHA.107.754424
[10] Meucci MC, Stassen J, Tomsic A, et al. Prognostic impact of left ventricular global longitudinal strain in atrial mitral regurgitation[J]. Heart, 2023, 109(6): 478-484. doi: 10.1136/heartjnl-2022-321698
[11] Iwasaki YK, Nishida K, Kato T, et al. Atrial fibrillation pathophysiology: implications for management[J]. Circulation, 2011, 124(20): 2264-2274. doi: 10.1161/CIRCULATIONAHA.111.019893
[12] Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines[J]. Circulation, 2021, 143(5): e72-e227.
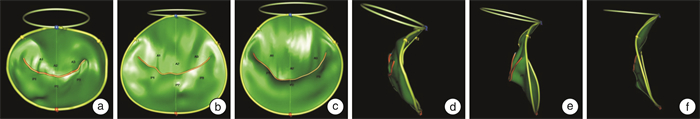
[13] 潘翠珍, 潘文志, 李伟, 等. 二尖瓣解剖结构及反流的超声心动图新评价[J]. 中华超声影像学杂志, 2020, 29(12): 1095-1099.
-




 下载:
下载: